치수재혈관화 술식에서 다양한 상아질 접착제가 치아 변색과 칼슘 실리케이트 시멘트의 밀폐 효과에 미치는 영향에 대한 실험실적 연구
An in Vitro Study of the Effects of Different Dentin Bonding Agents on the Prevention of Tooth Discoloration and the Sealing Ability of Calcium Silicate-Based Cement in Regenerative Endodontic Procedures
Article information
Abstract
본 연구는 치수 재혈관화 과정 중 상아질 접착제 도포 유무 및 종류가 치아 변색과 미세 누출에 미치는 영향을 평가하고자 하였다. 시편은 사람의 발거된 소구치 120개로 제작하였으며, 상아질 접착제 종류에 따라 다음과 같이 분류하였다. Group I. No bonding; Group II. One-Step; Group III. Clearfil SE Bond; Group IV. Single Bond Universal. 각 그룹은 칼슘 규산염계 시멘트인 Endocem MTA® Premixed Regular와 Biodentine의 사용에 따라 Subgroup a와 Subgroup b로 나뉘어 총 8개의 그룹으로 분류되었다. 치관변색 평가를 위해 초진(S0), 항생제 도포 1주(S1), 2주(S2), 4주 경과(S3)와 칼슘 규산염계 시멘트 적용 2주 경과(S4) 각 시점에서 사진을 촬영해 CIE L*a*b*를 측정하였다. 모든 시편은 2% 메틸렌 블루 용액에 침적 후 30배율로 관찰하여 미세누출을 평가하였다. 상아질 접착제 도포는 치관 변색을 감소시켰고, Biodentine은 상아질 접착제의 도포 유무 및 종류와 상관없이 최소한의 변색을 보였다. 또한 상아질 접착제 도포는 미세 누출을 증가시키지 않았다.
Trans Abstract
This study aimed to compare the effects of applying different types of dentin bonding agents (DBAs) on tooth and on the sealing ability of CSC in regenerative endodontic procedures (REPs). Specimens were made from 120 human first premolars and categorized into the following groups based on the presence and the type of DBA: Group I, no bonding; Group II, One-Step; Group III, Clearfil SE Bond; and Group IV, Single Bond Universal. Subsequently, the groups were categorized into Subgroup a and Subgroup b, in which Endocem MTA® Premixed Regular and Biodentine were used, respectively. The CIE L*a*b* on the photos taken prior to TAP placement (S0), 1 week after TAP placement (S1), 2 weeks after TAP placement (S2), 4 weeks after TAP placement (S3) and 2 weeks after CSC placement (S4) was used to assess discoloration. The samples were submerged in a 2% methylene blue solution and magnified by 30 times under a stereomicroscope to assess microleakage. The application of DBA during REP reduced crown discoloration, while Biodentine showed minimal discoloration with or without DBA and regardless of the DBA type. Additionally, the application of DBA did not increase microleakage.
Introduction
Regenerative endodontic procedure (REP) is aimed at the treatment of necrotic immature teeth[1]. The root canal is generally disinfected using triple antibiotic paste (TAP), which contains ciprofloxacin, metronidazole, and minocycline. Following disinfection, a blood clot or platelet-rich plasma/fibrin is induced and sealed with a bioactive substance like mineral trioxide aggregate (MTA)[2]. These procedures promote root length and thickness growth in immature permanent teeth[1,3]. Creating an antibacterial environment inside the root canal and an effective coronal seal are necessary for a better prognosis[2,4].
Coronal discoloration of teeth following REP, however, is a detrimental result [5,6]. The main cause of discoloration is the semisynthetic tetracycline derivative minocycline. It forms an insoluble compound by chelating calcium ions, which is then integrated into the tooth matrix to create discoloration[7]. Additionally, a number of studies have documented unfavorable tooth discoloration following MTA use[8,9]. This is a result of the chemical interaction between bismuth oxide, MTA components, and dentin matrix collagen[10].
To minimize the risk of coronal discoloration, the American Association of Endodontists (AAE) clinical considerations suggest the use of a double antibiotic paste containing ciprofloxacin and metronidazole. Furthermore, the European Society of Endodontology position statement suggests the use of a non-discoloring calcium hydroxide as an intracanal medicament[11]. TAP, on the other hand, is still recommended by the AAE clinical considerations since it has been demonstrated to be the most effective in removing bacteria within the dentinal tubules[12]. The AAE clinical considerations for REPs recommend using a dentin bonding agent (DBA) and calcium silicate-based cements (CSCs) as an alternative to MTA to cover the blood clot[2].
There are two main types of dentin bonding procedures: etch-and-rinse and self-etch. The etch-and-rinse technique uses 30 - 40% phosphoric acid to remove the smear layer adhering to the enamel and dentin prior to application, and is rinsed with plenty of water to open the dentinal tubules. To dissolve the smear layer and demineralize a portion of the underlying dentinal surface, a primer containing an acidic monomer is used in the self-etch process. It is allowed to polymerize without being washed off, so that the resin remains embedded in the dentinal surface, including the smear layer, and forms an adhesive interface.
CSC is a material used to compensate for the disadvantages of MTA, such as discoloration, long setting time, and difficult handling. It contains CaO, SO3, P2O5, and SiO2 but not bismuth oxide; thus, its discoloration potential is significantly lower than that of MTA[13,14].
Several studies have reported that the application of DBA in REPs reduced coronal discoloration caused by TAP and CSC[15]. However, this can affect the sealing ability of the CSC because the latter is mechanically and chemically bonded to the tooth. After the setting process, micromechanical tags are created by attaching calcium carbonate crystals into dentinal tubules. Micromechanical tags aid in the material’s bonding to the tooth structure[16]. CSC chemically interacts with dentin to generate a hydroxyapatite-like structure that attaches to the dentinal walls[17]. Thus, DBA may interfere with the calcium-releasing capability or sealing ability of CSC. However, to the best of our knowledge, there are no specific guidelines on how or what type of DBA to apply. Furthermore, there are no reports on the impact of the DBA application on microleakage.
Therefore, this study aimed to evaluate the effect of applying DBA using the etch-and-rinse and self-etch techniques on coronal discoloration caused by TAP and two types of CSCs and on the sealing ability of CSCs.
Materials and Methods
The protocol was approved by the Institutional Review Board of Kyungpook National University Dental Hospital (Approval No. KNUDH-2023-01-01-00).
1. Subjects
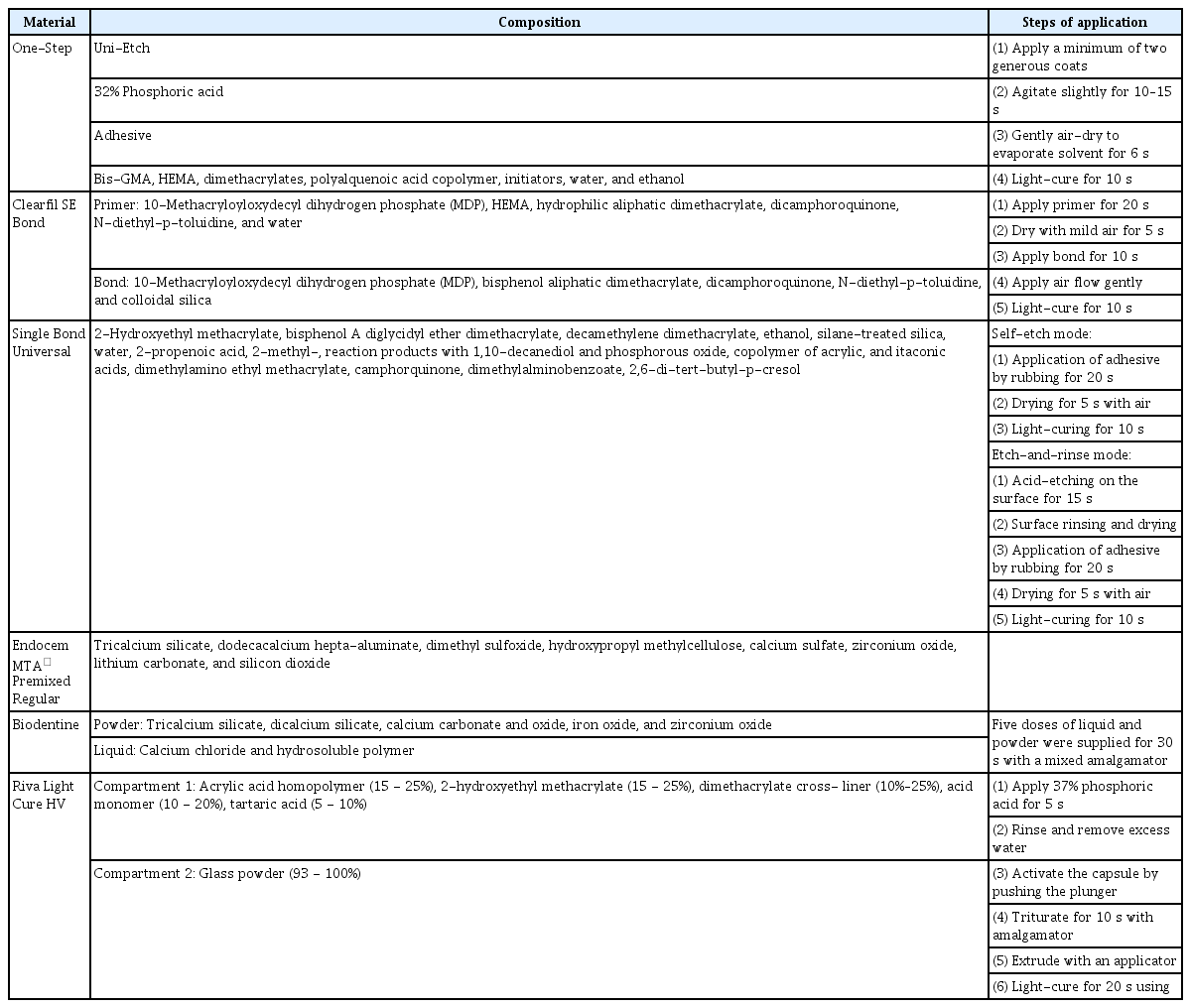
In this study, the three types of DBA used were One-Step (BISCO, Inc., Schaumburg, IL, USA; etch-and-rinse), Clearfil SE Bond (Kuraray Noritake Dental, Inc., Okayama, Japan; self-etch), and Single Bond Universal (3M ESPE, St. Paul, MN, USA; self-etch mode). The two types of CSC were Endocem MTA® Premixed Regular (EMPR, Maruchi, Wonju, Korea) and Biodentine (Septodont, Saint-Maur-des-Fossès Cedex, France). Riva Light Cure HV (SDI company, Victoria, Australia), a resin-modified glass ionomer cement, was used as a restorative material. Details of the study materials are presented in Table 1.
2. Methods
1) Sample preparation
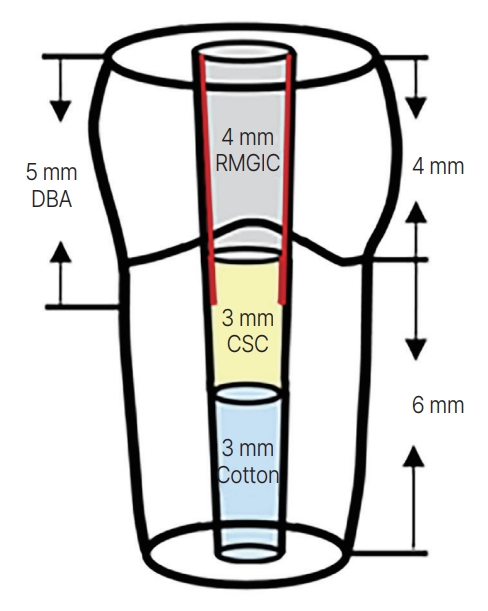
According to the orthodontic treatment plan, a total of 120 human mandibular premolars were extracted. The teeth were placed in a physiologic saline solution until usage. They were clinically and radiographically examined to be free of caries, intrinsic or extrinsic discolorations, cracks, restoration, developmental anomalies, and calcification. Specimens were fabricated, as illustrated in Fig. 1. Each specimen’s crown was resected to achieve a standardized crown length of 4 mm above the labial cemento-enamel junction (CEJ), and the apical part was resected to achieve a standardized root length of 6 mm below the labial CEJ. The root apical areas were sealed with utility wax and embedded in self-curing acrylic resin (Vertex; Vertex dental, Soesterberg, Netherlands). Subsequently, the pulp chambers were prepared with a diamond bur (No. 237) to a depth of 4 mm and a width of 2.1 mm. The internal walls of the pulp chamber were gently debrided with NiTi-file (ProTaper Gold F5; Dentsply Sirona, Bensheim, Germany). After the final irrigation with 17% ethylenediaminetetraacetic acid (EDTA), the pulp chambers were dried using paper points.
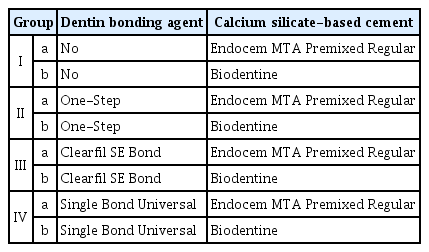
2) Experimental setup
The specimens were randomly divided into four groups (n = 30) according to the presence and the type of DBA prior to TAP placement (Table 2). To reproduce and control the downward flow of the DBA during the air blowing process after its application, which affects the CSC-tooth interface, DBA was applied a total of 5 mm from the crown to 1 mm below the labial CEJ on Groups II - IV according to the manufacturer’s protocol. Single Bond Universal used in Group IV was used in self-etch mode. Triple antibiotic paste was made in all groups by combining equal parts ciprofloxacin, metronidazole, and minocycline (1 : 1 : 1) with saline to a final concentration of 0.1 mg/mL, ensuring that the solution was limited to the root canal beneath the labial CEJ with 1 ml syringe. The access cavities were filled with a temporary filling material (Caviton; GC Corp., Tokyo, Japan). The specimens were incubated for 4 weeks at room temperature with 100% saturation in humidity. The Caviton was then removed, the root canals were irrigated with 20 mL 17% EDTA and dried using paper points. In Groups II - IV, DBA was reapplied to the access cavity walls in the same way as the initial application to address the potential for previous DBA layer deterioration during the removal of temporary filling material. In all groups, the root canals were then filled with cotton until 3 mm below the labial CEJ to simulate a blood clot, standardize the coronal barrier thickness, facilitate material condensation, and prevent the material from moving toward the apical region. A periodontal probe was used to gauge the extent of the remaining space for restoration with reference to the labial CEJ. Then, each group was further randomly divided into two subgroups (n = 15) and labeled according to the type of CSC applied (Table 2). For Subgroup a, EMPR was applied, whereas for Subgroup b, Biodentine was used. Considering the risk of inhomogeneous mixing, the Biodentine capsule was triturated using an Ultramat S Mixer (SDI, Victoria, Australia), and then a Centrix syringe gun (Shinwoo Dental, Anyang, Korea) was used. EMPR was selected as the premixed type. Each material was prepared in accordance with the manufacturer’s instructions and placed on the cotton in a homogeneous layer about 3 mm below the labial CEJ. The CSCs were subsequently covered with a cotton pellet soaked with saline, and the cavity was sealed with Caviton for a day. After removing Caviton and the DBA in the access cavity using the bur, Riva Light Cure HV was applied in 4 mm thickness to cover the canal orifice. All the specimens were immersed in saline at room temperature for 2 weeks. The experimental process is illustrated in Fig. 2.
3) Measurement of tooth discoloration
A circle with a diameter of 3 mm was evaluated on the cervical and middle thirds of the crowns for repeatable color assessment, with two-thirds of its height in the cervical and one-third in the middle third of the tooth crown[18]. All digital images were taken under standard desiccation and lighting conditions by the same operator. The lighting was standardized using a PhotoBox (Daehan, Osan, Korea). Photos were taken using a digital camera (Canon EOS 100D; Canon Inc., Tokyo, Japan) held 20 cm away from the subject and a 100 mm macro lens (Canon EF 100 mm F 2.8 macro USM) under controlled lighting conditions (exposure: 1/200 s, aperture: F/22, white balance flash: 5500)[9]. The images were imported into Adobe Photoshop CS6 for shade analysis with the CIE L*a*b*. L* indicates the value of lightness/darkness; a*, greenness-redness; and b*, blueness-yellowness[19]. The color measurements were performed three times inside the marked circle using the five steps presented below, and the mean value was recorded.
S0: prior to TAP placement as the baseline color
S1: 1 week after TAP placement
S2: 2 weeks after TAP placement
S3: 4 weeks after TAP placement
S4: 2 weeks after CSC placement (after a total of 6 weeks)
The color change (ΔEab) between the baseline (S0) and the other steps (S1, S2, S3, and S4) was calculated as follows:
ΔEab ≥ 3.3 was considered clinically unacceptable[20].
4) Microleakage evaluation
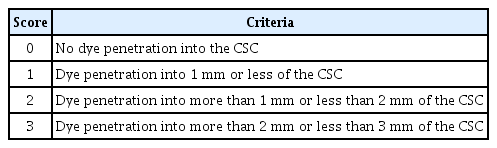
All specimens were immersed in water baths at 5°C for 30 s, and a total of 1500 rounds were performed at 2 weeks after CSC placement[21]. One day after thermocycling procedures, nail varnish was applied to the whole surface of the teeth excluding the restorative surface and the surrounding 1.0 mm. To assess microleakage, all specimens were immersed in a 2% methylene blue solution for a day before being rinsed and dried. They were then buccolingually sectioned with a TechCut 4 TM Low-Speed Saw (Allied, Rancho Dominguez, USA) to acquire two specimens for each tooth. The acquired specimens were examined under a 30 magnification stereoscopic microscope. Each specimen’s dye penetration was rated from 0 to 3 (Table 3, Fig. 3) and then categorized and measured according to the criteria. The higher score was recorded after examining two specimens from the same tooth.
5) Statistical analysis
The SPSS version 20.0 (IBM SPSS Inc., Chicago, IL, USA) program was used for the statistical analysis. Using the Kolmogorov-Smirnov test, the normality of the data distribution was evaluated. Furthermore, the Kruskal-Wallis test was used to evaluate the effect of DBA application on tooth discoloration. The Mann-Whitney U test was used as a post hoc test. To evaluate the discoloration caused by TAP, we compared the changes in S1, S2, and S3 with those in S0 in Groups I, II, III, and IV. To evaluate the discoloration caused by CSC, the changes between S3 and S4 in each subgroup were compared. The microleakage scores of each subgroup were compared using the Mann-Whitney U test. p < 0.05 was considered to indicate statistical significance.
Results
1. Measurement of tooth discoloration
1) Discoloration due to TAP
The mean L* value of the entire specimens was 99.14 ± 0.58, the mean a* value was -1.43 ± 0.69, and the mean b* value was 7.08 ± 3.72 at S0. After TAP application, discoloration over time is shown in Fig. 4. Group I was statistically significantly different from Groups II, III, and IV in each period (S1 - S3). No statistical significance was found when analyzing Groups II - IV to compare the discoloration effects by DBA type (Table 4, Fig. 5, p > 0.05).

Photographs of discoloration on specimens over time after TAP application. (1) No bonding, (2) One-Step, (3) Clearfil SE Bond, (4) Single Bond Universal, (A) Baseline (S0), (B) 1 week after TAP placement (S1), (C) 2 weeks after TAP placement (S2), (D) 4 weeks after TAP placement (S3).
S0: prior to triple antibiotic paste (TAP) placement as the baseline color; S1: 1 week after TAP placement; S2: 2 weeks after TAP placement; S3: 4 weeks after TAP placement.
2) Discoloration caused by CSC
The ΔE values of 2 weeks after EMPR and Biodentine application are shown in Table 5 and Fig. 6. For EMPR, Group Ia was statistically significantly different from Groups IIa, IIIa, and IVa, respectively (p < 0.05). There was statistical significance between Subgroup IIa with One-Step and Subgroup IVa with Single Bond Universal when IIa, IIIa, and IVa were analyzed to determine the differences by DBA type (p > 0.05).

Comparison of crown discoloration depending on the dentin bonding agent type after the application of Endocem MTA Premixed Regular and Biodentine
For Biodentine, on the other hand, Group Ib did not show statistical significance with Group IIb, IIIb, and IVb, respectively (p > 0.05). Subgroups IIb, IIIb, and IVb were analyzed to assess differences by DBA type, but no statistical significance was observed (p > 0.05).
2. Evaluation of microleakage
The effect of DBA application on microleakage at the tooth-CSC interface was evaluated. About 47.5% (n = 57) of the dye penetration was confined to RMGI restorations (Score 0), 45.8% was within 1 mm of the CSC (Score 1), and 6.6% was within 1 - 2 mm of the CSC (Score 2); microleakage greater than 2 mm of the CSC (Score 3) was not observed (Table 6).
Subgroups Ia - IVa were analyzed, respectively, to compare the sealing ability of EMPR with and without DBA application and the type of DBA; no statistical significance was observed (p > 0.05). Furthermore, to evaluate the sealing ability of Biodentine according to with and without DBA application and the type of DBA, Subgroups Ib - IVb were analyzed in the same way as before; no statistical significance was observed in all groups (p > 0.05).
Discussion
To measure color changes, a variety of techniques have been used in the literature, including visual techniques, spectrophotometers, colorimeters, and digital photograph analysis. Although the most commonly used technique for color measurements continues to be spectrophotometric analysis, some research evaluating coronal discoloration has adopted the digital image analysis method[22-24]. Comparing digital and spectrophotometric approaches for shade selection, previous studies came to the conclusion that both are trustworthy because the results from the digital method correlated with those from the spectrophotometer[25-27]. When compared to spectrophotometers or colorimeters, the advantages of the digital image analysis method include cost effectiveness, time savings, and convenience[27]. Therefore, in this study, crown discoloration was evaluated by the digital image analysis method.
In this experiment, the results indicated that the application of DBA is effective in preventing discoloration at 1, 2, and 4 weeks following TAP placement. Applying DBA to the dentinal walls of the pulp chamber reduces the interaction between minocycline and dentin, which prevents the insoluble complex that minocycline forms when it binds to calcium ions via chelation and is absorbed into the tooth matrix through discoloration[7].
This finding is consistent with that in previous study showing that DBA application reduces discoloration caused by TAP. According to Morresi et al.[28], in their experiments on TAP-induced tooth discoloration with and without the use of DBA, the ΔEab values after 4 weeks were 25 - 30 in the No DBA group and about 15 in the DBA group. The ΔEab values in our experiment were lower than these values, but a similar tendency was observed. According to Kim et al.[5], the use of Adhese (Ivoclar Vivadent, Schaan, Liechtenstein), a light-curing, self-etching, two-component adhesive dentin bonding system, prior to TAP placement during revascularization resulted in a mean ΔEab value of 13.7 ± 3.4 after 2 weeks. Two single-step restorative materials, namely, OptiBond All-In-One (KERR, Orange, CA, USA) and RelyX U200 TR (3M ESPE, Seefeld, Germany), were also applied prior to TAP placement, which resulted in a significant reduction in discoloration after 4 weeks[29].
We used several DBA types with different bonding systems to compare their efficacy in preventing tooth discoloration; however, most of them did not exhibit significant differences. However, the use of One-Step resulted in less discoloration compared with that of Single Bond Universal at 2 weeks after EMPR application. It is important to avoid contact with dentin to prevent staining, as minocycline chelates with calcium ions in dentin to form insoluble complexes that cause discoloration[7]. However, consistent with our results, previous studies have shown that applying DBA does not completely prevent minocycline-induced discoloration, with ΔE ≥ 3.3[5]. In other words, the sealing ability of the DBA application is not completely achieved on the surface. Therefore, the degree of sealing in the dentinal tubule may be compared next. After application of the etch and rinse system and the self-etch system, field-emission scanning electron micrographs showed that the etch and rinse system resulted in deep, distinct, and elongated resin tags in the dentinal tubules, whereas the self-etch system resulted in resin penetration within the smear layer and smear plug[30]. This suggests that the total etch adhesive can effectively prevent the penetration of minocycline and may explain the low ΔE value of One-Step in this result. However, it is considered a limitation of this study that Single Bond Universal is composed of one-bottle, which has low technique sensitivity, and One-Step is difficult to reproduce clinically identical wet-bonding.
Clinically, regardless of the DBA type, less coronal discoloration would result from REP if DBA were applied to the dentinal walls of the pulp chamber. This is because DBA would reduce the interaction between minocycline/dentin, bismuth oxide/collagen, and erythrocyte access into the dentinal tubules. Furthermore, when access cavity walls are covered in DBA, it is simple to clean if they get contaminated with TAP or blood[28].
About 2 weeks after the application of EMPR, the use of DBA significantly reduced coronal discoloration. There are no previous studies evaluating the difference in discoloration of EMPR with or without a DBA, but there is a study on Retro MTA, a type of CSC. When coronal discoloration was evaluated 4 weeks after the application of Retro MTA, the No DBA group had an ΔEab value of 21.84, whereas the DBA group had 8.40[31]. This indicates that the application of DBA was effective in preventing discoloration caused by CSC, which is consistent with the results of this study.
Biodentine did not exhibit any difference in discoloration between the DBA group (mean ΔEab = 2.56) and the No DBA group (mean ΔEab = 2.62). This result is contrary to EMPR, which is thought to be due to differences in the composition of the two types of CSCs. One study evaluated tooth discoloration at various phases of calcium aluminate cement and found that dodecacalcium heptaaluminate, a component of EMPR, showed ΔEab value of 4.5 ± 4.8 at 15 days[32]. Compared to the study that the Δ Eab ≤ 3.3 after 4 weeks of Biodentine application without DBA[33], these results suggest that the low discoloration level of Biodentine itself is lower than EMPR; thus, the presence or absence of DBA did not have a significant effect. In addition, previous study has demonstrated that the presence or absence of DBA prior to Biodentine application has no significant effect on tooth discoloration[28]. In addition, studies have shown that the porosity, fluid uptake, and sorption value of bioceramics are positively correlated with discoloration[34]. If EMPR has these properties, the potential for discoloration from minocycline is high, and further research on material properties is needed.
The aforementioned ΔEab values were lower than those in the previous study, which was 10.63 for ProRoot MTA after 4 weeks of application[31]. In other words, using CSC instead of MTA could prevent discoloration in REPs. This may be due to the difference in their compositions, as compared with MTA, CSC does not contain iron and bismuth oxide[35].
Microleakage at the tooth-restoration interface is anticipated to have a major impact on the longevity of the restoration. The development of secondary caries may be started by microleakage from restoration, which would eventually result in treatment failure. To evaluate microleakage, two different interfaces must be analyzed: 1) the tooth-DBA interface and 2) the adhesive-bioceramics interface. One of the factors that can affect the tooth-adhesive interface is the DBA type. Previous studies have demonstrated that the self-etch technique is superior to the etch-and-rinse technique in terms of dentin-to-tooth bond strength[36-38]. Host-derived matrix metalloproteinases (MMPs), acting slowly, cause collagen matrixes to degrade on their own within hybrid layers made by contemporary dentin bonding systems[30,39]. The faster degradation of hybrid layers reported in etch-and-rinse bonds appears to correlate with the usually greater degree of MMP activity observed in etch-and-rinse adhesives compared to self-etch adhesives[40]. The factor that can affect the adhesive-bioceramics interface is the pH of the DBA. One-Step has a pH of 4.6; Clearfil SE Bond, 2.0; and Single Bond Universal, 2.7. Although the manufacturer claims that the pH increases after curing, even if the DBA is cured, an acidic environment is formed due to unreacted monomers in the oxygen inhibition layer[41]. The placement of CSCs in a low-pH environment may affect their physical and chemical properties[42,43]. Acidic environments prevent the complete setting of bioceramic cement, increase the setting time, and increase porosity, which increases solubility and decreases microhardness[42,44-46]. Acidic environments are more prone to disrupt the synthesis of hydroxyapatite crystals and the consequent production of a hybrid layer at the CSC-dentin interface[47]. These two factors can lead to contradicting results for different types of adhesives at each interface.
In the microleakage evaluation conducted in this study, the access cavity was filled with 4 mm thick RMGI after the removal of the DBA according to the AAE clinical considerations[2]. As a result, this study found that the presence or absence of an adhesive and the type of adhesive had no statistically significant effect on the sealing ability of the CSC. In particular, 47.5% of the total samples did not reach the CSC layer in the microleakage evaluation. This indicates that a significant portion of sealing was achieved in the RMGI restoration. Thus, it can be deduced that the sealing ability provided by the restorative material outweighs the effect of the DBA application on the CSC sealing ability. Therefore, restoration should be carefully considered to achieve sufficient sealing. In clinical practice, composite resin is generally used for restoration. Particularly in the development of DBAs, which improve adhesion, the presence or absence of DBA is thought to have a relatively low impact on the sealing ability of the CSC. Temporary restoration is a required thickness of at least 4 mm to achieve clinically sufficient sealing ability[48]. In the anterior and premolar teeth, the AAE clinical considerations[2] recommend 3 mm of CSC, followed by bonding of a filled composite to the beveled enamel margin, and in the molar teeth, 3 mm of MTA, followed by RMGI, composite, or alloy.
However, because the dye penetration method only measures the degree of leakage in one plane, calculating the total amount of leakage is impossible[49,50]. The pH and chemical reactivity of dyes can also affect dye penetration[51]. The characteristics and surface morphology of these cements at each interface were not evaluated in this study. Thus, it is recommended that scanning electron microscopy evaluation be performed in future studies to clearly elucidate the increases and/or decreases in the degree of microleakage[52].
This study is significant in that it is the first to compare the efficacy of different DBA types in preventing discoloration in REPs and to evaluate the sealing ability of CSC, to the best of our knowledge. The results of this study indicated that sealing of the dentinal walls with DBA significantly reduced coronal discoloration caused by TAP and CSC; however, the type of DBA does not have an effect on the prevention of discoloration. No significant differences were also observed in microleakage.
This study has the following limitations: First, because the experimental design was based on clinical processes, the CSCs were applied to the specimens with TAP. Therefore, the values used to evaluate discoloration after CSC application (S4-S3) included both the discoloration of TAP and the discoloration of CSCs. Further studies should include an additional control group with TAP and without CSCs to evaluate discoloration caused by CSCs. In addition, because this study only evaluated the color change over a 2-week period, a long-term evaluation is needed. Second, inducing bleeding and blood clot formation in the root canal is a further stage in REP, which is done after placing endodontic cements below the CEJ to seal the blood clot[15,53]. Among the proposed mechanisms of tooth discoloration in REPs are erythrocyte penetration into the tooth structure[9] and the accumulation of hematin and hemoglobin within dentinal tubules[54]. However, this study did not evaluate the discoloration potential when contaminated with blood. Third, the outcomes of this study should be carefully considered because other CSCs are available on the market but were not included here. Furthermore, the cytotoxicity of the DBA monomer could affect the pulp tissue[55]. Thus, further study focusing on the scope of the DBA application is warranted.
Conclusion
The application of DBA effectively prevented the discoloration caused by TAP. The use of CSC instead of MTA was supposed to reduce discoloration in REP. Although some significant differences were observed in the prevention of discoloration by DBA type, there was a general trend of no difference. In addition, the application of DBA did not significantly increase the degree of microleakage.
Notes
Conflict of Interest
The authors have no potential conflicts of interest to disclose.