 |
 |
| J Korean Acad Pediatr Dent > Volume 46(1); 2019 > Article |
|
ģ“ė”
ģė©“ķøķ”ģ„ģ ė źµ¬ź°ģ
ģė©“ ź·¼ģ” źø°ė„ė¶ģ ģ ģ ė°ķģ¬ ģėŖØģ ķķģ“ģ ė° ė¶ģ źµķ©ģ ģ ė°ķ ģ ģė¤. ģģģ¹ź³¼ ģģģģ ģė©“ķøķ”ģ„ģ ģ ģ”°źø° ģ§ėØź³¼ ģ¹ė£ė ģ“ė¬ķ ķ©ė³ģ¦ģ ģ°ØėØķģ¬ ģ ģģ ģø ģėŖØ ģ±ģ„ģ ģ ģ§ķ ģ ģė¤ė ģ ģģ ģ¤ģķė¤. ģė©“ķøķ”ģ„ģ ģ ģ¹ė£ė² ģ¤ģ ķėė” ź·¼źø°ė„ģė²ģ“ ģģ¼ė©° źø°ģ± ź·¼źø°ė„ ģ„ģ¹ź° ė³“ģ”°ģ ģ¼ė” ģ¬ģ©ė ģ ģė¤. ė³ø ģ¦ė”ė¤ģģė ģė©“ķøķ”ģ„ģ ź° ģė ė¶ģ źµķ© ķģė¤ģź² źø°ģ± ź·¼źø°ė„ ģ„ģ¹ė„¼ ģ¬ģ©ķģ¬ ģė©“ķøķ”ģ„ģ ė„¼ ķ“ģķė ź²°ź³¼ė„¼ ģ»ģźø°ģ ė³“ź³ ķė ė°ģ“ė¤. ķģ§ė§ ģ“ģģ ź°ģ ķØź³¼ė ź·ø ģ ėģ ė°ė¼ ģ°Øģ“ź° ė°ģķ ģ ģģ¼ėÆė” ģ“ģ ėķ ķź³ģ ģ ź³ ė ¤ķ ķģź° ģė¤.
Abstract
Sleep-disordered breathing (SDB) induces dysfunction of the orofacial muscles, leading to morphologic alteration of the face and dental malalignment. Early diagnosis and treatment of SDB is required in pediatric patients to ensure normal facial growth. Myofunctional therapy (MFT) is a modality for the treatment of SDB and prefabricated appliances can be used. Herein 2 cases of malocclusion with SDB, in which MFT with a prefabricated appliance was used for orthodontic treatment, have been described. SDB was diagnosed based on clinical symptoms taken by interview and home respiratory polygraphy. In both cases, SDB was improved using prefabricated appliance for MFT. However, resolution of crowding depended on the degree of crowding.
Sleep-disordered breathing (SDB) encompasses a wide range of respiratory disorders specific to sleep or exacerbated by sleep ranging from habitual snoring to obstructive sleep apnea[1]. SDB is common in children as well as adults, with prevalence rate of 3 - 35% for snoring and 1.2 - 5.7% for obstructive sleep apnea[2-4]. Even though most pediatric obstructive sleep disorders are mild to moderate compared to adult type, untreated pediatric SDB can have adverse effects on cardiovascular, metabolic, and neurobehavioral development that contribute directly to reduced quality of life[5-8].
According to the international classification of sleep disorders, pediatric obstructive sleep apnea was defined as an apnea-hypopnea index (AHI) ā„ 1.0 or a pattern of obstructive hypoventilation defined as at least 25% of total sleep time with hypercapnia (PaCO2 > 50 mmHg) in association with snoring, flattening of the nasal pressure waveform, or paradoxical respiratory efforts[9].
Early recognition and treatment of SDB is required in children, in order to achieve maximal resolution of symptoms and prevention of SDB in adulthood. It has been established that adenotonsillectomy can result in substantial improvement of SDB in children in which the condition is related to adenoid or tonsillar hypertrophy[10]. However, some patients continue to exhibit abnormal breathing and other symptoms during sleep after surgery[11]. Therefore, it is necessary to investigate other modes of treatment for SDB.
Myofunctional therapy (MFT) has been proposed as a multidisciplinary SDB treatment[10,12]. The therapy aims to correct tongue position and improve functions of orofacial muscles in order to facilitate better nasal breathing and lip competence. However, it is difficult for young children to follow complex myofunctional exercises. Oral appliances designed for MFT may help children to perform orofacial exercises.
In this case report, 2 cases of malocclusion accompanying SDB, treated with prefabricated appliances for MFT have been reported; improvement in SDB and tooth alignment was noted in both cases.
A 7-year-old girl visited the pediatric dentistry department with the chief complaint of anterior teeth crowding. Body mass index (BMI) was in the 10th percentile, corresponding to normal obesity, with a calculated BMI of 14.0.
For diagnosis of SDB, Embletta MPR (ResMed Co., Australia), which measures AHI and average saturation of percutaneous oxygen (SpO2), was used for home respiratory polygraphy, and clinical symptoms of SDB were taken by interview with the patientās mother. In home respiratory polygraphy, AHI was 1.3 and average SpO2 was 96.6%. Based on an interview, the patientās oral habits included mouth breathing and nocturnal bruxism. According to the international classification of sleep disorders, the patient was diagnosed with pediatric obstructive sleep apnea as AHI was above 1.0.
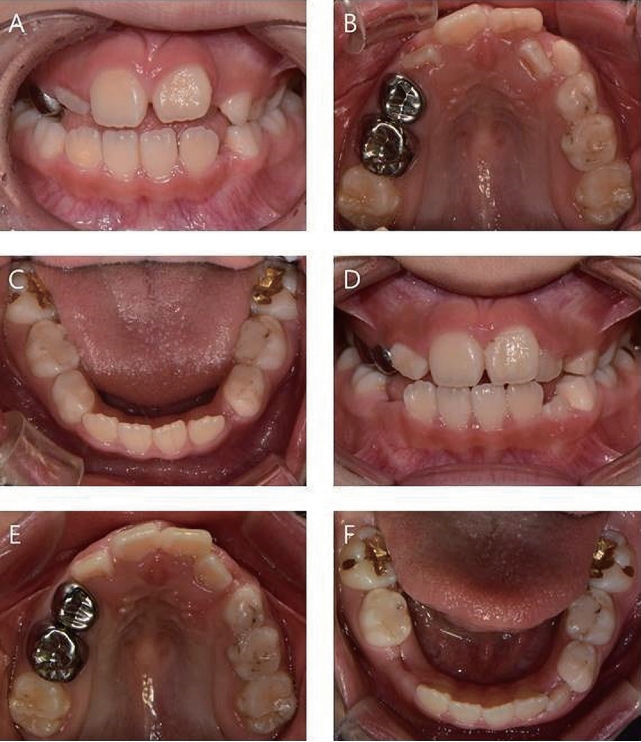
On extraoral examination, lateral profile was convex and lip incompetence was observed. Proclined upper incisors (U1 to SN of 110.2Ā°), substantial overjet (7.2 mm) and normal overbite (3.4 mm) were noted on cephalometric analysis. A large ANB (6.0Ā°) and reduced APDI (74.7Ā°) were also noted. FMA was 25.5Ā°, which meant a normal vertical growth. Further, a class II skeletal tendency with a mandible retruded in relation to the maxilla, were observed. As for soft tissue analysis, the upper lip was protruded (Nasolabial angle of 80.9Ā°) and lower lip was retruded (L-nasolabial angle of 68.8Ā°). In cast model analysis, the molar relationship was flush terminal plane and canine relationship was class I. Upper and lower arch forms were both narrow.
The patient was diagnosed with class II division 1 consequent to SDB. The patientās mother was informed that the main purpose of MFT was orthodontic improvement with concomitant resolution of SDB. Also comprehensive orthodontic treatment could be followed depending on the patientās needs and dental status. After consultation, treatment was initiated with a myofunctional appliance, EF line (OrthoPlus Co. Ltd., France) (Fig. 1). The patient was instructed to wear the appliance daily for at least 2 hours during the day and overnight while sleeping.
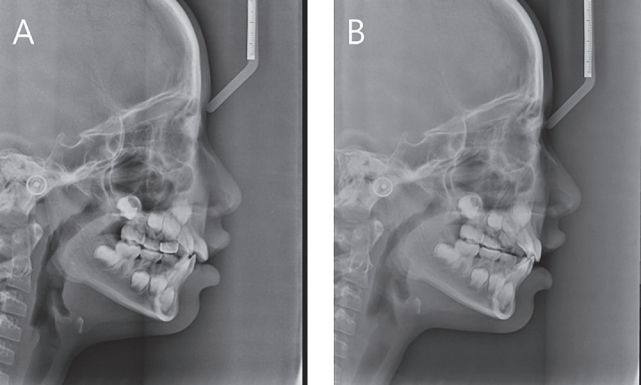
After 6 months of treatment, U1 to SN reduced from 110.2Ā° to 101.1Ā° and an IMPA increased from 94.4Ā° to 96.8Ā° (Fig. 2, Table 1). Overjet reduced from 7.2 mm to 3.7 mm, and overbite from 3.4 mm to 2.3 mm. Nasolabial angle and L-nasolabial angle increased form 80.9Ā° to 91.1Ā° and 68.8Ā° to 71.3Ā°, respectively. AHI had decreased from 1.3 to 0.6, and average SpO2 had increased from 96.6% to 97.2%. Oral breathing reverted to nasal breathing, and moderate lip competence with a decrease in bruxism were noted (Fig. 3). Intercuspid width between the centers of the dento-gingival junctions of deciduous canines had increased from 23.5 mm to 24.5 mm in the maxilla and from 19.7 mm to 20.8 mm in the mandible. There were no significant changes in bimolar width between the centers of dento-gingival junctions of the first permanent molars. Both upper and lower anterior crowding showed improved alignment (Fig. 4).
A 7-year-old girl presented at the pediatric dentistry department for the treatment of upper incisor crowding, bruxism, and chewing problem. BMI was in the 50th percentile, corresponding to normal obesity, with a calculated BMI of 15.9.
In home respiratory polygraphy, AHI was 1.8 and average SpO2 was 96.2%. According to an interview with the patientā s mother, oral habits included mouth breathing and nocturnal bruxism. Considering AHI and SDB symptoms, the patient was diagnosed with pediatric obstructive sleep apnea.
On extraoral examination, a convex lateral profile and poor lip competence were observed. On intraoral examination, tongue thrusting with an anterior openbite was found. Cephalometric analysis revealed retroclined upper incisors (U1 to SN of 99.4Ā°) and lower incisors (IMPA of 85.1Ā°). A reduced ANB (1.4Ā°) and APDI (73.3Ā°) were also noted. FMA was 39.3Ā°, which meant a vertical growth pattern. The skeletal pattern of malocclusion was ambiguous as ANB and APDI were contrary to each other. The nasolabial angle and U-nasolabial angle were both reduced. In cast model analysis, the molar relationship was flush terminal plane and 3 deciduous canines (#53, 73, 83) were prematurely lost. The mandibular midline was shifted about 2.6 mm to the right. The overbite was -1.4 mm and overjet was 3.8 mm. The upper and lower arch forms were tapered and ovoid, respectively.
The patient was diagnosed with Angleās class II division 2 malocclusion and had symptoms of SDB[13]. The patientā s mother was informed that MFT could be performed for the correction of tongue thrust and reduction of SDB in phase I treatment. Additionally, MFT should be followed by orthodontic re-evaluation because of insufficient space available for the unerupted permanent teeth. The use of a myofunctional appliance for treatment was also suggested and planned, with the consent of patientās mother. The patient was instructed to wear the appliance daily for at least 2 hours during the daytime, and overnight while sleeping.
After 6 months of treatment, there was an increase in the APDI from 73.3Ā° to 77.5Ā°, which is within the normal range (Fig. 5, Table 2). Clinically, convexity of the lateral facial profile was also found to decrease (Fig. 6). Bimolar width between the centers of the dento-gingival junctions of the first deciduous molars had increased from 21.4 mm to 22.9mm in the maxilla, and from 22.0 mm to 23.3 mm in the mandible. In contrast, bimolar width between the centers of the dento-gingival junctions of the first permanent molars had decreased from 29.5 mm to 28.3 mm in the maxilla, and from 31.3 mm to 31.1 mm in the mandible. AHI had decreased from 1.8 to 1.0 after 6 months of treatment, and average SpO2 had increased from 96.2% to 97.3%. Mouth breathing reverted to nasal breathing, and nocturnal bruxism had disappeared according to an interview with the patientās mother. SDB was improved by MFT, but upper anterior crowding remained (Fig. 7). In an effort to resolve the upper anterior crowding, fixed orthodontic treatment with first premolar extraction was planned.
The present case report describes improvement of SDB symptoms after orthodontic treatment with MFT in 2 patients with malocclusion and SDB.
For the treatment of SDB, custom-made mandibular advancement device is a representative appliance[14]. However, due to its rigidity, the transverse growth of jaws in the developing dentition may be impeded. In addition, consistent retention is hard to obtain when deciduous teeth exfoliate during the mixed dentition. In contrast, the prefabricated appliance used in the present report is made of elastic reinforced silicone, which can accommodate dentition regardless of the exfoliation of deciduous teeth. It also has specialized components for MFT such as tongue positioner and twin splint for the prevention of muscular interference
The gold standard method for diagnosing SDB is polysomnography, which is a particularly useful test for differentiating between the various different types of SDB[15]. However, polysomnography cannot be utilized to meet the high demand for diagnosis because it is comparatively costly and time-consuming. Portable sleep studies have been proposed as an alternative to polysomnography due to associated cost reduction and diagnostic convenience[16]. In the present cases, home respiratory polygraphy was used for measurement of AHI and average SpO2 instead of polysomnography.
AHI is a parameter based on the total number of apneas and hypopneas events divided by the total hours of sleep. Pediatric obstructive sleep apnea severity is classified as follows: mild (AHI = 1 - 5), moderate (AHI = 5 - 10), and severe (AHI > 10)[17]. In case 1, AHI indicating mild obstructive sleep apnea before treatment dropped below obstructive sleep apnea after treatment. In case 2, AHI was decreased to the borderline of mild obstructive sleep apnea after treatment. SpO2 is the other main parameter of ventilation disruptions associated with obstructive sleep apnea[18]. Average SpO2 increased in both of the present cases. These increases in SpO2 were considered to be caused by improvements in AHI, associated with changes in the occurrences of apneas and hypopnea, that influenced oxygen desaturation in arterial blood during sleep. The observed improvements in both major objective parameters during sleep suggest that myofunctional intervention for SDB with myofunctional disharmony has the potential to improve respiration quality during sleep.
Associations between SDB and dentofacial malocclusion have been reported in many studies. Kirsi et al .[19] suggested that children diagnosed with obstructive sleep apnea tended to have a significantly narrower maxillary arch, increased overjet, and shorter length of the mandibular arch compared with non-obstructed children. Carlos et al .[20] reported that children with obstructive sleep apnea grew more vertically, and had a tendency to exhibit class II skeletal malocclusion. Collectively, previous studies suggest that improvements in SDB need to be accompanied by orthodontic treatment.
MFT is one of the modalities for the treatment of SDB, and it has been shown to improve many problems of dentition including resolution of dental open bite and large overjet[21]. With regard to dental arches, prefabricated functional appliances stimulate transverse development in patients with crowding, and their effects appear to be greatest at the bimolar width of the first premolars rather than the first permanent molars[22]. Concordantly, the 2 patients in this case exhibited increased width between their deciduous canines or first deciduous molars, rather than their first permanent molars. These results suggest that prefabricated appliances made for MFT may be helpful for the treatment of crowding of the anterior teeth. However, reduced bimolar width was observed in case 2. It seemed likely that premature loss of the primary canines led to mesial drift of the first permanent molars. In a study reported by Kau et al .[23], extraction of the primary canine in the developing dentition reduced the perimeter of the arch due to forward movement of the molars. To maximize the transverse widening effect of prefabricated MFT appliances, the presence of the relevant primary canine is crucial.
The skeletal effects of MFT are still controversial. Ramirez et al .[24] reported that prefabricated functional appliances induced skeletal changes that were mainly associated with mandibular growth. Conversely, Katri et al .[25] reported that no significant differences were detected after treatment with such appliances. In the current 2 cases, effects of prefabricated myofunctional appliances were mainly confined to the dentoalveolar region. In case 1, proclined upper incisors were retruded and deep overbite decrease to normal range but no significant skeletal effects were found. In case 2, angulations of incisors were changed but no significant skeletal effects were found. However, the treatment period was relatively short in both cases. Further research is required to determine the longterm cephalometric results of such treatment.
In the cases described herein, the primary aims were to improve myofunctional disharmony, SDB, and malocclusion. In such cases, continuous motivation is required during the treatment process because a high level of compliance is key to the success of MFT. In both cases, AHI showed a decreasing tendency and symptoms of SDB disappeared. However, in some cases where myofunctional disharmony and SDB are improved, dental malalignment may remain after the treatment and orthodontic changes occurred mainly to dentoalveolar region rather than basal bone. Therefore, appropriate subsequent treatment options based on the patientās needs and dental status should be discussed with the patient in such cases and dentists should be aware of limitations of MFT.
SDB in early childhood can have adverse effects on myofunctional balance, and is associated with malocclusion. Orthodontic treatment, alone does not guarantee that these issues will be resolved. MFT may facilitate successful orthodontic treatment and maintenance.
In the present cases, prefabricated appliances for MFT were used and achieved favorable improvements in SDB. However, the orthodontic effect of MFT was mainly confined to the dentoalveolar region, and crowding was not resolved in the case of premature loss of primary canine. Prefabricated myofunctional appliances may constitute a viable alternative modality for the treatment of malocclusion complicated by SDB in carefully selected cases considering these limitations.
TableĀ 1.
Cephalometric mesurements before and after treatment in case 1
TableĀ 2.
Cephalometric mesurements before and after treatment in case 2
References
1. Simmons MS, Clark GT : The potentially harmful medical consequences of untreated sleep-disordered breathing: the evidence supporting brain damage. J Am Dent Assoc, 140:536-542, 2009.


2. Castronovo V, Zucconi M, Ferini-Strambi L, et al . : Prevalence of habitual snoring and sleep-disordered breathing in preschool-aged children in an Italian community. J Pediatr, 142:377-382, 2003.


3. Gislason T, BenediktsdĆ³ttir B : Snoring, apneic episodes, and nocturnal hypoxemia among children 6 months to 6 years old. Chest, 107:963-966, 1995.


4. Marcus CL, Brooks LJ, Spruyt K, et al . : Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatr, 130:714-755, 2012.

5. Amin R, Somers VK, Daniels S, et al . : Activity-adjusted 24-hour ambulatory blood pressure and cardiac remodeling in children with sleep disordered breathing. Hypertension, 51:84-91, 2008.


6. Sans Capdevila O, Crabtree VM, Kheirandish-Gozal L, Gozal D : Increased morning brain natriuretic peptide levels in children with nocturnal enuresis and sleep-disordered breathing: a community-based study. Pediatr, 121:1208-1214, 2008.

7. Gozal D : Sleep-disordered breathing and school performance in children. Pediatr, 102:616-620, 1998.

8. Gozal D, Kheirandish-Gozal L, Dayyat E, et al . : Obstructive sleep apnea and endothelial function in school-aged nonobese children: effect of adenotonsillectomy. Circulation, 116:2307-2314, 2007.


9. Sateia MJ : International classification of sleep disordersthird edition (ICSD-3). Chest, 146:1387-1394, 2014. 146:1387-1394, 2014.

10. Guilleminault C, Huang YS, Lin CH, et al . : Critical role of myofascial reeducation in pediatric sleep-disordered breathing. Sleep Med, 14:518-525, 2013.


11. Guilleminault C, Li KK, Martinez S, et al . : Sleep disordered breathing: surgical outcomes in prepubertal children. Laryngoscope, 114:132-137, 2004.


12. Huang YS, Guilleminault C : Pediatric obstructive sleep apnea and the critical role of oral-facial growth: evidences. Front Neurol, 3:184, 2013.



13. Katz MI : Angle classification revisited 2: a modified Angle classification. Am J Orthod Dentofacial Orthop, 102:277-284, 1992.


14. Villa MP, Bernkopf E, Ronchetti R, et al . : Randomized controlled study of an oral jaw-positioning appliance for the treatment of obstructive sleep apnea in children with malocclusion. Am J Respir Crit Care Med, 165:123-127, 2002.


15. Wise MS, Nichols CD, Hoban TF, et al . : Executive summary of respiratory indications for polysomnography in children: an evidence-based review. Sleep, 34:389-398, 2011.




16. Flemons WW, Littner MR, Loube DI, et al . : Home diagnosis of sleep apnea: a systematic review of the literature. Chest, 124:1543-1579, 2003.


17. Chuang LC, Lian YC, Huang YS, et al . : Passive myofunctional therapy applied on children with obstructive sleep apnea: a 6-month follow-up. J Formos Med Assoc, 116:536-541, 2017.


18. Caples SM, Garcia-Touchard A, Somers VK : Sleep-disordered breathing and cardiovascular risk. Sleep, 30:291-303, 2007.



19. PirilƤ-Parkkinen K, Pirttiniemi P, Lƶppƶnen H, et al . : Dental arch morphology in children with sleep-disordered breathing. Eur J Orthod, 31:160-167, 2009.



20. Flores-Mir C, Korayem M, Major PW, et al . : Craniofacial morphological characteristics in children with obstructive sleep apnea syndrome: a systematic review and metaanalysis. J Am Dent Assoc, 144:269-277, 2013.


21. Benkert KK : The effectiveness of orofacial myofunctional therapy in improving dental occlusion. Int J Orofacial Myology, 23:35-46, 1997.


22. Ramirez-YaƱez G, Sidlauskas A, Junior E, Fluter J : Dimensional changes in dental arches after treatment with a prefabricated functional appliance. J Clin Pediatr Dent, 31:279-283, 2007.


23. Kau CH, Durning P, Harzer W, et al . : Extractions as a form of interception in the developing dentition: a randomized controlled trial. J Orthod, 31:107-114, 2004.


- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 5,980 View
- 360 Download
- Related articles
-
Self-inflicted Tongue Ulceration in a Patient with Tourette Syndrome: A Case Report2016 August;43(3)







 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



