 |
 |
| J Korean Acad Pediatr Dent > Volume 46(1); 2019 > Article |
|
ņ┤łļĪØ
ļ│Ė ņŚ░ĻĄ¼ļŖö ņ£Āņ╣śņŚ┤ņŚÉņä£ ļ░£ņāØĒĢśļŖö ĒĢ©ņ×ģņä▒ ņåÉņāüņØś ĒŖ╣ņ¦ĢņØä ņĪ░ņé¼ĒĢśĻ│Ā ņןĻĖ░Ļ░äņØś ņČöņĀü ņĪ░ņé¼ ĻĖ░Ļ░ä ļÅÖņĢłņØś ņ£Āņ╣śņŚ┤ ļ░Å ņśüĻĄ¼ņ╣śņŚ┤ņŚÉ ļ░£ņāØĒĢśļŖö ĒĢ®ļ│æņ”ØņŚÉ ņśüĒ¢źņØä ļ»Ėņ╣Ā ņłś ņ׳ļŖö ņÜöņØĖņØä ĒÅēĻ░ĆĒĢśĻ│Āņ×É ĒĢśņśĆļŗż.
ņØ┤ļź╝ ņ£äĒĢ┤ ņ┤Ø 61ļ¬ģņØś 84Ļ░£ņØś ņ╣śņĢäĻ░Ć ņŚ░ĻĄ¼ļīĆņāüņ£╝ļĪ£ ņäĀņĀĢļÉśņ¢┤ ĒÖśņ×ÉņØś ņŚ░ļĀ╣, ņä▒ļ│ä, ņÖĖņāüņØś ņøÉņØĖĻ│╝ ļ░£ņāØņןņåī, ņÖĖņāü ņ╣śņĢäņØś ņåÉņāü ņĀĢļÅä, ņÖĖņāü ļ░£ņāØ ņŗ£ ļÅÖļ░śļÉ£ ļŗżļźĖ ņåÉņāü, ņ╣śļŻīļ░®ļ▓Ģ, ņČöņĀüņĪ░ņé¼ ĻĖ░Ļ░ä ņżæ ņ£Āņ╣śņŚ┤Ļ│╝ ņśüĻĄ¼ņ╣śņŚ┤ņŚÉ ļ░£ņāØĒĢ£ ĒĢ®ļ│æņ”ØņØ┤ ņĪ░ņé¼ļÉśņŚłļŗż. ņŚ░ļĀ╣, ņÖĖņāü ņ╣śņĢäņØś ņåÉņāü ņĀĢļÅä, ņÖĖņāü ļ░£ņāØ ņŗ£ ļÅÖļ░śļÉ£ ļŗżļźĖ ņåÉņāüņØś ņóģļźśĻ░Ć ņ£Āņ╣ś ļ░Å ņśüĻĄ¼ņ╣śņØś ņśłĒøäņŚÉ ļ»Ėņ╣śļŖö ņśüĒ¢źņØä ĒÖĢņØĖĒĢśĻĖ░ ņ£äĒĢ┤ ņĪ░ņé¼ļÉ£ ņ×ÉļŻīļŖö ņ╣┤ņØ┤ņĀ£Ļ│▒ Ļ▓ĆņĀĢĻ│╝ FisherņØś ņĀĢĒÖĢĻ▓ĆņĀĢņ£╝ļĪ£ ĒÅēĻ░ĆĒĢśņśĆļŗż.
ņ£ĀņĀäņ╣śņØś ĒĢ©ņ×ģņØĆ ļé©ņĢäņŚÉĻ▓ī ņŚ¼ņĢäļ│┤ļŗż ņÜ░ņäĖĒĢśĻ▓ī ļéśĒāĆļé¼ņ£╝ļ®░, ĒĢ©ņ×ģņØś ņøÉņØĖņ£╝ļĪ£ļŖö ļéÖņāüņØś ļ╣łļÅäĻ░Ć Ļ░Ćņן ļåÆņĢśļŗż. ņ£ĀņĀäņ╣śņØś ĒĢ©ņ×ģņØĆ ņ¦æņŚÉņä£ Ļ░Ćņן ļ¦ÄņØ┤ ļ░£ņāØĒ¢łņ£╝ļ®░, ņāüņĢģ ņ£ĀņżæņĀłņ╣śņŚÉņä£ Ļ░Ćņן ļ¦ÄņØ┤ ļ░£ņāØĒ¢łļŗż. ņ£Āņ╣śņŚ┤ņŚÉ ļ░£ņāØĒĢ£ ĒĢ©ņ×ģņØś ņżæņ”ØļÅäļŖö ņśüĻĄ¼ņ╣śņŚ┤ņŚÉ ļ░£ņāØĒĢśļŖö Ēøäņ£Āņ”ØņØś ļ░£ņāØņŚÉ ņ£ĀņØśĒĢśĻ▓ī ņśüĒ¢źņØä ļ»Ėņ│żļŗż(p= 0.014). ņ£Āņ╣śņØś ĒĢ©ņ×ģņä▒ ņåÉņāüņŚÉ ņŚ░ņĪ░ņ¦ü ņåÉņāüņØ┤ ļÅÖļ░śļÉ£ Ļ▓ĮņÜ░, ļŗżļźĖ ņ╣śņŻ╝ņĪ░ņ¦ü ņåÉņāüņØ┤ ļÅÖļ░śļÉ£ Ļ▓ĮņÜ░ ļ│┤ļŗż ĒĢ®ļ│æņ”ØņØś ļ░£ņāØņØ┤ ņ£ĀņØśĒĢśĻ▓ī ņĀüņŚłļŗż(p= 0.000).
Abstract
The purpose of this study was to investigate the characteristics of intrusion in primary dentition and to evaluate factors influencing complications of primary and permanent dentition during long-term follow-up period.
61 patients (84 teeth) were selected in this study. Medical records of 61 patients were reviewed and age, gender, cause of injury, site of injury, severity of traumatic injury, other injuries associated with trauma, treatment method, and complications of primary and permanent dentition were examined. Collected data were statistically evaluated using Chisquare test and FisherŌĆÖs exact test.
Intrusion in primary anterior teeth was predominant in boys over girls and fall was the most common cause of trauma. It was most common at home and occurred most in the primary maxillary central incisors. Severity had an effect on the incidence of sequelae in permanent successors (p= 0.014). The incidence of complications was significantly lower in patients with soft tissue injuries than in patients with other periodontal injuries (p= 0.000).
Intrusion refers the condition that the traumatized tooth is driven into its socket and this can lead pulp and/or periodontal tissue damage and alveolar bone fracture, resulting in pulp necrosis, crown discoloration, pathologic root resorption, or ankylosis[1-3]. Primary tooth intrusion commonly occurs between the ages of 1 and 3 years which corresponds to the time of calcification of the tooth germ of permanent successor[4-6]. Therefore, primary tooth intrusion can affect a wide range of pathologic changes to permanent successors, including hypoplasia, crown/root dilacerations, cessation of root development, and eruption disturbance[1,2,7,8].
In primary dentition, intrusion usually does not occur solely but in the complicated form. Thus when anticipating the prognosis of intruded primary teeth, it is reasonable to examine whether the other adjacent tissue such as soft tissue is involved together.
Due to spatially and anatomically close relationship between apex of the primary tooth and its permanent successor, intrusive injuries in primary dentition can lead to sequelae in permanent dentition. Therefore, the treatment of primary tooth intrusion should aim to prevent the possible damage to the tooth germ of permanent successors[9]. Therefore, it is necessary to identify complications in the intruded primary tooth as well as effect on permanent successors.
The International Association for Dental Traumatology (IADT) recommends different treatment strategies according to the root orientation of affected primary tooth. If apex is labially displaced, the tooth is left for anticipating spontaneous repositioning. Otherwise, the tooth needs removed when apex is displaced palatally[9].
The purpose of this study was to investigate characteristics of primary tooth intrusion and to evaluate factors influencing prognosis of primary and permanent dentition during the long-time follow-up period.
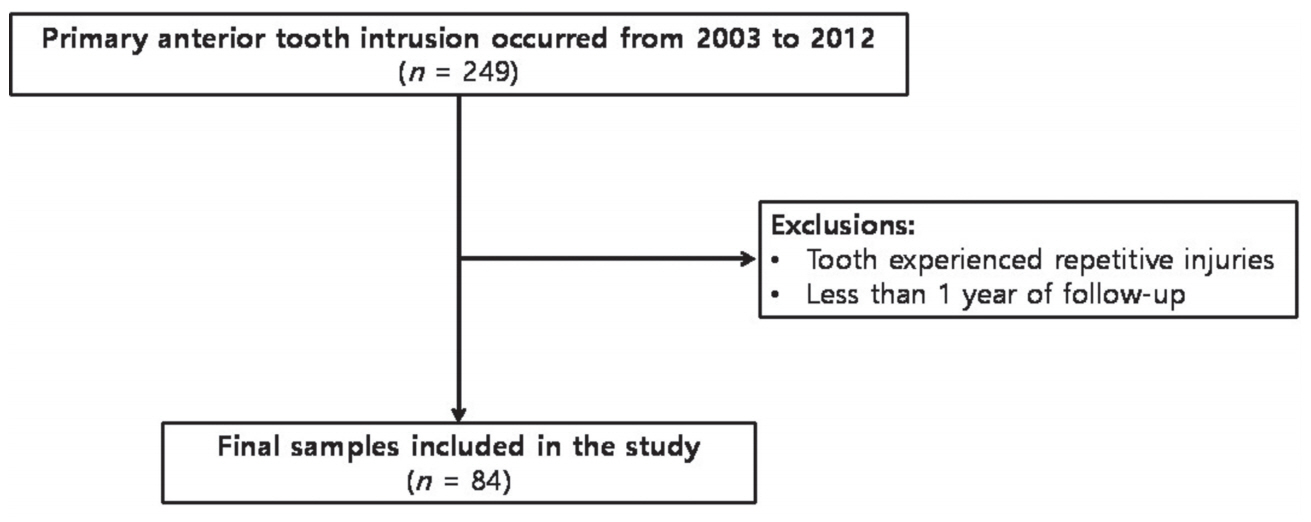
All patients who visited the Department of Pediatric Dentistry, School of Dentistry, Kyung Hee University, Seoul, Republic of Korea with chief complaints of traumatic dental injuries (TDIs) in the primary dentition between 2003 and 2012 were analyzed. Only patients who were diagnosed as primary anterior tooth intrusion were included. Patients with special medical history or repetitive TDIs during follow-up periods were excluded (Fig. 1). The study proposal was reviewed and approved by the ethics committee of Kyung Hee University Dental Hospital, Kyung Hee University, Seoul, Republic of Korea (KHDIRB-1408-1).
Based on trauma medical records, we collected data including clinical history, intraoral photographs and radiographic documentation of all patients. These data were organized according to age, gender, cause and site of trauma, severity of intrusion, other type of injuries accompanied at the time of injuries and complications during the follow-up periods in both primary and permanent dentition.
Severity of intrusion was classified into mild, moderate, or severe type by evaluation of clinical photographs and periapical radiographs at the time of injury. An adjacent primary incisor with no evidence of displacement was established as a baseline. Comparing with the baseline, it was defined as mild type when greater than half of clinical crown exposure was presented upon the gingival tissue, and moderate type as less than half of clinical crown exposure. Severe type was defined as a total of clinical crown was intruded.
Other types of injury accompanied at the time of TDI occurred were divided by classification of Andreasen et al .[2]; soft tissue injuries, hard dental tissue injuries, and periodontal tissue injuries.
1. Injuries to the soft tissue: abrasion, laceration and contusion;
2. Injuries to the hard tissue and the pulp: enamel crack, enamel fracture, enamel-dentin fracture without pulp exposure, enamel-dentin fracture with pulp exposure, enamel-dentin-cementum fracture without pulp exposure, enamel-dentin-cementum fracture with pulp exposure and root fracture;
3. Injuries to the periodontal tissue: concussion, subluxation, displacement, intrusion, extrusion and avulsion.
To evaluate clinical outcomes after primary tooth intrusion, only patients who were followed-up more than 1 year were included. Patients were scheduled for clinical and radiographic examination every 3 - 6 months until the physiologic exfoliation of intruded primary tooth and eruption of permanent successor. The follow-up period varied from 0.1 to 8.10 years (mean [SD], 1.8 [1.10] years).
Complication was grouped into 2 categories; (1) complication in primary tooth, and (2) complication in permanent successor. Crown discoloration, pulp canal obliteration, periapical abscess formation, inflammatory root resorption, and ankylosis were included as complication in primary tooth. To assess clinical outcome, clinical success was defined as discoloration only, pulp canal obliteration, and no complication and failure was defined when the traumatized tooth needed further treatment; periapical abscess formation, inflammatory root resorption, ankyloses. In permanent successor, enamel hypoplasia and crown shape malformation were recorded.
Data were analyzed using SPSS 22.0 software (SPSS Inc., Chicago, IL, USA). In order to determine the factors that affect prognosis, age, severity and type of accompanied injury were examined statistically. As the number of teeth which were followed-up until their successors erupt was small, influence of age and severity on prognosis of permanent tooth was statistically analyzed using FisherŌĆÖs exact test. For the same reason, difference in incidence of primary tooth complication according to a type of accompanied injury was analyzed using FisherŌĆÖ s exact test. On the other hand, effect of age and severity on primary tooth complication was statistically analyzed with Chisquare test.
Of 176 children (249 teeth) who were diagnosed as primary tooth intrusion, 61 children (84 teeth) who met the inclusion criteria were evaluated. The mean age of these samples was 3.1 ┬▒ 1.3 years old and most prevalent age was 2 - 3 years in both boy and girl group. The final samples consisted of 40 (65.6%) boys and 21 (34.4%) girls. Intrusion occurred predominantly in males than in females, with a ratio of 1.90:1 (Table 1). Complication in primary and permanent tooth according to age is presented in Table 2. However, there was no statistical difference in incidence of complication in primary (Table 3, p= 0.197) and permanent tooth (Table 4, p= 0.237) according to age.
Causes and sites of intrusion were as follows (Table 5): Falls (51.2%) were the major sources of intrusion and most of intrusion occurred at home (56%) and the area around the home (31%).
Intrusion was commonly observed in primary maxillary central incisors (81%) with no difference between right and left teeth followed by primary maxillary lateral incisors (19%). 40 patients (65.6%) presented with a single affected tooth; 19 patients (31.1%) with 2 affected teeth; 2 patients (3.3%) with multiple affected teeth.
According to severity of intrusion, approximately half of tooth intrusion was mild type, followed by moderate type (32.1%) and severe type (14.3%). The severity of intrusion did not affect significantly the incidence of complication (Table 6, p= 0.082). However, it had an effect on the incidence of sequelae in permanent successors (Table 7, p= 0.014).
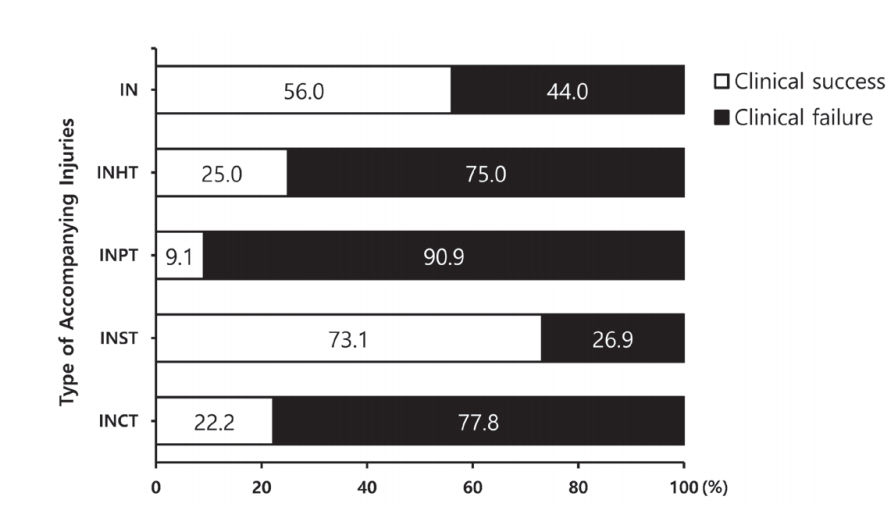
Of 84 teeth, 45 teeth (53.6%) exhibited clinical complications in affected primary teeth during the follow-up periods, and 39 teeth (46.4%) did not. Table 8 shows the clinical complications in primary tooth intrusion according to presence of other type of TDIs accompanied on the adjacent primary teeth. When primary tooth intrusion occurred with other periodontal tissue injuries simultaneously, the affected tooth was more likely to develop clinical complications. However, when intrusion was accompanied with soft tissue injuries, complications were significantly fewer (Fig. 2).
TDIs in the primary dentition can negatively affect the quality of life of children[10,11]. Especially in the children with developing permanent teeth, all kinds of TDIs can have a harmful effect on their quality of life for the whole their lives by causing developmental disorder on permanent teeth. Particularly the intrusive TDI to the primary teeth is likely to harm the successor of theirs due to spatial and anatomical position of primary and permanent teeth.
Most children suffer from primary tooth intrusion in the early stage of their lives. In the present study, higher incidence of intrusion was observed in 2 - 3 years. In this age group, children are likely to experience TDIs due to insufficient motor skills[4,12]. However, even in patients of the same age group, each patient may have all the different degrees of severity. And this can demonstrate why age was not a factor affecting the prognosis of primary and permanent tooth.
From this study, fall was predominant cause of intrusive dental injury accounting for 51.2% followed by collision and this result is in agreement with previous studies[13-15].
Moreover, approximately 84% of children in this age experienced intrusive luxation at home and around home in the present study. This is because children in this age spend most of their life time at home[16]. Based on these findings, educational program for caregivers regarding prevention and home care of TDIs can be beneficial.
Because of their anterior position in the dental arch, most intrusive luxation occurs in maxillary central incisors[5,7]. In this study, intrusive luxation usually involved a single primary tooth, which corresponded with previous studies[5,12].
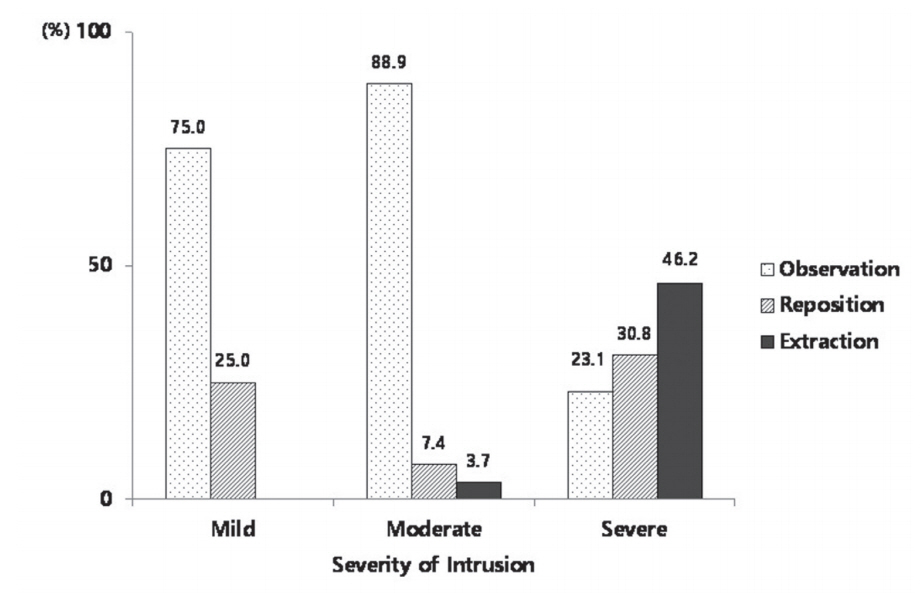
In terms of severity, mild type was most common followed by moderate type in this study. In severe intrusion cases, permanent successor presented unfavorable outcomes more frequently. Therefore, it is reasonable to rely not only on the path or direction of intrusion but also on the remaining portion of intruded tooth when selecting the treatment method and anticipating the prognosis of involved tooth. In the present study, 75% of mild type teeth, 88.9% of moderate type teeth and 23.1% of severe type teeth were observed without any intervention. And reposition was performed to 25% of mild type teeth, 7.4% of moderate type teeth and 30.8% of severe type tooth (Fig. 4).
In this study, 45 teeth (53.6%) of 84 teeth presented unfavorable outcomes in the primary teeth during the periodical check-up. Borum and Andreasen[17] reported inflammatory root resorption accounted for 14% of complications in the primary teeth following intrusion. Whereas in this study the inflammatory root resorption (71.1%) was the most common complication and followed by periapical abscess (35.6%). In the previous studies, the percentage of developmental disturbances of the permanent successors after intrusive dental injury ranges from 18% to 69%[6,18,19]. Likewise, 5 teeth (20.0%) of 25 successors presented complication in the permanent teeth in the study.
As most of intrusive dental injuries were consequences of fall accident, intrusive dental injuries usually occur in multiple teeth and are accompanied by multiple site injuries such as hard and soft tissues. In the present study, the intruded teeth accompanied with periodontal tissue injury showed unfavorable outcomes more frequently. While the intruded teeth accompanied with soft tissue injury were more likely to present favorable outcomes. This can be explained by the fact soft tissues like gingiva and buccal mucosa are softer than hard tissue and can absorb and favorably distribute impact from trauma[20-22].
However, there are several limitations in this study. First, since this study was performed retrospectively based on medical records, there was a possibility that majority of complicated type of injuries were included in ŌĆśintrusion onlyŌĆÖ group. For example concussion or subluxation of adjacent primary incisors could be ignored during the examination due to young patientŌĆÖs age. Second, as the number of intruded primary teeth which were followed-up until their permanent successors erupt was small, we could not statistically determine the effect of intrusive injuries on permanent successors development. Nonetheless, this study is significant in that a research on sequelae of permanent successors was carried out through long-term follow-up and in that this study determined factors influencing the outcome of intruded primary teeth and their successors. This retrospective study suggested that the severity of primary tooth intrusion can influence prognosis of permanent successor and when intrusion occurs with soft tissue injuries, traumatized primary tooth is likely to show favorable prognosis.
In this retrospective study, the intrusion occurred most frequently at home and fall accident was major cause of intrusion. Therefore caregivers such as parents should be trained about prevention of TDIs and should be encouraged to visit dental hospital in order to confirm whether the permanent successor is involved. Furthermore the clinician should provide periodic recall plan to the parents and exact periodic check with radiographs.
Within the limits of this study, age was not a factor which influence incidence of complication. However, severity of intrusion had an effect on incidence of sequelae in permanent successor and intrusion accompanied with soft tissue injury was likely to present better prognosis and show fewer complication.
On the basis of present study, when choosing a treatment method and predicting prognosis of intruded teeth, the clinician needs to depend not only on the intrusion path or direction, but also on the depth of intrusion or portion of crown above the gingiva and type of accompanied injuries.
Since the number of samples used in this study is limited, further studies with larger number of samples and longer follow-up period are needed.
Fig┬Ā2.
Clinical outcomes of primary tooth intrusion according to presence of accompanying other TDIs to the adjacent primary teeth.
IN = Intrusion only, INHT = Intrusion accompanied with hard tissue injuries, INPT = Intrusion accompanied with periodontal tissue injuries, INST = Intrusion accompanied with soft tissue injuries, INCT = Intrusion accompanied with complicated tissue injuries.
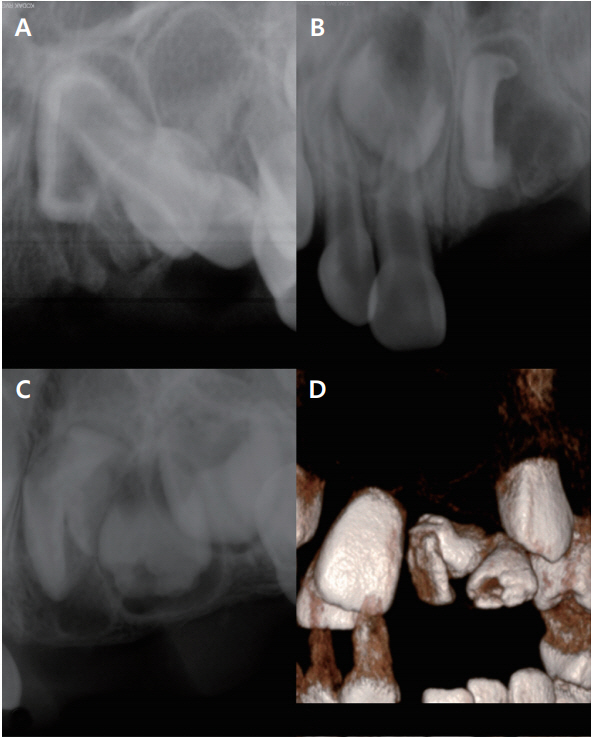
Fig┬Ā3.
Long-time follow up of patient 2. (A) Initial periapical radiograph showing intrusion of left maxillary primary incisors. Displacement of permanent tooth germ was revealed. (B) Progressing periapical radiograph at the 3 months follow-up. (C) Progressing periapical radiograph at the 3 years follow-up showing crown deformation in both permanent incisors. (D) Progressing periapical radiograph at the 6 years follow-up. Large extent of crown deformation was observed in both permanent incisors.
Table┬Ā1.
Age and gender distribution of patients
Table┬Ā2.
Age and complication in primary and permanent dentition
| Age (year) | Total | Complication in Primary Tooth | Followed-up Cases1 | Sequelae in Permanent Successor |
|---|---|---|---|---|
| n (%) | ||||
| 0-2 | 25 | 11 (44.0) | 11 | 4 (36.4) |
| 2-5 | 54 | 34 (63.0) | 12 | 1 (7.1) |
| 5- | 5 | 1 (20.0) | 2 | 0 (0.0) |
Table┬Ā3.
Age and complication in primary tooth
| Age (year) | No Complication | Complication | Total | p value |
|---|---|---|---|---|
| n | ||||
| 0-2 | 14 | 11 | 25 | 0.197 |
| 2- | 24 | 35 | 59 | |
| Total | 38 | 46 | 84 | |
Table┬Ā4.
Age and complication in permanent tooth
| Age (year) | No Complication | Complication | Total | p value |
|---|---|---|---|---|
| n | ||||
| 0-2 | 7 | 4 | 11 | 0.237 |
| 2-5 | 11 | 1 | 12 | |
| 5- | 2 | 0 | 2 | |
| Total | 20 | 5 | 25 | |
Table┬Ā5.
Cause and site of intrusion according to the age group
Table┬Ā6.
Severity of intrusion and complication in primary tooth
| Severity | No Complication | Complication | Total | p value |
|---|---|---|---|---|
| n (%) | ||||
| Mild1 | 18 (40.0) | 27 (60.0) | 45 | 0.082 |
| Moderate2 | 11 (40.7) | 16 (59.3) | 27 | |
| Severe3 | 9 (75.0) | 3 (25.0) | 12 | |
| Total | 38 (45.2) | 46 (54.8) | 84 | |
Table┬Ā7.
Severity of intrusion and sequelae in permanent successor
| Severity | No Sequelae | Sequelae | Total | p value |
|---|---|---|---|---|
| n (%) | ||||
| Mild1 | 11 (100.0) | 0 (0.0) | 11 | 0.014 |
| Moderate2 | 5 (83.3) | 1 (16.7) | 6 | |
| Severe3 | 4 (50.0) | 4 (50.0) | 8 | |
| Total | 20 (80.0) | 5 (20.0) | 25 | |
Table┬Ā8.
Clinical outcomes of primary teeth intrusions
| Favorable | Unfavorable | p value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| None | Crown Discoloration | Pulp Canal Obliteration | Total | Periapical Abscess | Inflammatory Root Resorption | Ankylosis | Total | ||
| IN1 | 11 | 3 | 2 | 14 | 2 | 9 | 3 | 11 | 0.000 |
| INHT2 | 0 | 1 | 0 | 1 | 3 | 2 | 0 | 3 | |
| INPT3 | 1 | 0 | 0 | 1 | 5 | 5 | 2 | 10 | |
| INST4 | 15 | 4 | 0 | 19 | 1 | 7 | 0 | 7 | |
| INCT5 | 4 | 0 | 0 | 4 | 5 | 9 | 2 | 14 | |
Table┬Ā9.
Sequelae of permanent successors after primary tooth intrusion
References
1. Diab M, elBadrawy HE : Intrusion injuries of primary incisors. Part II: Sequelae affecting the intruded primary incisors. Quintessence Int, 31:335-341, 2000.

2. Andreasen JO, Andreasen FM, Andersson L : Textbook and color atlas of traumatic injuries to the teeth. 4th ed. Blackwell Munksgaard, Cophenhagen, 542-576, 2007.
3. Tarj├Īn J, Balaton P, K├®ri I : Consequence and therapy of primary tooth intrusion. J Int Assoc Dent Child, 19:25-28, 1988.

4. Altun C, Cehreli ZC, G├╝ven G, Acikel C : Traumatic intrusion of primary teeth and its effects on the permanent successors: a clinical follow-up study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 107:493-498, 2009.


5. Colak I, Markovic D, Milenkovic A, et al. : A retrospective study of intrusive injuries in primary dentition. Dent Traumatol, 25:605-610, 2009.


6. Zilberman Y, Fuks A, Lustmann J, et al. : Effect of trauma to primary incisors on root development of their permanent successors. Pediatr Dent. 8:289-293, 1986.

7. Gondim JO, Moreira Neto JJ : Evaluation of intruded primary incisors. Dent Traumatol, 21:131-133, 2005.


8. Onetto JE, Flores MT, Garbarino ML : Dental trauma in children and adolescents in Valparaiso, Chile. Endod Dent Traumatol, 10:223-227, 1994.


9. Malmgren B, Andreasen JO, Tsukiboshi M, et al. : International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 3. Injuries in the primary dentition. Dent Traumatol, 28:174-182, 2012.


10. Cortes MI, Marcenes W, Sheiham A : Impact of traumatic injuries to the permanent teeth on the oral health-related quality of life in 12-14-year-old children. Community Dent Oral Epidemiol, 30:193-198, 2002.


11. Ramos-Jorge ML, Bosco VL, Peres MA, Nunes AC : The impact of treatment of dental trauma on the quality of life of adolescents - a case-control study in southern Brazil. Dent Traumatol, 23:114-119, 2007.


12. Kramer PF, Zembruski C, Ferreira SH, Feldens CA : Traumatic dental injuries in Brazilian preschool children. Dent Traumatol, 19:299-303, 2003.


13. Fleming P, Gregg TA, Saunders ID : Analysis of an emergency dental service provided at a childrenŌĆÖs hospital. Int J Paediatr Dent, 1:25-30, 1991.


14. Sandalli N, Cildir S, Guler N : Clinical investigation of traumatic injuries in Yeditepe University, Turkey during the last 3 years. Dent Traumatol, 21:188-194, 2005.


15. Skaare AB, Jacobsen I : Primary tooth injuries in Norwegian children (1-8 years). Dent Traumatol, 21:315-319, 2005. 21:315-319, 2005.
16. Carvalho V, Jacomo DR, Campos V : Frequency of intrusive luxation in deciduous teeth and its effects. Dent Traumatol, 26:304-307, 2010.


17. Borum MK, Andreasen JO : Therapeutic and economic implications of traumatic dental injuries in Denmark: an estimate based on 7549 patients treated at a major trauma centre. Int J Paediatr Dent, 11:249-258, 2001.


18. von Arx T : Developmental disturbances of permanent teeth following trauma to the primary dentition. 38:1-10, 1993.

19. Tewari N, Mathur VP, Pandey RK, et al . : Long-term effects of traumatic dental injuries of primary dentition on permanent successors: A retrospective study of 596 teeth. Dent Traumatol, 34:129-134, 2018.


20. Choi WJ, Russell CM, Robinovitch SN, et al . : Age-related changes in dynamic compressive properties of trochanteric soft tissues over the hip. J Biomech, 48:695-700, 2015.


- TOOLS
-
METRICS

-
- 3 Crossref
- 0 Scopus
- 4,113 View
- 216 Download
- Related articles
-
Factors Influencing the Duration of Forced Eruption in Impacted Maxillary Canines2022 November;49(4)



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



