1.Saenger P., Wikland KA., Silberbach M,
et al. : Recommen-dations for the diagnosis and management of Turner syndrome.
J Clin Endocrinol Metab, 86:3061-3069, 2001.


2.Batch J : Turner syndrome in childhood and adolescence.
Best Pract Res Clin Endocrinol Metab, 16:465-482, 2002.


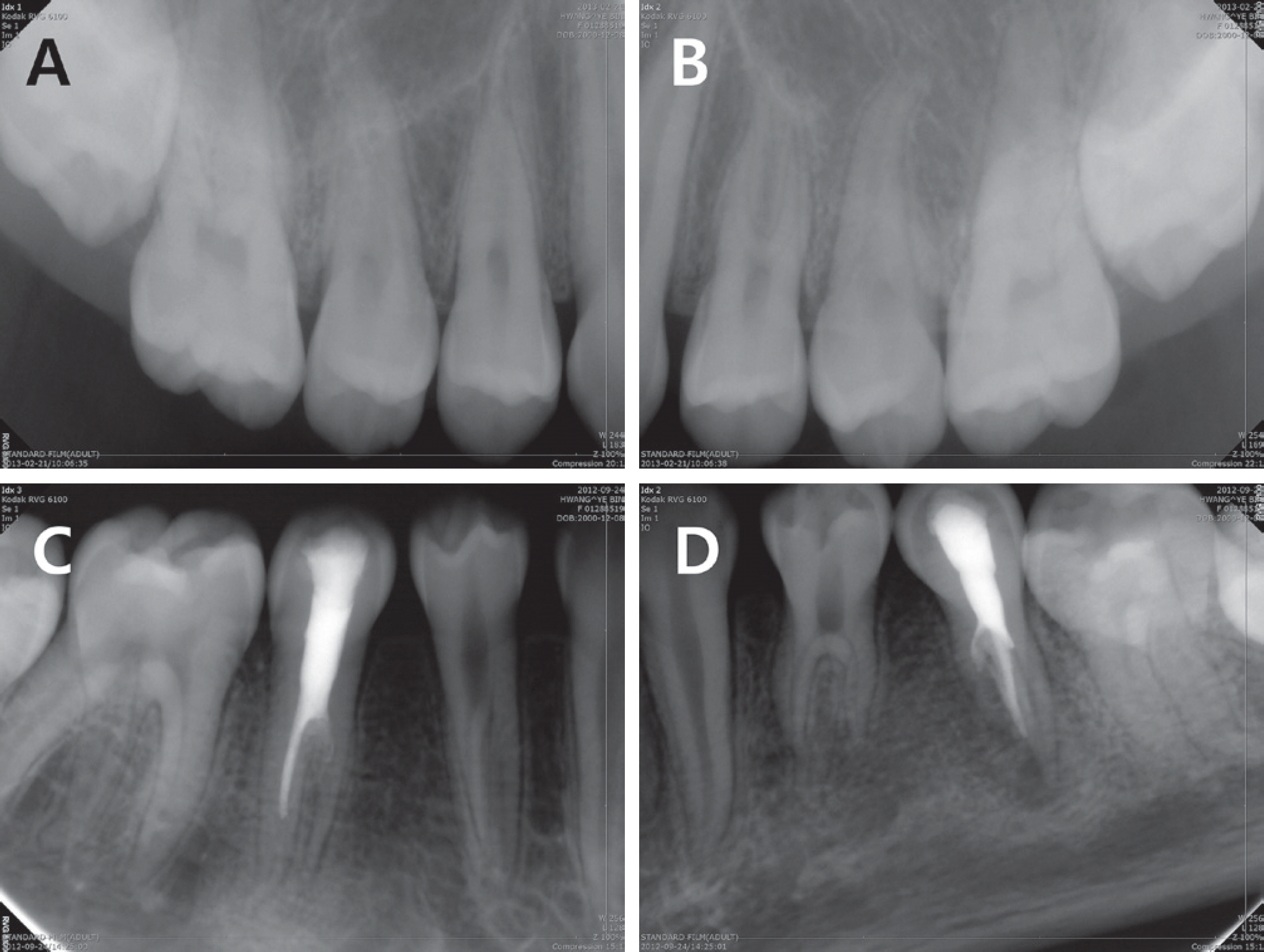
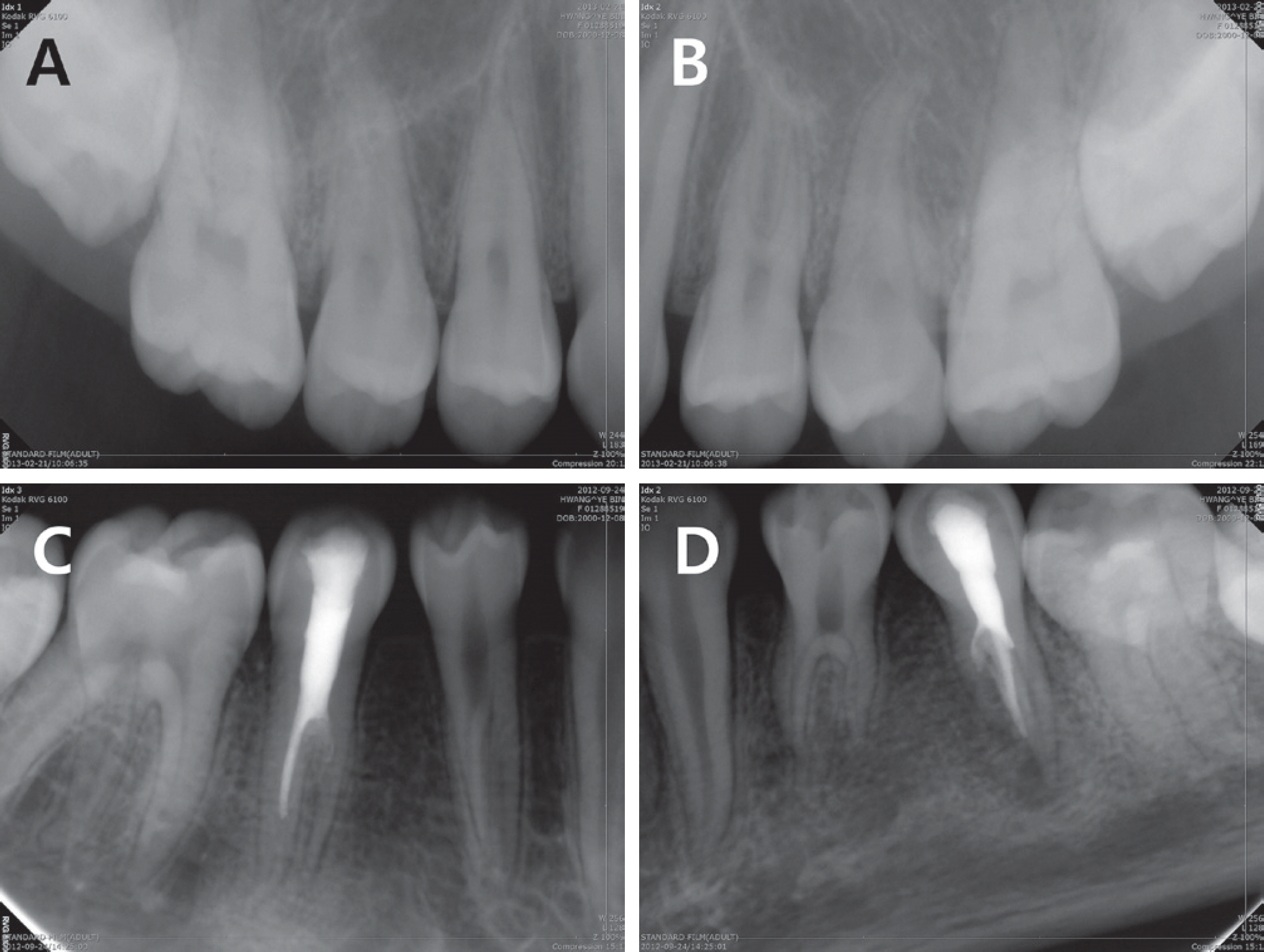
3.Faggella A., Guadagni MG., Piana G,
et al. : Dental features in patients with Turner syndrome.
Eur J Paediatr Dent, 7:165-168, 2006.

4.Ho VB., Bakalov VK., Bondy CA,
et al. : Major vascular anomalies in Turner syndrome: prevalence and magnetic resonance angiographic features.
Circulation, 110:1694-1700, 2004.


5.Szilágyi A., Keszthelyi G., Nagy G., Madléna M : Oral mani-festations of patients with Turner syndrome.
Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 89:577-584, 2000.


6.Varrela J : Root morphology of mandibular premolars in human 45,X females.
Arch Oral Biol, 35:109-112, 1990.


7.Midtbø M., Halse A : Tooth crown size and morphology in Turner syndrome.
Acta Odontol Scand, 52:7-19, 1994.


8.Varrela J., Alvesalo L., Mayhall J : Taurodontism in 45,X females.
J Dent Res, 69:494-495, 1990.


9.Gonzalez L., Witchel SF : The patient with Turner syndrome: puberty and medical management concerns.
Fertil Steril, 98:780-786, 2012.



10.López ME., Bazán C., Lorca IA., Chervonagura A : Oral and clinical characteristics of a group of patients with Turner syndrome.
Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 94:196-204, 2002.


11.Saenger P : Turner's Syndrome.
N Engl J Med, 335:1749-1754, 1996.


12.Gøtzsche CO., Krag-Olsen B., Kristensen BO,
et al. : Prevalence of cardiovascular malformations and association with karyotypes in Turner's syndrome.
Arch Dis Child, 71:433-436, 1994.



13.Sybert VP : Cardiovascular malformations and complications in Turner syndrome.
Pediatrics, 101:E11, 1998.

14.Lin AE., Lippe B., Rosenfeld RG : Further delineation of aortic dilation, dissection, and rupture in patients with Turner syndrome.
Pediatrics, 102:e12, 1998.


15.Mazzanti L., Cacciari E : Congenital heart disease in patients with Turner's syndrome. Italian Study Group for Turner Syndrome (ISGTS). J.
Pediatr, 133:688-692, 1998.

16.Knickmeyer RC : Turner syndrome: advances in understanding altered cognition, brain structure and function.
Curr Opin Neurol, 25:144-149, 2012.


17.Turner EK : A case of probable ovarian agenesis with Turner syndrome in a female child aged seven months.
Med J Aust, 41:39-42, 1954.


18.Horowitz SL., Morishima A : Palatal abnormalities in the syndrome of gonadal dysgenesis and its variants and in Noonan's syndrome.
Oral Surg Oral Med Oral Pathol, 38:839-844, 1974.


19.Townsend G., Jensen BL., Alvesalo L : Reduced tooth size in 45,X (Turner syndrome) females.
Am J Phys Anthropol, 65:367-371, 1984.


20.Varrela J., Townsend G., Alvesalo L : Tooth crown size in human females with 45,X/46,XX chromosomes.
Arch Oral Biol, 33:291-294, 1988.


21.Mayhall JT., Alvesalo L., Townsend GC : Tooth crown size in 46,X,i(Xq) human females.
Arch Oral Biol, 36:411-414, 1991.


22.Midtbø M., Halse A : Tooth crown size and morphology in Turner syndrome.
Acta Odontol Scand, 52:7-19, 1994.


23.Garn SM., Lewis AB., Kerewsky RS : X-linked inheritance of tooth size.
J Dent Res, 44:439-441, 1965.


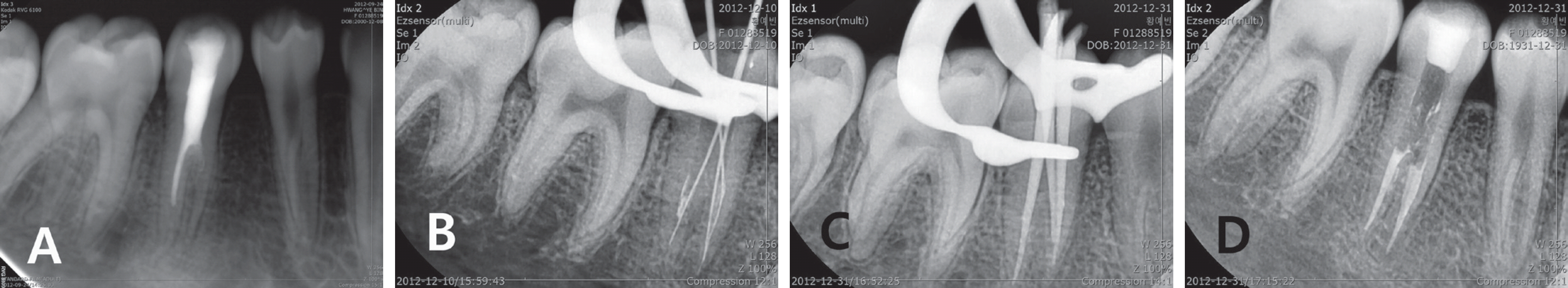
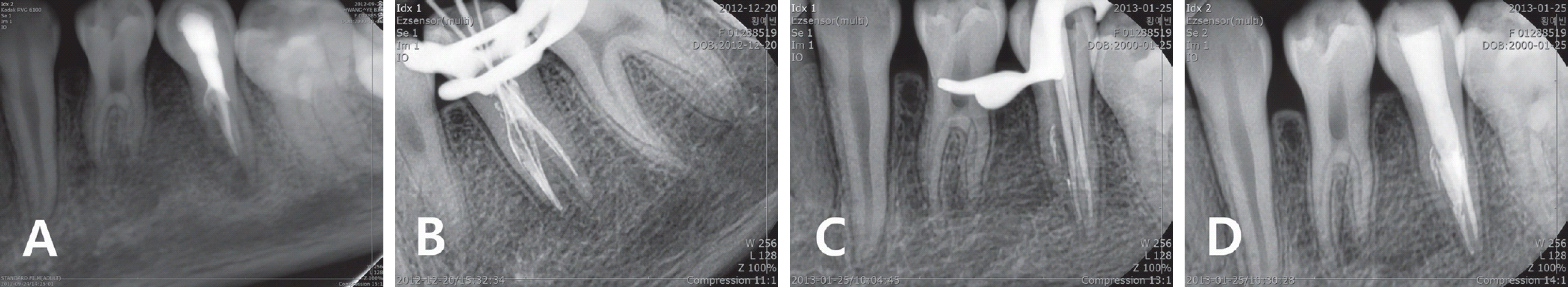
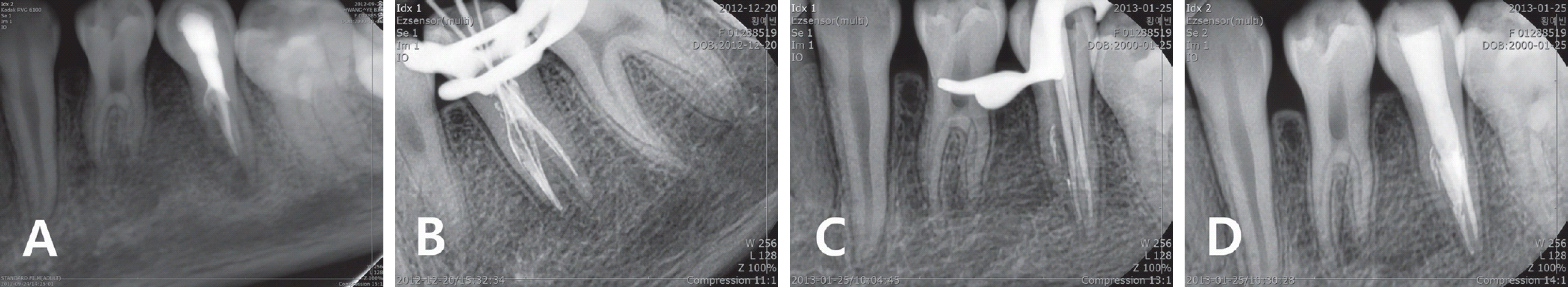
24.Kusiak A., Sadlak-Nowicka J., Limon J., Kochań ska B : Root morphology of mandibular premolars in 40 patients with Turner syndrome.
Int Endod J, 38:822-826, 2005.


25.MidtbMidtbø M., Halse A : Skeletal maturity, dental matu-rity, and eruption in young patients with Turner syndrome.
Acta Odontol Scand, 50:303-312, 1992.


26.Varrela J : Root morphology of mandibular premolars in human 45,X females.
Arch Oral Biol, 35:109-112, 1990.


27.Varrela J : Effect of 45,X/46,XX mosaics on root morphology of mandibular premolars.
J Dent Res, 71:1604-1606, 1992.


28.Cleghorn BM., Christie WH., Dong CC : The root and root canal morphology of the human mandibular first premolar: a literature review.
J Endod, 33:509-516, 2007.


29.Cleghorn BM., Christie WH., Dong CC : The root and root canal morphology of the human mandibular second premolar: a literature review.
J Endod, 33:1031-1037, 2007.


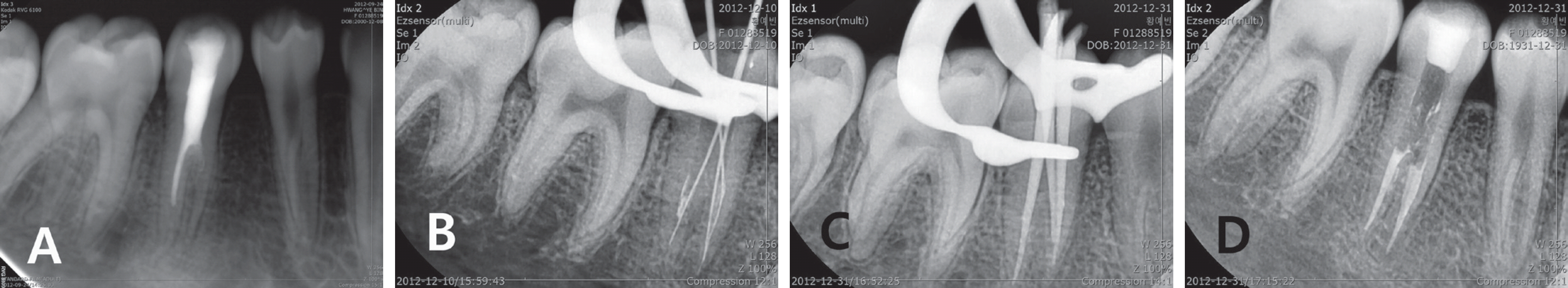
30.Bharti R., Chandra A., Tikku AP., Wadhwani KK : “Taurodontism” an endodontic challenge: a case report.
J Oral Sci, 51:471-474, 2009.


31.Varrela J., Alvesalo L : Taurodontism in females with extra X chromosomes.
J Craniofac Genet Dev Biol, 9:129-133, 1989.

32.Joseph M : Endodontic treatment in three taurodontic teeth associated with 48,XXXY Klinefelter syndrome: a review and case report.
Oral Surg Oral Med Pathol Oral Radiol Endod, 105:670-677, 2008.

33.Tsesis I., Shifman A., Kaufman AY : Taurodontism: an endodontic challenge. Report of a case.
J Endod, 29:353-355, 2003.