Prevalence, Severity, and Correlation with Agenesis of Permanent Successors of Infraoccluded Primary Molars at Chonnam National University Hospital’s Department of Pediatric Dentistry
Article information
Trans Abstract
This study aimed to analyze the prevalence and severity of infraoccluded primary molars (IPM) and their correlation with the agenesis of permanent successors (APS). A total of 4,011 panoramic radiographs from children aged 4 to 11 years who had all 8 primary molars were examined. The prevalence of APS was analyzed based on the severity and tooth type of IPM. The prevalence of IPM was 13.0%, and there was no difference between genders. The majority of the children had two IPMs each. In all tooth types, mild infraocclusion was the most prevalent, whereas severe infraocclusion was the least frequent. Among the types of primary molars, the lower primary first molar (62.3%) was the most affected, followed by the lower primary second molar (27.7%), the upper primary second molar (5.8%), and the upper primary first molar (4.2%). Infraocclusion was 11.2 times more prevalent in the mandible than in the maxilla, with no significant difference between the left and right sides. The correlation between IPM and APS was also investigated. Among the subjects, 177 had one or more agenesis of premolars, of whom 54 (30.5%) had IPM. Additionally, among the 521 individuals with IPM, 54 individuals exhibited APS (10.4%). This study identified a noteworthy prevalence of infraocclusion, with notable variations among molar types. The LPFM was particularly affected. The majority of cases were classified as mild in severity. Furthermore, a compelling association between IPM and APS was established. Understanding this connection may enhance treatment strategies for infraoccluded teeth and tooth agenesis.
Introduction
Infraocclusion is a clinical condition where a tooth is situated below the occlusal plane when compared with adjacent teeth. This condition is common, particularly in deciduous teeth [1]. The diagnosis of infraocclusion involves clinical examination and radiological assessment. The former includes observations of differences in occlusal plane height, tooth immobility, and metallic sounds upon percussion, whereas the latter is often conducted through panoramic radiographs and plays a pivotal role in diagnosing infraocclusion [2-4].
Ankylosis is known to be the main cause of infraocclusion. On the other hand, tooth ankylosis is caused by local (trauma, infection, and inflammation) and genetic factors [5,6], although the specific related genes have not yet been clearly identified [7]. Delayed tooth eruption is associated with various developmental disorders, such as cleidocranial dysplasia, condylar hyperplasia, and amelogenesis imperfecta [8].
The occurrence frequency of infraocclusion in deciduous teeth has been reported to range from 2.8% to 38.5% [9]. These variations are largely attributed to study population age, diagnostic methodologies, and racial diversity [10]. A previous study has demonstrated that there is no gender difference in occurrence. Infraocclusion is more frequent in deciduous and mixed dentition than in permanent dentition, in the posterior than in the anterior teeth, and in the mandibular than in the maxillary arch [11]. However, controversy exists regarding the prevalence rates of the primary first and second molars.
Clinical symptoms associated with infraocclusion include vertical bone loss, adjacent tooth displacement, dental midline deviation, impaction of retained deciduous or permanent successor teeth, delayed eruption of ankylosed teeth or successors, excessive eruption of opposing teeth, and altered eruption paths for successor teeth [11]. In addition, infraocclusion severity can vary depending on the timing of ankylosis occurrence due to the vertical growth of adjacent alveolar bone [2,12]. Also, retained primary molars with the agenesis of permanent successors (APS) often undergo progressive infraocclusion, and their exfoliation is not easily predictable [13].
Previous studies have shown that infraocclusion cases are commonly mild [3,10], with most research focusing on the severity of infraocclusion in primary first and second molars [14]. Notably, the severity tends to be more prominent in the second primary molar compared to the first primary molar [9]. However, research that directly compares infraocclusion severity between the teeth of the upper and lower jaws as well as between the left and right sides is still lacking.
Furthermore, several studies have reported an association between APS and infraoccluded primary molars (IPM) [15-17]. One hypothesis suggests that infraocclusion disrupts or delays the eruption path of permanent successor teeth; this disruption could potentially lead to altered eruption paths or even complete developmental failure of the permanent successor teeth, particularly in cases of severe infraocclusion [18]. However, research on the relationship between IPM and the prevalence of APS based on the four types of ankylosed teeth (maxillary/mandibular first and second primary molars) is scarce, as is research on the impact of the infraocclusion degree on APS.
IPM treatment is influenced by various factors such as the timing of diagnosis, the patient’s age, the degree of infraocclusion, and the presence of permanent successors, making early diagnosis essential [7]. To address this problem, studies on the prevalence and characteristics of infraoccluded teeth have been conducted in various countries [3,14,15,19]; however, to the best of our knowledge, there is no research conducted specifically on pediatric patients in Korean or within the Asian population.
Therefore, this study aimed to use panoramic radiographs of pediatric patients who visited Chonnam National University Hospital to analyze the prevalence, distribution, and severity of infraocclusion in each type of primary molar. In addition, it aimed to evaluate the correlation between infraocclusion and APS.
Materials and Methods
This study was approved by the Institutional Review Board of Chonnam National University Hospital (IRB No: CNUDH-2023-011).
1. Study Subjects
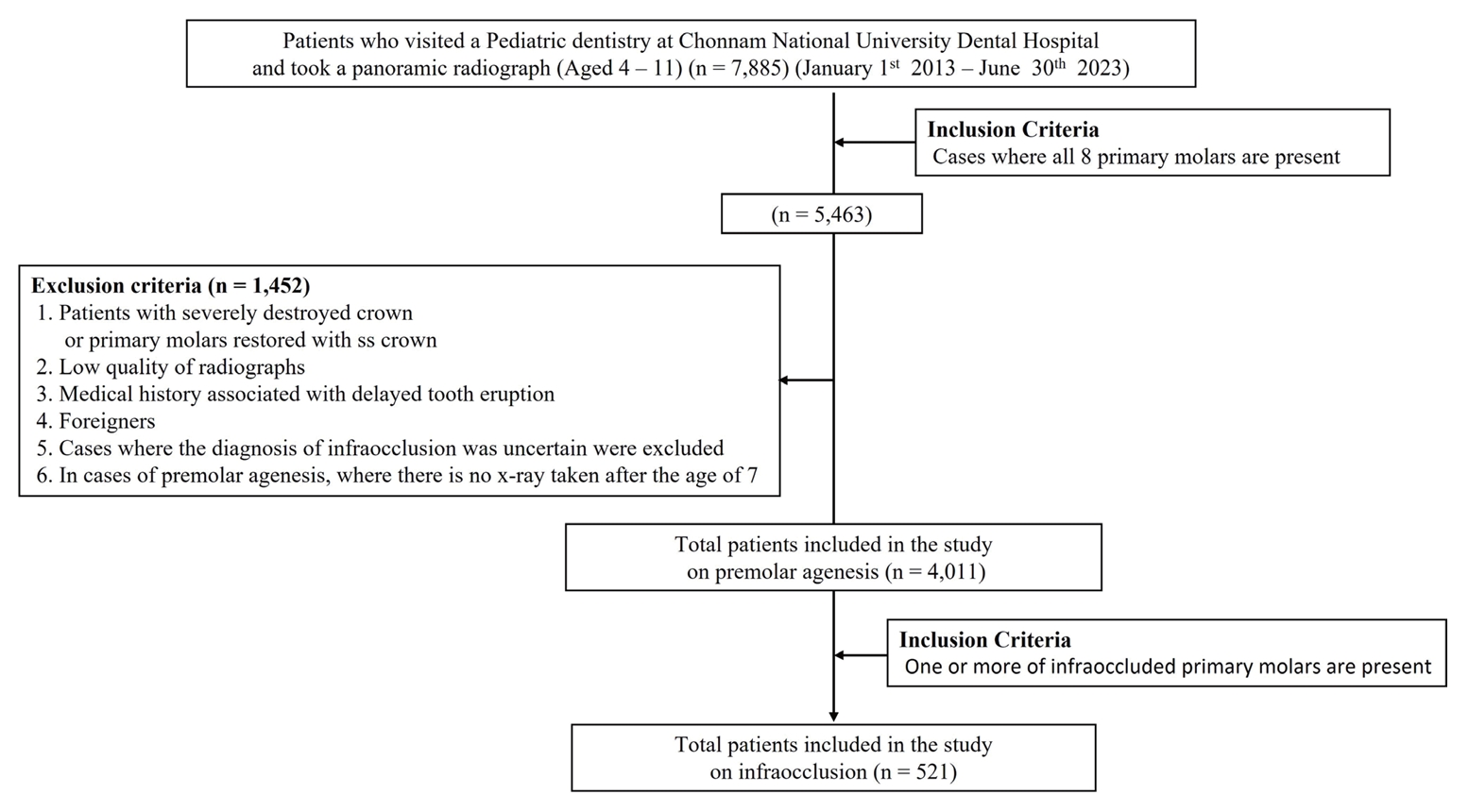
A total of 7,885 panoramic radiographs from children aged 4 to 11 years who visited the Pediatric Dentistry Department at Chonnam National University Hospital from January 1, 2013, to June 30, 2023, and had all eight primary molars were examined. The exclusion criteria were as follows.
1) Patients with severely destroyed crown or primary molars restored using stainless steel crowns
2) Poor-quality or distorted panoramic radiographs
3) Patients with developmental disorders highly correlated with delayed tooth eruption (cleidocranial dysplasia, condylar hyperplasia, amelogenesis imperfecta)
4) Non-Korean patients
5) Cases where the diagnosis of infraocclusion was uncertain were excluded
6) Individuals diagnosed with agenesis of primary molars at age 7 or younger, with no subsequent panoramic X-ray taken after the age of 7 during follow-up visits
A total of 4,011 subjects (2,496 boys and 1,515 girls) were included in the analysis after applying the exclusion criteria (Fig. 1).
2. Study Methods
This study examined 4,011 panoramic radiographs. For the infraocclusion cases, the tooth numbering, age, gender, and degree of infraocclusion were recorded. Additionally, the age of diagnosis for infraocclusion in each primary molar was categorized into pre- and postaverage exfoliation timings. The timing was based on the standards: 10.5 years for maxillary/mandibular first primary molars, 11.5 years for maxillary second primary molars, and 11 years for mandibular second primary molars [20]. The prevalence of infraocclusion was compared by gender, arch types, and arch sides. In the pan-oramic radiographs, the degree of infraocclusion was measured in millimeters as the vertical distance between the marginal ridge of IPM and the line connecting the mesial and distal marginal ridges of normal adjacent teeth. When measuring the degree of infraocclusion for the second primary molar, comparisons were made with either the first primary molar or the first permanent molar. For the first primary molar, the height difference with the second primary molar, not the primary canine, was measured. In cases where both teeth were infraoccluded simultaneously, the degree of infraocclusion for the second primary molar was measured first. Subsequently, the relative degree of infraocclusion with the first primary molar was measured and calculated (Fig. 2). Values below 1 mm were considered to indicate no infraocclusion, whereas 1 mm to less than 2 mm indicated mild; 2 mm to less than 3 mm, moderate; and 3 mm or more, severe infraocclusion of each tooth number. The Federation Dentaire Internationale system was used to document the tooth numbering: 54, 55, 64, 65, 74, 75, 84, and 85.

Measurement method of infraocclusion level (mm). If the first and second primary molars in the same quadrant are ankylosed, the second primary molar (①) is measured first, followed by the measurement of the first primary molar (②).
Based on tooth type, agenesis of premolars was classified into upper first premolar (UFP), upper second premolar (USP), lower first premolar (LFP), and lower second premolar (LSP). Tooth type, presence of IPM, and severity of infraocclusion, if present, were recorded. Agenesis of premolar was diagnosed based on the absence of calcification observed in panoramic radiographs taken after the age of 7 [21].
3. Statistical Analysis
All statistical analyses were conducted using SPSS version 25.0 (SPSS Inc., Chicago, USA). We examined the prevalence of IPM, comparing differences among genders and tooth types. We also evaluated variations in severity based on tooth types. Furthermore, the association between APS and infraocclusion and its correlation with the degree of infraocclusion severity and APS were assessed. All statistical analyses were conducted using chi-squared test.
Results
1. Prevalence of infraoccluded primary molars
Of the 4,011 subjects (1,515 girls and 2,496 boys), 521 (322 girls and 199 boys) had infraocclusion, resulting in an overall prevalence of 13.0%, with no gender difference (Table 1, p = 0.83). The mean ages at which infraocclusions were observed were 6.4 and 7.3 years for the girls and boys, respectively. Fig. 3 depicts the distribution of IPM by age, with the highest prevalence observed at ages 6 and 7.

Distribution of infraoccluded primary molars by age. IPM: Infraoccluded Primary Molars; LPSM: Lower Primary Second Molar; LPFM: Lower Primary First Molar; UPSM: Upper Primary Second Molar; UPFM: Upper Primary First Molar.
Among the subjects, infraocclusion was more prevalent in those with 2 IPMs, followed by those with one and then 4 IPMs in the descending order (Fig. 4).
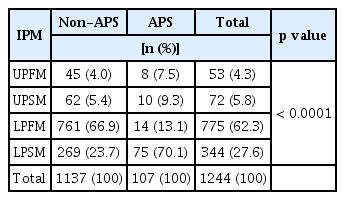
IPM was observed 11.2 times more frequently in the mandible than in the maxilla (Table 2, p < 0.0001), with no significant difference between the left and right sides (Table 2, p = 0.72). Among the tooth types, the lower primary first molar (LPFM) had the highest prevalence of infraocclusion (62.3%), followed by the lower primary second molar (LPSM, 27.7%), the upper primary second molar (UPSM, 5.8%), and then the upper primary first molar (UPFM, 4.2%) (Table 3, p < 0.0001). Cases diag-nosed before the average exfoliation timing were significantly more common in all tooth types. The distribution of infraocclusion on the left and right sides was similar for all tooth types (Table 3).
2. Distribution of the degree of infraocclusion
Table 4 presents the distribution of the degree of infraocclusion. In all tooth types, mild cases were the most prevalent (n = 1,034, 83.1%), followed by moderate (n = 172, 13.8%) and then severe (n = 438, 3.1%). In all tooth types, a similar prevalence was observed between both sides. In the UPSM and LPSM, the proportions of moderate and severe severity were higher compared to the UPFM and LPFM types, respectively (Table 4, p < 0.0001).
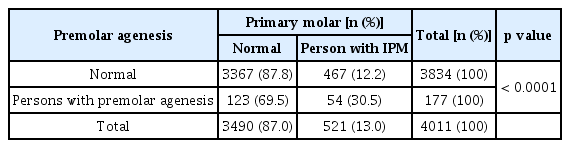
3. Correlation between infraocclusion and agenesis of permanent successors
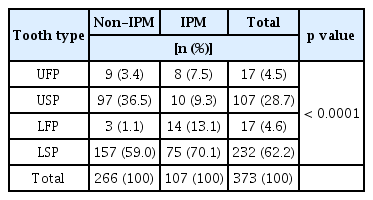
Of the 4,011 subjects, 177 (4.4%) had at least one missing premolar, for a total of 373 missing teeth. Among the subjects with missing premolars, 54 out of 177 (30.5%) had primary molar infraocclusion. Conversely, among the 521 individuals with IPM, 54 individuals exhibited permanent tooth loss (10.4%) (Table 5, p < 0.0001). Table 6 presents the distribution and prevalence of IPM based on the presence of premolar agenesis. Among the 1,244 cases of IPM, 107 (8.6%) were accompanied by APS. The prevalence of IPM in the non-APS group was similar to that of the total IPM. However, the frequency of IPM associated with APS showed the sequence of LPSM, LPFM, UPSM, and UPFM (Table 6, p < 0.0001). In contrast, Table 7 shows the distribution and prevalence of premolar agenesis in the non-IPM group and the IPM group. Among the 373 cases of premolar agenesis, 107 (28.7%) were accompanied by IPM. The prevalence of premolar agenesis in the non-IPM group followed the order of LSP, USP, UFP, and LFP, while in the IPM group, the prevalence of APS exhibited the sequence of LSP, LFP, USP, and UFP (Table 7, p < 0.0001).
Furthermore, in all tooth types, APS was most prevalent when the degree of primary molar infraocclusion was mild, although no statistically significant difference was observed (Table 8, p = 0.80).
Discussion
The reported occurrence frequency of infraocclusion in teeth widely varies from 2.8% to 38.5% [9]. These differences seem to be significantly influenced by race, age, and diagnostic method [5,10]. In a study comparing the prevalence of submerged molars among different 7 ethnic groups (Kurds, East Europeans, Druse, Circassians, North Africans, Cochins, and Yemenites), Kurds exhibited the highest prevalence at 35.3%, while Yemenites showed the lowest prevalence at 14.2% [10]. There were no previous studies targeting Koreans or Asians; however, the current paper indicates an incidence rate of 13%. While this is higher than the incidence rates of Turkish children aged 7 - 11 (3.3%), Italian children aged 5 - 15 (6.6%), and Swedish children aged 3 - 12 (8.9%), it is lower than the incidence rate of Israeli children aged 3 - 13 (24.8%) [5,14,22,23].
Notably, infraocclusion prevalence is age-dependent; thus, the age range of the subjects is likely to have a significant impact [5]. Ankylosis of the first primary molars starts at age 3, whereas that of the second primary molars starts at around age 5, it was least common in the 12-year-old. Additionally, the highest prevalence of ankylosis of the primary molars is observed at ages 7 - 9 [5,20,24-28]. The present study focused on patients aged 4 to 11 years. There were cases of delayed eruptions even within the 3-year-old range. To exclude cases where infraocclusion might be misdiagnosed as delayed eruption, the age range of 3 years old was excluded. Furthermore, the age was limited up to 11 years since the study focused on patients including all 8 permanent molars.
Previous studies reported that the number of ankylosed teeth per person accompanying infraocclusion ranged from 1.7 to 2.1 per child [27,29,30]. In the present study, a slightly higher ankylosis prevalence of 2.4 per child was observed.
In accordance with the present study’s findings, most studies have reported no significant difference in the occurrence of infraocclusion based on gender [3,14,24]. Infraocclusion was found to be significantly more prevalent in the mandible than in the maxilla, and no significant differences were observed in prevalence between the left and right sides, consistent with the previous findings [14,24]. Furthermore, the LPFM had the highest prevalence of infraocclusion, followed by the LPSM, UPSM, and then UPFM. However, the prevalence of ankylosis of the first and second primary molars remains controversial [9]. Some studies have reported high prevalence in the LPSM [9,14,28], whereas others have reported high prevalence in the LPFM [30,31].
Exfoliation is delayed in most cases of IPM. For individuals with permanent successors, this delay is typically around 6 months from the expected time. However, in cases of aplasia, this delay has been observed to be considerably extended [13]. In this study, 3.8% of the cases were attributed to delayed exfoliation. However, due to the limited age range in this study, setting a broader age range for future research on this aspect can yield more reliable results.
Similar to other studies, infraocclusion was defined as the condition where a tooth is located 1 mm or more below the occlusal plane [31,32]. Infraocclusion was quantitatively measured on panoramic images, as done in a previous study [29,33]. Consistent with other study findings, the prevalence of mild infraocclusion (83%) was the highest in all tooth types, whereas severe infraocclusion (3%) was notably low [3,4,10]. Studies comparing the first and second primary molars demonstrated that moderate and severe infraocclusion tended to be more prevalent in the latter, consistent with the results of this study [9,15,34].
Infraocclusion is associated with various dental anomalies; in a previous study, more than half of the children with infraoccluded teeth had dental anomalies, particularly dental agenesis [14]. In this study, only 54 out of 521 children (10.4%) with ankylosis had APS, which is slightly lower than the 12.5% reported in the previous study [9]. Futhermore, the prevalence of infraocclusion in children with hypodontia was 8.6%, resembling the value from a previous domestic study, which was 7.7% [35]. Furthermore, in addition to dental agenesis, dental anomalies such as peg lateralis, second premolar agenesis, palatally displaced maxillary canines, enamel hypoplasia, and dis-tal angulation of the lower second premolars have been reported. There is a reciprocal association between each dental anomaly and infraocclusion. These correlations substantiate that infraocclusion of deciduous molars is a distinct element within dental anomaly patterns, characterized by groups of interconnected dental abnormalities likely stemming from shared genetic origins [16]. In this study, we focused on the correlation between the agenesis of permanent successors and infraocclusion, and currently, there is a lack of studies analyzing the APS and IPM by tooth type. In this study, the distribution of APS and IPM was compared by categorizing them into normal groups and groups with IPM or APS for each of the 4 tooth types, indicating strong correlations were observed between them based on tooth types. Undoubtedly, including research on various dental anomalies beyond just APS, future studies will shed light on the genetic correlation with dental anomalies. The prevalence of infraocclusion was highest in LPFM, but it exhibited the highest premolar agenesis when it occurred in LPSM. Additionally, in the non-IPMs group, the pattern of APS prevalence was similar to those in previous studies, showing LSP as the most prevalent, followed by USP [21]. However, in the IPM group, different results were obtained, with LSP having the highest prevalence, followed by LFP. This indicates a connection with genetic origin rather than just local factors in the occurrence of infraocclusion [5].
Further research with a larger sample size, including a broader range of congenital tooth loss cases, could provide more accurate information if conducted, thereby shedding more light on this aspect. While the precise cause-and-effect relationship between congenital tooth loss and infraocclusion of primary molars is not yet fully elucidated, one hypothesis suggests that infraocclusion of primary molars disrupts or delays the eruption path of permanent successor teeth. Similarly, primary molars without permanent successor teeth tend to exhibit more severe infraocclusion [14]. However, in the present study, loss of permanent successor teeth was more frequent in cases of mild infraocclusion, and the correlation between infraocclusion severity and loss of permanent successor teeth was not confirmed.
The association between primary molar ankylosis and loss of permanent successor teeth highlighted in this study calls for further clinical investigations. The results of this study may provide valuable insights for the design and implementation of future clinical research. The findings also emphasize the importance of early diagnosis of infraocclusion and the provision of intervention.
This study had several limitations. First, the subjects were from a single center, a tertiary medical institution; hence, there could be differences from the studies involving patients from general dental clinics or the general population. Therefore, further research involving patients from multiple institutions nationwide and the general population could provide more accurate information on the prevalence of IPM and APS as well as the severity of infraocclusion in Korean pediatric patients. Second, panoramic radiographs were used to diagnose congenital tooth loss starting at age 7 [18,21]. It has been reported that crown formation of the mandibular second premolars has been observed even in children over the age of 12[ 35]. As the possibility of tooth developmental delay cannot be completely ruled out, inherent diagnostic limitations exist for tooth loss. Future studies should expand the age criteria for diagnosing congenital tooth loss to achieve more accurate research results.
Conclusion
This study analyzed the prevalence and severity of IPM as well as its correlation with congenital permanent tooth loss in children who visited Chonnam National University Hospital. The prevalence of infraoccluded teeth was found to be 13.0%; with the highest prevalence observed at the age of 7, the tooth-specific prevalence of infraoccluded teeth ranked in the order of LPFM, LPSM, UPSM, and UPFM, with a similar prevalence observed between genders and left and right sides. As regards severity, mild infraocclusion was the most prevalent in all tooth types, whereas severe infraocclusion was the least frequent. In addition, moderate and severe infraocclusion tended to be more prevalent in the second primary molar than in the first primary molar. The occurrence and frequency of agenesis of premolars varied depending on the presence of IPM. 10.4% of individuals with IPM also had APS, while 30.5% of individuals with APS exhibited IPM.
These findings can improve the clinical understanding of the relationship between infraocclusion and congenital tooth loss, potentially providing insights into the treatment and management of infraoccluded teeth.
Notes
Conflict of Interest
The authors have no potential conflicts of interest to disclose.