대구치-절치 형태이상 환자의 임상적 치료 및 단기 예후: 증례 보고
Clinical Management and Short-term Prognosis of Molar-Incisor Malformation Affected Patients: Case Reports
Article information
Abstract
대구치-절치 형태이상(MIM)은 비교적 최근에 보고되고 있는 치아의 형태 이상으로, 주로 제1대구치의 치근, 제2유구치의 치근, 상악 중절치의 치관에 형태이상이 나타난다. MIM을 일으키는 원인에 대해서는 아직 정확하게 밝혀진 바가 없으나, 공통적으로, 조산을 포함한 생 후 1 - 2년 이내에 발생한 의학적 병력을 가진다. MIM에 영향을 받은 제1대구치는 임상적으로 정상적인 치관 형태를 가지므로, 정확한 진단을 위해서는 방사선학적 검사가 꼭 필요하다. 주로 대구치 부위의 극심한 통증과 붓기를 주소로 내원하여 발견되는 경우가 많으며, 염증이 심하지 않고, 치근의 형태 이상이 비교적 양호한 경우에는 근관치료를 시도해 볼 수 있다. 그러나 치근주위 염증이 상당히 진행되어 광범위한 치조골 소실이 관찰되는 경우 발치가 불가피하다. 발치를 해야 하는 경우에는 발치 시기와 제3대구치의 존재 여부를 고려해야 하며, 추후 안정적인 교합을 위해서 적절한 공간 관리와 장기적인 계획이 필요하다. MIM 환자들은 혼합치열기에 있으므로, 정확한 진단과 시기에 맞는 적절한 치료가 중요하다. 이번 증례에서는 두 명의 MIM 어린이의 치료과정과 치료 후 2년의 경과에 대하여 보고하는 바이다.
Trans Abstract
Molar-incisor malformation (MIM) is a newly reported dental anomaly with molar root deformity and incisor crown defects. MIM-affected teeth may cause severe pain with no apparent tooth caries. Since the affected molars clinically appear normal, radiographs are recommended for accurate diagnosis on the first visit. Since MIM-affected patients are in mixed dentition, timely and appropriate interventions are needed to avoid unnecessary pain and complicated clinical issues. This report was written to describe two patients who had MIM in early mixed dentition and report their 2-year follow-ups.
Ⅰ. Introduction
The term molar-incisor malformation (MIM) was first coined in Lee et al.[1] case reports in 2014. MIM is a relatively new type of dental anomaly that mainly appear on permanent first molars and permanent maxillary central incisors[1-3].
The first descriptions of this anomaly were malformed roots and a distinctly narrowed pulp chamber with a mineralized diaphragm reported by Witt at al. in 2014[2]. Features of MIM are deviated roots and a constricted pulp chamber on permanent first molars and sometimes on primary second molars, and cervical notches on clinical crowns of permanent maxillary central incisors[1,2,4,5]. Despite serious root anomaly of permanent first molars and primary second molars, their clinical crowns appear normal[1]. This makes clinicians difficult to diagnose and even miss the abnormality. Therefore, taking radiographs is recommended on examination. MIM patients would complain of severe pain and gingival swelling with periapical lesion accompanied by periodontal bone loss on the affected regions[4,5]. These patients in mixed dentition need timely and proper treatments to avoid unnecessary pain and complicated clinical issues.
In this paper, how MIM-affected children were clinically managed and their prognosis in 2 years were presented.
Ⅱ. Case Report
1. Case 1
A-9-year-old girl presented to the department of pediatric dentistry with chief complaints of severe pain and gingival swelling on the right mandibular first permanent molar. Periodontal pockets deep enough to reach the apical area were present on both mandibular first permanent molars. The patient had been taking antibiotics and painkillers prescribed at a local dental clinic. The pain had been occasional and endurable. Symptoms became worsen by the time of the visit, which lead the patient to awaken during the nighttime. On medical history scanning, the patient was born 15 days earlier than the expected date and diagnosed with neonatal jaundice 10 days after birth, which had the patient hospitalized and undergo blood transfusion.
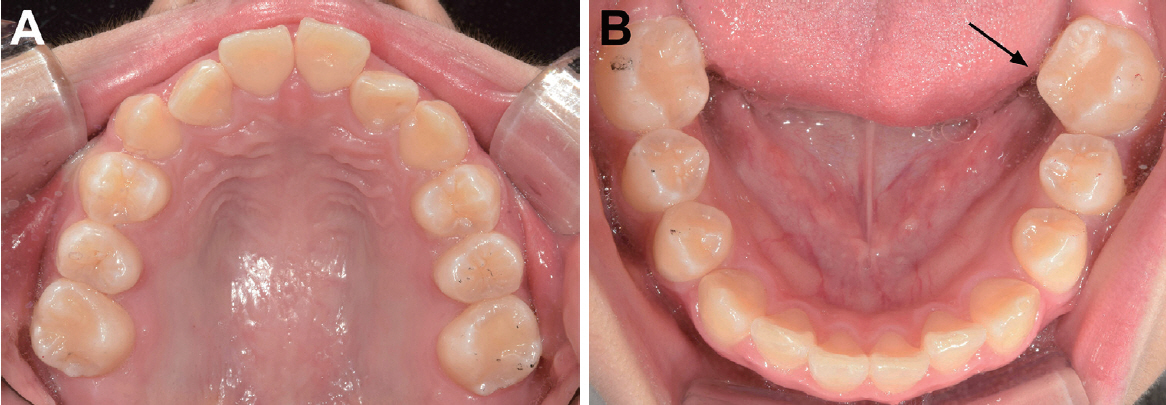
The patient had been misdiagnosed with dentin dysplasia type Ⅰ (DD type Ⅰ) a year ago. Sealant (3M ESPE, St. Paul, MN, USA), a prophylactic therapy, was applied on the 4 permanent first molars. On the re-visit 1 year after due to unbearable pain on the right molar region, both mandibular permanent first molars were percussion-sensitive with no obvious tooth mobility on intraoral examination. The clinical crowns of both mandibular permanent first molars appeared morphologically normal without dental caries. Three of primary second molars, except for the one in the upper left quadrant had been exfoliated before the primary first molars shed. Periapical radiographs revealed malformed and atypical root forms on both mandibular first permanent molars (Fig. 1A, 1B). A sinus tract was formed on the buccal side of the right mandibular permanent first molar. Root canal treatment was performed on the affected molar with notification of the possibility of extraction. There was difficulty in canal negotiation arising from deformity of the pulp cavity and orifices to radicular canals. To obtain specific images of the tooth, cone-beam computed tomography (CBCT) was taken. Unconventional root forms, slit-shaped pulp cavity and severe periodontal bone loss around bilateral mandibular first permanent molars were revealed on CBCT (Fig. 2). Bilateral mandibular first permanent molars were decided to be extracted based on considerable alveolar bone resorption due to periodontal inflammation and malformed tooth structure that was difficult to be endodontically treated.

Periapical views of the first patient showing atypical root shape and slit-like pulp chamber of the MIM-affected molars. (A) Right mandibular permanent first molar. (B) Left mandibular permanent first molar.
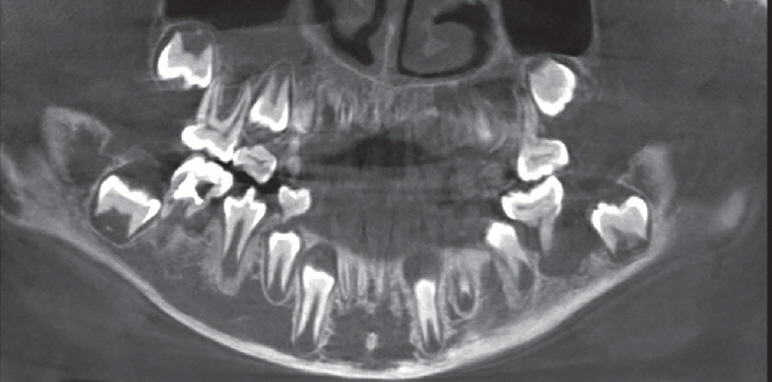
Cone-beam computed tomography image of the first patient showing severe bone resorption on both mandibular permanent first molars after endodontic access opening on the right first permanent molar that was temporarily filled.
Before removal of the first permanent molars, comprehensive orthodontic analysis was performed and the formation stage of the second permanent molars was stage E (Demerjian’s method)[6]. The affected molars were eventually removed. As there was the potential for problems such as supra-eruption of the opposing teeth after extraction, a maxillary removable appliance with Adams clasps on permanent first molars and primary first molars was placed (Fig. 3).
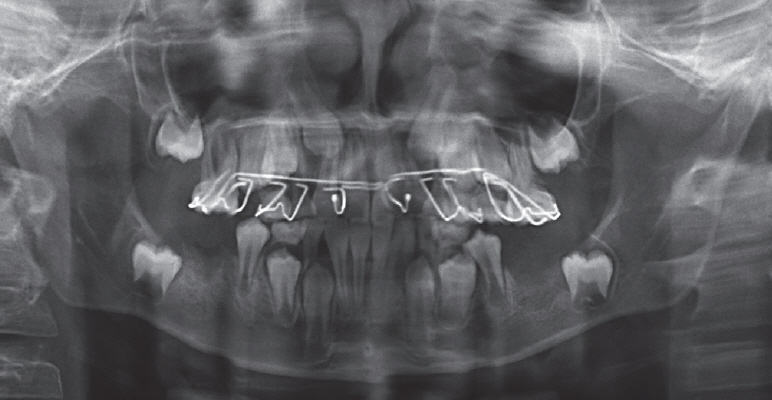
Panoramic radiograph of the first patient (at the age of 9 years and 11 months) showing after extraction of bilateral mandibular permanent first molars, a removable appliance placed on the maxilla, and permanent second molars being developed in the bone.
The patient complained of pain on the right maxillary first permanent molar with a sinus tract on the buccal side. Root canal treatment had been planned on the right maxillary first molar, however, a month later, the pain disappeared. After 6 months, the patient complained of recurred pain on the right maxillary permanent first molar. The sinus track was still detected on the buccal side of the tooth. Conservative endodontic treatment was performed using continuous wave technique, and composite (LuxaCore Z-Dual, DMG, Hamburg, Germany) was filled on the molar (Fig. 4A). On 3-month periodic recall check, the sinus track was still present as well as periapical radiolucency on the molar. Five months later, the sinus tract was closed, whereas radiolucency around the roots of the right maxillary first permanent molar was observed. The patient had not experienced pain or discomfort between visits. The tooth was subject to regular check-ups. On a 2-year check-up after extraction of the mandibular first molars, space closure of the extracted sites was confirmed with mild mesial inclination of mandibular second permanent molars on a panoramic radiograph and intraoral views (Fig. 5, 6). Periapical radiolucency was still observed on the endodontically treated maxillary first permanent molar without any clinical manifestation (Fig. 4B).
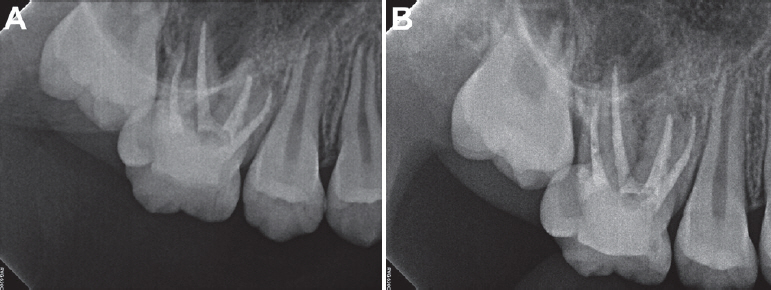
Periapical views of endodontically treated maxillary right permanent first molar (A) and the 2-year follow-up (B) in the first case.

Panoramic radiograph of the first patient (at the age of 12 years) showing favorable space closure accomplished by the eruption of permanent second molars 2 years after extraction and the tooth germ of left mandibular third molar.
2. Case 2
A 9-year-old girl came in with a chief complaint of severe pain on bilateral maxillary and mandibular first permanent molars. All 4 permanent first molars were percussion-sensitive but no clinical gingival swelling was observed. Periodontal pockets more than 5 mm were present on the distal surface of bilateral maxillary first permanent molars, whereas no pocket depth was measured on the mandible. No obvious tooth mobility was observed. On medical investigation, the patient was born 2 weeks earlier than her due date, resulting in getting intense care in the incubator. The patient was diagnosed with neonatal jaundice 16 days after birth, and was hospitalized for a month.
Radiographs including CBCT were taken in suspicion that the patient was affected by MIM. The roots of all 4 permanent first molars were turned out affected by MIM on the panorama radiograph (Fig. 7). Wedge shaped defects on the crown of maxillary permanent central incisors were found on the periapical standard film (Fig. 8A). The defects were pinched shape on the cervical third of the clinical crown on the intraoral view (Fig. 8B). Periodontal-endodontic lesions and periodontal bone loss around bilateral maxillary first permanent molars and the left mandibular first permanent molar were observed on CBCT view (Fig. 9). All 4 permanent first molars were diagnosed with symptomatic irreversible pulpitis due to periodontal inflammation. The patient had third molars in all 4 quadrants and the second permanent molars were on Demerjian’s dental formation stage F[6]. The all 4 MIM-affected molars were planned to be extracted expecting favorable space closure by eruption of the second molars, possibly followed by the third molars eruption[7]. Orthodontic interventions were considered in case the second permanent molars would erupt with mesial inclination. The affected molars were extracted and space closure was confirmed on the panorama (Fig. 10). Moderate inclination of both mandibular permanent second molars and a crown rotation of the left second molar were observed on a 2-year recall check (Fig. 11A, 11B).
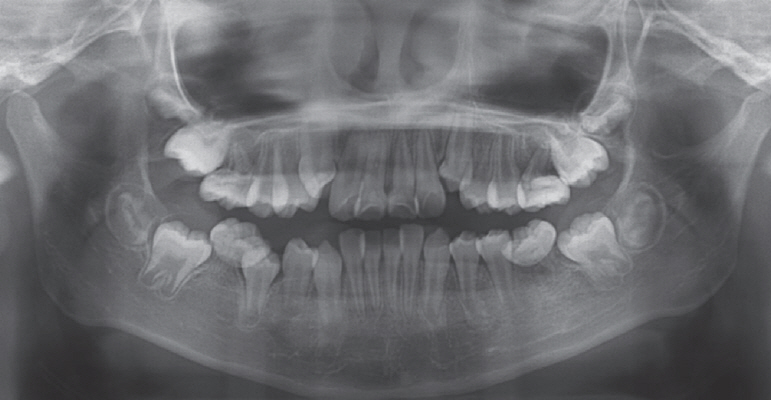
Panoramic radiograph of the second patient (at the age of 9 years and 6 months) showing abnormal root forms of bilateral maxillary permanent first molars and rudimentary roots of bilateral mandibular permanent first molars.
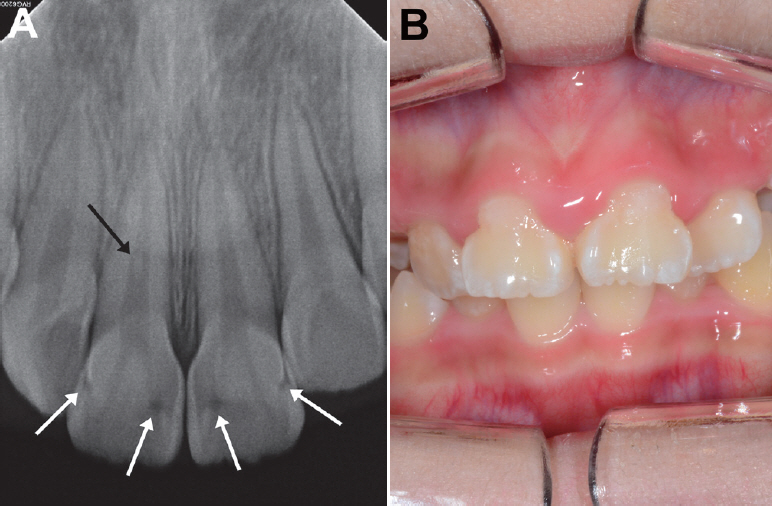
Maxillary central incisors of the second patient. (A) Periapical radiograph showing defects on the crown (white arrows) and a pulp stone on the right incisor (black arrow). (B) Intraoral view showing bell-shaped clinical crowns due to the defects on the cervical third area.
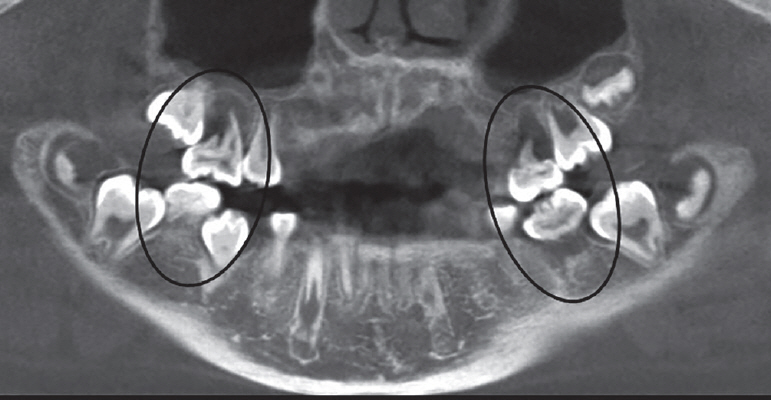
Cone-beam computed tomography image of the second patient showing malformed radicular roots and periapical lesions of permanent first molars (black circles).

Panoramic radiograph of the second patient 2 years after extraction (at the age of 11 years and 10 months) showing space closure of the extraction sites of 4 permanent first molars with mesial inclination in the mandible.
Ⅲ. Discussion
MIM was first termed by Lee et al.[1] in the case reports of 12 patients in 2014. Since 2014 when the malformation was first defined, cases of MIM had been reported along with the patients’ medical backgrounds. Majority of the patients had been hospitalized or treated due to premature birth, meningitis or brain-related diseases within 1 - 2 years after birth[1,4,8]. The two girls presented in this study were diagnosed with neonatal jaundice. Jaundice features yellow discoloration of the sclera and skin, which is caused by an increase in serum bilirubin levels resulting in accumulation of bilirubin in the tissues[9]. High levels of bilirubin could cause acute bilirubin toxicity and permanent brain damage[9]. Elevated serum levels of bilirubin during the dental development period could cause green discoloration in teeth[10]. Since jaundice is a condition that can affect the brain and dentition, neonatal jaundice seems in accordance with the medical issues which many MIM-affected patients have had. Neonatal jaundice the 2 patients had is not a rare systemic condition that could be present up to 80% among premature babies[9,11]. Jaundice in MIM affected patients was reported in previous case reports[4,8,12]. It has yet to be determined how jaundice and tooth malformation are interrelated. According to Centers for Disease Control and Prevention (U.S. Department of Health & Human Sciences, October 30, 2020)[13], preterm birth is when a baby is born before 37 weeks of pregnancy have been completed. Two patients in this study were born 2 weeks ahead of their estimated due dates. This was not severely premature condition considering that a full-term pregnancy is 40 weeks. There might be as yet unknown mechanism that led to MIM in spite of relatively mild medical histories.
Tooth root formation initiates after completion of tooth crown formation[14]. Crown completion of mandibular first permanent molars was accomplished around 3.51 and 3.69 years old in boys and girls respectively[15]. Approximate timing of initial root formation of mandibular first permanent molars was 4.17 and 3.65 years old in boys and girls respectively[15]. Based on the facts above, the timing does not seem to explain that early-life medical events or interventions may be linked to the etiology of MIM. There should be complicated and delicate factors or mechanisms underlying molar root and incisor crown formation that have not been explored. Hormonal changes or medication was one of the possible causal factors associated with a systemic disease[1,3]. There is another well-known molar-incisor related dental anomaly, molar-incisor-hypomineralization (MIH). MIH is observations of hypomineralized enamel surface on one or more permanent first molars and some of permanent incisors[16,17]. While the aspects of the two anomalies are totally different from each other, both MIM and MIH show malformations on the permanent first molars and permanent incisors. It is assumed that the tooth formation periods of these teeth might be interrelated.
Abscess caused by periodontal inflammation, gingival swelling, periapical bone resorption and severe pain are typical clinical findings of MIM-affected patients. Witt et al.[2] detected ectopic mineralized plates at the cemento-enamel junction (CEJ) level from the extracted molars, and named a cervical mineralized diaphragm (CMD). There were many soft tissue canals interspersed inside CMD and transmissions between CMD and the root furcation[1,2]. In Lee et al.[3] microscopic analysis, 3 layers were marked in the pulpal floor; upper, middle, and lower. A higher radiopacity, amorphous hard tissues and hyperactive cells were detected in the middle pulpal floor (MPF). These structures could be potential paths of pulp exposure and bacterial infection. This results in periodontal infection, which could eventually infect the pulp. If the symptoms were untreated, it would cause severe alveolar bone resorption and unfavorable prognosis of the affected tooth. In this respect, making efforts to maintain good periodontal health seems crucial for MIM-affected patients. Prophylactic measures would be regular dental check-ups, scaling and mindful care of oral hygiene including flossing at home.
The first patient was misdiagnosed with DD type Ⅰ at first visit. DD type Ⅰ is an autosomal hereditary disturbance affecting both deciduous and permanent teeth in the entire dentition[18-20]. DD type Ⅰ-affected teeth clinically look normal in shape and color, but the roots are short with a constricted pulp chamber that is parallel with CEJ[21]. MIM-affected teeth are mainly limited to permanent first molars, primary second molars and permanent maxillary central incisors. In a recent paper, affected permanent and deciduous canines were additionally reported[4]. One of the important microscopic features of MIM that is distinguished from DD type Ⅰ is the existence of CMD or MPF[2,3].
In case 1, the decision to wait and see for the right maxillary first permanent molar led to good results for the patient. Even though there was periapical radiolucency on the tooth, no clinical symptoms were present on the 2-year follow-up. Regular check-ups should be performed on the molar with a notification of the possibility of tooth extraction when the condition becomes worse. If the right permanent first molar would have to be removed, the second permanent molar could be guided to the first molar position. Some of the extraction space could be used to level the canine, since space did not seem enough for the right canine to be erupted. Both right maxillary and mandibular third molars were not observed on the radiograph at the time. Dental implants on both maxillary and mandibular second permanent molar positions may be needed for a better function of occlusion on the right posterior side. If the right maxillary permanent first molar is retained for a period of time with the maxillary second permanent molar being erupted, the second permanent molar may overerupt due to the absence of the opposing tooth. Splinting the second permanent molar with the adjacent teeth or an orthodontic appliance may be needed to prevent the molar from overerupting. Meanwhile, if the second permanent molar being erupted is locked under the distal contour of the MIM-affected first permanent molar, inserting a separator or using appliances such as Halterman would be considered. Comprehensive space management should be planed until a dental implant is implanted or another replacement is placed on the right mandibular second permanent molar position.
In case 2, the 4 permanent first molars were extracted without consideration of root canal treatment unlike case 1. The second permanent molars favorably erupted shifting to mesial and replaced the first molars. Kim et al.[22] reported a similar case in which the mandibular permanent first molars were removed due to MIM and the extraction sites were closed through eruption of the second permanent molars. In our cases, the dental developmental stage of the permanent second molars corresponded to stage E in case 1 and stage F in case 2 (Demirjian’s method)[6]. The ideal stage of development was stage E at the time of first permanent molars extraction[6,7]. Although 92% of maxillary extractions demonstrated complete space closure irrespective of second permanent molars development stage, only 66% of mandibular first permanent molars extracted at second permanent molars stage E showed complete space closure[7]. The ideal extraction timing of first permanent molars has not been clearly decided. Late removal of the first permanent molar would increase the risk of mesial tipping of the second permanent molar and result in spaces adjacent to the extracted region[23,24]. Early removal would cause a distal drifting or rotation of the second premolar, which could occupy the space for the second permanent molar to erupt[23,24]. Eichenberger et al.[25] researched the timing of extraction of permanent first molars to minimize clinical complications such as remaining gaps adjacent to the extracted region, tilting or rotation of the permanent second molars. The authors concluded that extraction should be performed between the ages of 8 and 11.5 for mandibular first permanent molars, whereas no solid conclusions were drawn concerning the maxillary first permanent molars[23,25]. When considering extraction of the first permanent molars, extraction in the maxilla is thought to be relatively free from clinical complications than in the mandible. The extraction of the first permanent molar should be performed at the right timing for successful eruption of the second permanent molar.
Mesial inclination of the second permanent molars seemed inevitable in our cases, especially in case 2. At the time of first permanent molar extraction, roots of the mandibular second permanent molars were more developed in case 2 than in case 1. The root length was less than the crown height in case 1, while the root length was equal to or longer than the crown height in case 2. The second molars of case 2 were almost supraosseous, whereas the ones of case 1 were intraosseous. These developmental conditions of the second permanent molars at the time of first molar extraction would be possible factors affecting their eruption in the future. Although space closure was fulfilled in both cases, the second permanent molar eruption was more favorable in case 1 than in case 2. Crown rotation was observed on the left mandibular second permanent molar in case 2. Mesially inclined and rotated second permanent molars might be corrected by the aid of orthodontic forces. Regular check-ups are needed to observe the progress of third molars eruption and their functional occlusion within the dentition.
MIM is now a dental anomaly with accumulated case descriptions. Brusevold et al.[5] cautiously speculated that prevalence of MIM could increase because newborns with medical issues previously mentioned, who might have not made it to life in the past, have been well treated and survived thanks to the development of health care. Clinicians should be aware of characteristics of MIM and be able to detect, diagnose and provide appropriate treatments. Since treatment guidelines for MIM-affected children have not been clearly established, whether to preserve or extract the affected molar is a difficult decision. Enforced molar extractions are performed when tooth prognosis is poor due to extensive caries or severe MIH[23,24]. Depending on the dentition stage of the affected child and the level of MIH severity, treatment plans would vary from preventative cares, restoration, endodontic treatment to extraction[24]. For MIM-affected children, if short, slender, rudimentary roots of permanent first molars are examined on radiographs, possible symptoms of MIM should be explained to the parents and the patients with emphasis of maintaining good periodontal health. Moreover, prophylactic oral hygiene care including flossing and scaling and regular check-ups should be stressed to prevent late detection of inflammation. Once pain is present and continuous, taking CBCT is recommended to scrutinize the anatomy of the affected tooth. If the symptomatic region seems endodontic-origin and the canal shapes are endodontically approachable, root canal treatment may be indicated[26]. Successful root canal treatment may ensure a good prognosis of the affected tooth[27,28]. When all canals were negotiated and filled, and vertical bone loss from the furcation was less than one third, a favorable prognosis was observed until 2 years post-treatment[28]. In Kim et al.[4] study, MIM-affected mandibular first permanent molars with endodontic-periodontal lesion were retained for 5 years after root canal treatment. If inflammation is severe and periodontal bone loss is destructive, extraction of the malformed molar would be the last choice. Before extraction, clinicians should examine the developmental stage of the second permanent molars, the existence of third molar tooth germs and the patient’s age. Depending on the conditions, molar extraction could be awaited until the right timing. The recommended timing for the first molar extraction was when a calcified point on the root bifurcation of the second permanent molar would appear on radiographs[23]. A beginning of calcification of third molars would be observed between 7 and 9 years old[29]. Depending on the time of extraction, favorable closure of extraction sites could be accomplished or not. In some cases, space management should be considered.
Ⅳ. Summary
This report described clinical management of 2 MIM-affected children and their 2-year follow-ups. Both patients had their permanent first molars extracted due to periodontal-endodontic inflammation and favorable space closure was accomplished through the eruption of the permanent second molars. Space management was required after extractions, and more observations would be needed on third molars eruption and their functional occlusion in the dentition. Root canal treatment was performed on the MIM-affected molar and the prognosis was favorable. Since MIM-affected patients are in mixed dentition and growing individuals, a correct diagnosis and appropriate treatments are important. When planning extraction of the affected molars, the timing of extraction and existence of third molar tooth germs are to be considered. Clinicians should be well informed of the symptoms and the progression of the anomaly to minimize pain and clinical complications.