1. Andreason JO, Andreason FM, Andersson L : Textbook and Color Atlas of Traumatic Injuires to the Teeth. 5th ed. John Wiley & Sons, Hoboken, 2018.
2. Andersson L, Andreasen JO, Day P, Heithersay G, Trope M, DiAngelis AJ, Kenny DJ, Sigurdsson A, Bourguignon C, Flores MT, Hicks ML, Lenzi AR, Malmgren B, Moule AJ, Tsukiboshi M : International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teeth.
Dent Traumatol, 28:88-96, 2012.


3. Anderason J, Borum MK, Jacobsen H, Anderasen FM : Replantation of 400 avulsed permanent incisors.
Endod Dent Traumatol, 11:76-89, 1995.

4. Ahn HJ, Nam OH, Lee HS, Kim EC, Cohenca N, Choi SC : Expression of inflammatory cytokines and MMPs on replanted teeth at different extra-alveolar time: an ex vivo and in vivo study.
Int J Pediatr Dent, 26:301-309, 2016.

5. Hiremath G, Kidiyoor KH : Avulsion and storage media.
J Investig Clin Dent, 2:89-94, 2011.


6. Subramaniam P, Girija P, Eswara U, Girish Babu KL : Oral rehydration salt-liquid as a storage medium for avulsed tooth.
Dent Traumatol, 31:62-66, 2015.


7. Siddiqui F, Karkare S : Storage media for an avulsed tooth: nature to the rescue. Br J Med Health Res, 1:1-10, 2014.
8. Poi WR, Sonoda CK, Martins CM, Melo ME, Pellizzer EP, de Mendonca MR, Panzarini SR : Storage media for avulsed teeth: a literature review.
Braz Dent J, 24:437-445, 2013.


9. Rajakeerthi R, Nivedhitha MS : Natural Product as the Storage medium for an avulsed tooth - A Systematic Review.
Cumhur Dent J, 22:249-256, 2019.

10. Jain D, Nagarajappa S, Dasar PL : Natural products as storage media for avulsed tooth.
Saudi Endod J, 5:107, 2015.

11. Hwang JY, Choi SC, Park JH, Kang SW : The use of green tea extract as a storage medium for the avulsed tooth.
J Endod, 37:962-967, 2011.


12. Özan F, Polat ZA, Er K, Özan Ü, Değer O : Effect of propolis on survival of periodontal ligament cells: new storage media for avulsed teeth.
J Endod, 33:570-573, 2007.


14. Squadrito F, Bitto A, Irrera N, Pizzino G, Pallio G, Minutoli L, Altavilla D : Pharmacological activity and clinical use of PDRN.
Front Pharmacol, 8:224, 2017.



15. Guizzardi S, Martini D, Bacchelli B, Valdatta L, Thione A, Scamoni S, Uggeri J, Ruggeri A : Effects of heat deproteinate bone and polynucleotides on bone regeneration: an experimental study on rat.
Micron, 38:722-728, 2007.


16. Pallio G, Bitto A, Pizzino G, Galfo F, Irrera N, Squadrito F, Squadrito G, Pallio S, Anastasi GP, Cutroneo G, Macri A, Altavilla D : Adenosine receptor stimulation by polydeoxyribonucleotide improves tissue repair and symptomology in experimental colitis.
Front Pharmacol, 7:273, 2016.



17. Jeong EK, Jang HJ, Kim SS, Lee SY, Oh MY, Kim HJ, Eom DW, Ham JY, Han DJ : Protective effect of polydeoxyribonucleotide against renal ischemia-reperfusion injury in mice.
Transplant Proc, 48:1251-1257, 2016.


18. Bizzoca D, Brunetti G, Moretti L, Piazzolla A, Vicenti G, Moretti FL, Solarino G, Moretti B : Polydeoxyribonucleotide in the Treatment of Tendon Disorders, from Basic Science to Clinical Practice: A Systematic Review.
Int J Mol Sci, 24:4582, 2023.



19. Yang CY, Ha JS, Lee WS, Bae JS, Lee CW, Jeong EH, Kim GH, Park KH : The effect of wound healing of Nile tilapia (Oreochromis niloticus) using PDRN (polydeoxyribonucleotide) extracted from seaweed (Porphyra sp. J Fish Pathol, 34:233-241, 2021.
20. Song MH, Choi MH, Jeong JH, Lee SS, Jeong WY : Efficiency of PDRN (Polydeoxyribonucleotide) extraction from various plants species and its in vitro wound healing activity. J Korea Inst Inf Electr Commun Technol, 15:387-395, 2022.
21. Castellini C, Belletti S, Govoni P, Guizzardi S : Anti inflammatory property of PDRN - an in vitro study on cultured macrophages. Adv Biosci Biotechnol, 8:13-26, 2017.
22. Bitto A, Polito F, Irrera N, D’Ascola A, Avenoso A, Nastasi G, Campo GM, Micali A, Bagnato G, Minutoli L, Marini H, Rinaldi M, Squadrito F, Altavilla D : Polydeoxyribonucleotide reduces cytokine production and the severity of collagen-induced arthritis by stimulation of adenosine A2A receptor.
Arthritis Rheum, 63:3364-3371, 2011.


25. Jung J, Lim HS, Lee DW : Polydeoxyribonucleotide, as a novel approach for the management of medication-related osteonecrosis of the jaw: A preliminary observational study. J Korean Dent Sci, 11:57-61, 2018.
28. Spinas E, Generali L, Mameli A, Demontis C, Martinelli D, Giannetti L : Delayed tooth replantation and inflammatory root resorption in childhood and adolescence.
J Biol Regul Homeost Agents, 33:623-627, 2019.

29. Keum KY, Kwon OT, Spängberg LS, Kim CK, Kim J, Cho MI, Lee SJ : Effect of dexamethasone on root resorption after delayed replantation of rat tooth.
J Endod, 29:810-813, 2003.


30. Colangelo MT, Galli C, Guizzrdi S : The effects of polydeoxyribonucleotide on wound healing and tissue regeneration: a systematic review of the literature.
Regen Med, 2020 Aug 6. doi:
10.2217/rme-2019-0118. Online ahead of print

32. Kim TH, Heo SY, Oh GW, Heo SJ, Jung WK : Applications of Marine Organism-Derived Polydeoxyribonucleotide: Its Potential in Biomedical Engineering.
Mar Drugs, 19:296, 2021.



33. Colangelo MT, Galli C, Guizzardi S : Polydeoxyribonucleotide Regulation of Inflammation.
Adv Wound Care, 9:576-589, 2020.

34. Ceravolo I, Mannino F, Irrera N, Minutoli L, Arcoraci V, Altavilla D, Cavallini GM, Guarini S, Squadrito F, Pallio G : Beneficial Effects of Polydeoxyribonucleotide (PDRN) in an In Vitro Model of Fuchs Endothelial Corneal Dystrophy.
Pharmaceuticals, 15:447, 2022.



35. Thellung S, Florio T, Maragliano A, Cattarini G, Schettini G : Polydeoxyribonucleotides enhance the proliferation of human skin fibroblasts: involvement of A2 purinergic receptor subtypes.
Life Sci, 64:1661-1674, 1999.


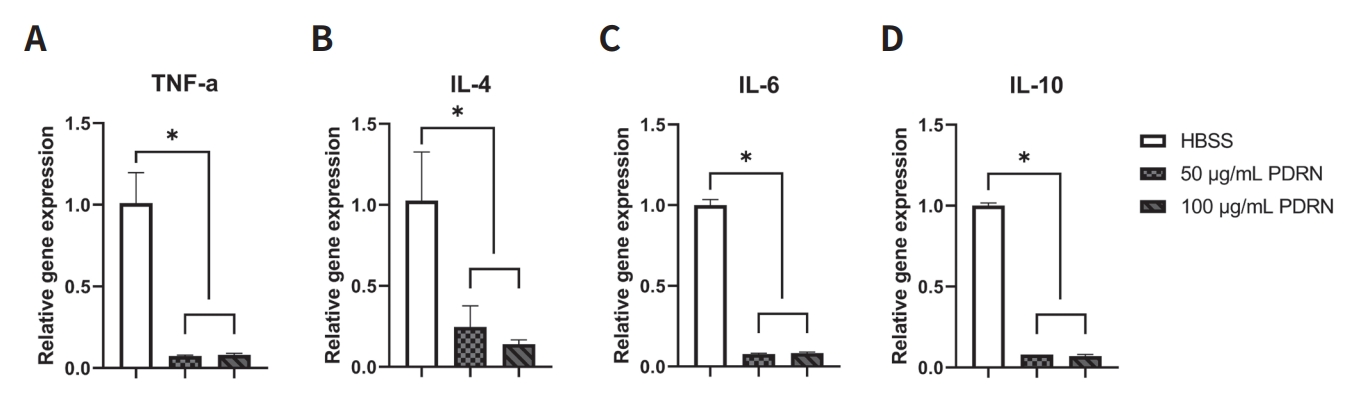
36. Han JH, Jung J, Hwang L, Ko IG, Nam OH, Kim MS, Lee JW, Choi BJ, Lee DW : Anti-inflammatory effect of polydeoxyribonucleotide on zoledronic acid-pretreated and lipopolysaccharide-stimulated RAW 264.7 cells.
Exp Ther Med, 16:400-405, 2018.



37. Matejka M, Partyka L, Ulm C, Solar P, Sinzinger H : Nitric oxide synthesis is increased in periodontal disease.
J Periodontal Res, 33:517-518, 1998.


38. Lohinai Z, Benedek P, Fehér E, Györfi A, Rosivall L, Fazekas Á, Salzman AL, Szabó C : Protective effects of mercaptoethylguanidine, a selective inhibitor of inducible nitric oxide synthase, in ligature-induced periodontitis in the rat.
Br J Pharmacol, 123:353-360, 1998.




39. Lappin DF, Kjeldsen M, Sander L, Kinane DF : Inducible nitric oxide synthase expression in periodontitis.
J Periodontal Res, 35:369-373, 2000.



40. Graves D : Cytokines that promote periodontal tissue destruction.
J Periodontol, 79(8 Suppl):1585-1591, 2008.


41. Takemura A, Nakagawa I, Kawai S, Inaba H, Kato T, Hamada S, Amano A : Inhibitory effects of tumor necrosis factor-alpha on migration of human periodontal ligament cells.
J Periodontol, 77:883-890, 2006.


42. Graves DT, Oates T, Garlet GP : Review of osteoimmunology and the host response in endodontic and periodontal lesions. J Oral Microbiol. 2011 Jan 17;3. doi:
10.3402/jom.v3i0.5304

44. Murakani S, Hashikawa T, Sano T, Takedachi M, Nozaki T, Shimabukuro Y, Okada H : Adenosine regulates the IL-1β-induced cellular functions of human gingival fibroblasts.
Int Immunol, 13:1533-1540, 2001.


46. Bitto A, Oteri G, Pisano M, Pollito F, Irrera N, Minutoli L, Squadrito F, Altavilla D : Adenosine receptor stimulation by polynucleotides (PDRN) reduces inflammation in experimental periodontitis.
J Clin Periodontol, 40:26-32, 2013.



47. Altavilla D, Bitto A, Polito F, Marini H, Minutoli L, Stefano VD, Irrera N, Cattarini G, Squadrito F : Polydeoxyribonucleotide (PDRN): a safe approach to induce therapeutic angiogenesis in peripheral artery occlusive disease and in diabetic foot ulcers.
Cardiovas Hematol Agents Medi Chem, 7:313-321, 2009.

48. Bitto A, Polito F, Altavilla D, Minutoli L, Migliorato A, Squadrito F : Polydeoxyribonucleotide (PDRN) restores blood flow in an experimental model of peripheral artery occlusive disease.
J Vasc Surg, 48:1292-1300, 2008.


49. Galeano M, Bitto A, Altavilla D, Minutoli L, Polito F, Calò M, Cascio PL, d’Alcontres FS, Squadrito F : Polydeoxyribonucleotide stimulates angiogenesis and wound healing in the genetically diabetic mouse.
Wound Repair Regen, 16:208-217, 2008.


50. Polito F, Bitto A, Galeano M, Irrera N, Marini H, Calò M, Squadrito F, Altavilla D : Polydeoxyribonucleotide restores blood flow in an experimental model of ischemic skin flaps.
J Vasc Surg, 55:479-488, 2012.


52. Al-khafaji LK, Ali ML, Shaalan AH, Al-hijazi AY : Effect of VEGF on the Success of Dental Tissue Regeneration in Delayed Replantation of Avulsed Teeth. Syst Rev Pharm, 11:160-164, 2020.
53. Mullane EM, Dong Z, Sedgley CM, Hu JC, Botero TM, Holland GR, Nör JE : Effects of VEGF and FGF2 on the revascularization of severed human dental pulps.
J Dent Res, 87:1144-1148, 2008.
















 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



