심미수복용 기성 지르코니아 크라운의 색조 평가
Colorimetric Analysis of Preformed Zirconia Anterior Crowns for Esthetic Restoration
Article information
Abstract
이 연구의 목적은 지르코니아 크라운의 종류 및 두께와 시멘트 종류에 따른 색조를 평가하여 상악 유중절치와 가장 유사한 조합을 확인하는 것이었다.
시중에 유통되는 3가지 색조의 기성 지르코니아 크라운과 6종류의 지르코니아 블럭을 이용해 제작한 크라운이 연구에 사용되었고, A2 shade 또는 translucent shade의 레진 시멘트로 크라운 내면을 충전하였다. 분광 광도계를 이용하여 각 시편의 L*, a*, b* 값을 평가하여, 자연치와 지르코니아 크라운의 색 차이(ΔEn)를 평가하였다.
시편의 색조는 translucent-shade 레진시멘트를 사용했을 때 보다 A2-shade 레진시멘트를 사용하였을 때 더욱 자연치와 유사하였고, smile series 2 (SmS2) 지르코니아 블록으로 0.5 mm 두께의 크라운을 제작하여 A2-shade 레진시멘트로 채웠을 때 가장 자연치와 색 차이가 가장 작았다.
한국 어린이들의 상악 유전치부를 지르코니아 크라운으로 수복할 때, translucent-shade의 레진시멘트 보다는 A2-shade의 레진시멘트를 사용하는 것이 권장되고, 기성 지르코니아 크라운은 색조면에서 심미성이 충분하지 못하기 때문에 기성 지르코니아 크라운의 색조 개선이나 새로운 종류의 지르코니아 크라운의 개발이 필요하다.
Trans Abstract
The purpose of this study was to identify which combination of zirconia crowns and cements is most similar in color to the maxillary primary incisors by varying the color of zirconia crowns, crown thickness, and shade of cements. Prefabricated zirconia crowns in 3 shades and crowns fabricated using 6 types of zirconia blocks were used in this study. These were filled with A2-shade or translucent-shade resin cement and the L*, a*, and b* values were calculated using a spectrophotometer. The color differences between the natural teeth and the zirconia crowns were assessed. The shade of the final restoration was more similar to that of the natural teeth using A2‑shade than translucent-shade resin cement. Application of A2-shade cement to a 0.5-mm-thick crown fabricated from a smile series 2 zirconia block resulted in the color most similar to that of the natural teeth. A2-shade resin cement is recommended for zirconia crown restoration in anterior primary teeth compared to TR-shade resin cement for more esthetic restoration. Since restorations with Nusmile zirconia crowns were not esthetically favorable in terms of shade, improvement of the shade characteristics of the product or development of a new kind of zirconia crown is required.
Ⅰ. Introduction
Early childhood caries on the maxillary anterior teeth can be treated with full veneer crowns or direct resin restorations. The use of preformed zirconia crowns, which have proven physical durability and enhanced esthetics, especially for the primary incisors, has increased recently. However, few color variations are available, and it is difficult to ensure that the restoration blends in with the natural teeth.
Self-colored zirconia blocks with Fe2O3 content of 0.029 to 0.143 wt%, which do not need additional staining, are now available. Preformed crowns with the desired shape, color, and thickness can be fabricated using these zirconia blocks[1].
Because sintered zirconia is translucent, the luting cement affects the final shade of the restored tooth. Differences in translucency cause differences in the color of a restoration. The magnitude of light transmittance depends on the type and thickness of the zirconia block, as well as the shade of the luting cement[2,3]. Therefore, the final color of a tooth restored with a zirconia crown depends on the color of the zirconia, the thickness of the restoration, and the shade of the luting cement.
Shade matching for esthetic restoration with visual method is widely used method among dentists, but it is not objective method and the result of it is acceptable only when the trained expert performed. The spectrophotometer is an instrument for shade matching. It is useful for shade matching of the surface color, and it functions by measuring the spectral reflectance or transmittance curve of a specimen[4,5]. Developments in color-measuring equipment and the increased interest in esthetic restorations have enhanced the importance of reproducing the color of the teeth. However, currently available products are incapable of producing esthetic restorations that meet the requirements of dentists or patients[6,7]. Therefore, it is necessary to develop a zirconia crown for the primary teeth with a color very similar to that of the natural teeth.
The color of the primary teeth, restorative materials, and resin crowns has been evaluated in previous studies[8-10]. Regarding the preformed zirconia crowns, Lee[11] evaluated the shade of commercially available preformed zirconia crowns depending on the type of cements, but there was no esthetic result that is below the color threshold. Thus, this study aimed to evaluate which combination of zirconia crowns and cements is most similar in color to the maxillary primary incisors by varying the color and type of zirconia crowns, crown thickness, and shade of cements.
Ⅱ. Materials and Methods
1. Shade measurement of primary teeth
Shadepilot (DeguDent GmbH, Hanau, Germany, Fig. 1), a spectrophotometer with high levels of accuracy and reproducibility in vivo and in vitro, was used in this study[12]. The shade of intact maxillary right central incisors of children was measured by Shadepilot at three randomly selected child daycare centers. The informed consents were obtained from the children and their parents, and 105 children aged between 4 to 6 years old was enrolled in this study. The measurements were performed from 10:00 to 14:00 with the children lying on a mobile dental chair in front of a window with sufficient natural light.
The measurement procedure was as follows. All children performed tooth-brushing under the supervision of the tester before the measurement. After brushing, the child was laid on the chair and the labial surface of the teeth was wiped with sterile gauze. Visual inspection was performed to exclude teeth with labial or proximal caries, teeth discolored due to trauma, restored teeth, and extracted teeth. To avoid excessive drying, the child drank a cup of water. Then the child’s lips were retracted by the tester using one hand, and Shadepilot was placed on the labial gingiva of the maxillary right primary central incisor. An image of the crown was obtained in accordance with the angle displayed on the screen. The colorimeter was calibrated prior to each measurement. The results of measurements of intact maxillary right primary central incisors were expressed as Commission international de l’éclairage (CIE) Ln*, an*, and bn* values.
2. Materials
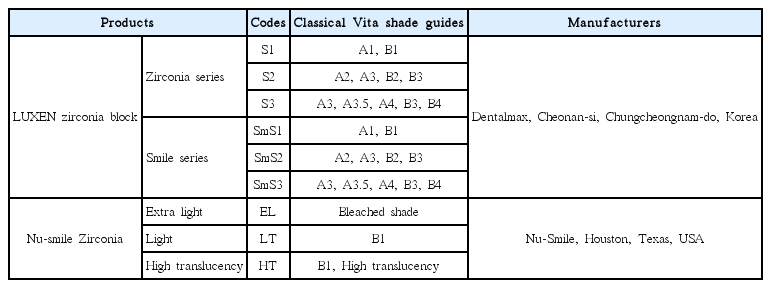
3 shades of LUXEN (Dentalmax, Cheonan-si, Chungcheongnam-do, Korea) zirconia series (S1, S2, and S3) and 3 shades of LUXEN smile series (SmS1, SmS2, and SmS3) were used to fabricate specimens in this study. 3 shades of Nu-smile zirconia crowns (Nu-Smile, Houston, Texas, USA), extra‑light shade (EL), light shade (LT), and high-translucency shade (HT) for the maxillary right central incisor were used in this study (Table 1).
3. Specimen preparation
The zirconia specimens were machined by computer-aided design (CAD)/computer-aided manufacturing (CAM) using eight selected zirconia blocks. To fabricate a crown, Nusmile zirconia crown for the maxillary right central incisor was scanned using a 3Shape D900 scanner (3Shape, Copenhagen, Denmark, Fig. 2), and a zirconia crown of the same size and shape was designed using a computer-aided design software (3Shape Dental System, 3Shape, Copenhagen, Denmark). To determine the thickness of the zirconia crown to be fabricated, the thickness of the labial surface of the Nu-smile zirconia crown was measured. The thickness on the middle third of the labial surface of the Nu-smile crown was measured using Iwanson Wax Calipers (Hu-Friedy, Chicago, IL, USA). The average thickness was 0.6 mm with little deviation. Thus zirconia crowns were fabricated in 2 thicknesses (0.5 and 0.6 mm). The surfaces were polished with #1200 SiC abrasive paper to enhance surface uniformity and adjust surface thickness. Sintering of the specimens was performed with Trione-F (DIO implant, Busan, Korea). The temperature was raised to 1450℃ at a rate of 8.3℃/min and maintained for 2 hours, followed by oven-cooling to room temperature. 10 specimens were prepared for each thickness and divided into 2 subgroups for 2 types of cement. Thus, each subgroup comprised 5 specimens. The interiors of the crowns produced for this study and the Nu-smile zirconia crowns were filled with 2 shades of Rely-X U200 Automix (3M/ESPE, Neuss, Germany): translucent (TR) and A2 shade. In accordance with the manufacturer’s instructions, the crown was filled with cement using an automatic mixing syringe from the incisal tip to a slight overflow, taking care to avoid producing air bubbles. Light curing was carried out using VALO (Ultradent Products, South Jordan, UT, USA) light curing unit at an intensity of 1000 ㎽/㎠ for 20 seconds on each labial and lingual surface, and excess cement was removed (Fig. 3A, 3B)
4. Shade measurements of zirconia crowns
The shades of the zirconia crowns were measured by the spectrophotometer after applying resin cement. All measurements were performed by one researcher from 10:00 to 14:00. The fabricated crown was fixed with transparent wax to the position of the maxillary right incisor in dentiform. The dentiform was installed on the head of a mannequin by the window of the dental practice room to ensure sufficient natural light. The Spectrophotometer was placed on the labial surface of the crown to be measured, and an image of the crown was obtained in accordance with the angle displayed on the screen. Calibration was performed prior to each measurement (Fig. 3C).
The CIE La*, aa*, and ba* values of the test materials were measured in triplicate and the means were calculated. The color difference (ΔEn) between the natural teeth (CIE Ln*, an*, and bn*) and test materials (CIE La*, aa*, and ba*) was calculated using the following equation:
5. Color threshold
The color threshold, the criterion for distinguishing 2 shades, was set to ΔE = 3.3. A color difference (ΔEn) between the natural teeth and zirconia crowns of less than 3.3 was regarded as an esthetic restoration[13].
6. Statistical analysis
The Mann-Whitney U test was performed to compare color differences according to the shade of cement in preformed crowns, and the color differences between the Nu-smile zirconia crowns and fabricated zirconia crowns for this study. Statistical analysis was performed using SPSS (version 23.0; IBM Corp., Armonk, NY, USA).
Ⅲ. Results
1. Shades of maxillary right primary central incisors
The mean CIE values of the maxillary right primary central incisors of the 105 subjects were Ln* = 75.00, an* = 3.07, and bn* = 11.51 (Table 2).
2. Color difference of Nu-smile zirconia crowns according to shade of luting cement
The ΔEn value was higher using the TR-shade cement (LT = 7.61, HT = 7.56, EL = 11.00) than using the A2-shade cement (LT = 6.97, HT = 6.09, EL = 8.92). There were statistically significant differences in ΔEn value between TR cement and A2 cement in the HT group (p= 0.01) and EL group (p= 0.01, Table 3).
3. Shade measurement of zirconia crowns
Application of A2 shade cement to a crown of 0.5 mm thickness made from SmS2 resulted in the color most similar to that of the natural teeth (ΔEn = 1.62) among all specimens. Also, it was significantly different from HT with A2 cement (ΔEn = 6.09), which was the most similar in color to natural teeth among the Nu-smile zirconia crowns (Table 4, 5).
Ⅳ. Discussion
The destruction of early affected maxillary primary anterior teeth is more severe than that of other affected teeth. Prevention and treatment of early childhood caries are important because of the risk of severe esthetic, mastication, pronunciation, and psychological development issues[14,15]. In Korea, the rate of dental caries is highest in the maxillary right primary central incisors of 2-year-old children[16]. Failure to treat caries of the primary anterior teeth may lead to early loss of teeth, and consequent psychological issues. Restoring primary dentition enhances esthetics and facilitates the emotional and social development of the child, and provides satisfaction to their caregivers[17].
Strip crowns are commonly used to restore maxillary primary incisors due to their pleasing esthetics, multiple shades, and applicability to crowded dentition[18]. However, bleeding and salivation must be controlled during the placement of strip crowns as these adversely affect the color of the restoration and the adhesive bond strength of the composite resin[19]. Several products have been introduced to overcome the disadvantages of strip crowns. Preformed metal crowns are typically used for cases with several caries-affected teeth. They are easy to apply, have good operability, good retention, and are relatively unaffected by moisture. However, these are not favored by patients and caregivers due to esthetic issues. The esthetics can be enhanced by reducing the labial surface of the crown and restoring it with resin composites. However, the metal margin remains visible and the restoration procedure takes longer[20]. Polycarbonate crowns are fabricated from thermoformed acrylic resin and can be used for the primary anterior teeth. Although polycarbonate crowns are more esthetically favorable than metal crowns, they are relatively weak. Furthermore, the long-term retention of polycarbonate crowns is unclear, which limits their use[21].
The first esthetically favorable zirconia crown for the primary anterior teeth was the EZ Pedo (Loomis, California, USA). Preformed zirconia crowns are available in various sizes, and have been used successfully in dentistry for many years[22,23]. Despite their high cost and technical difficulty, use of zirconia crowns is increasing because of the high fracture strength, esthetics, and biocompatibility. However, no study has evaluated the long-term success rates of zirconia crowns in children. 0% of zirconia crowns reportedly failed over a 6-month period, compared to 22% of strip crowns[24-26]. In vivo and in vitro studies of zirconia crowns have been performed, and their use in dentistry is likely to become more frequent[19].
Nu-smile zirconia crown have 3 shades light shade, extra light shade, and high translucency shade which was recently made available to accommodate the needs of domestic consumers. Although the manufacturer claims that these are suitable for esthetic restorations, fulfilling the esthetic requirements of dentists, patients, and caregivers is difficult[1,6]. Therefore, a zirconia crown with a color similar to that of the natural teeth is required. The thickness of the restoration and the color of the cement must be taken into consideration to produce a restoration with a color similar to that of the natural teeth[27-29]. In this study, the ΔEn values of crowns using A2-shade cement showed lower than those using TR-shade cement in all types of crowns. Among Nu-smile zirconia crowns, the differences in ΔEn values according to the cement shade were statistically significant for HT shade and EL shade, but not LT shade. LT showed lower ΔEn value than EL, which was the same result with previous study[11], but higher ΔEn value than HT. Thus, a combination of an HT shade crown and A2 shade cement can result in the most natural color tone when using Nu-smile zirconia crowns. However, the ΔEn value of it was 6.09, which was still above the color threshold, meaning that the difference in color between the restored tooth and the natural teeth would be easily recognizable[30].
The L*, a*, b* values of specimens used in this study were slightly different from the previous study when comparing the same materials. In this study, the mean L*, a*, b* value of LT with A2-shade cement were 80.43, -0.11, 14.44 respectively, and those of EL with A2-shade cement were 82.70, 0.38, 7.93 respectively. However, in previous study, the mean L*, a*, b* value of LT with A2-shade cement were 82.59, -0.62, 12.64 respectively and those of EL with A2-shade cement were 85.85, -0.62, 4.85 respectively[11]. The specimens of this study showed lower L* value, higher a* value and b* value. Lower L* value means the lower brightness, higher a* value means more reddish rather than greenish, and higher b* value means more yellowish rather than bluish. This difference seems to be due to the different measuring environment. Even if the same materials were used, spectrophotometric result may vary depending on the background color[31]. Unlike previous study, this study is more significant in that it attempted to simulate the condition of the shade measurement of natural teeth.
The 0.5-mm-thick crown fabricated from the SmS2 block cemented with A2-shade cement had a color most similar to that of the natural teeth, and was difficult to distinguish from the natural teeth using the naked eye. In addition, it was significantly different from HT with A2-shade cement, which was the most similar in color to natural teeth among Nu-smile zirconia crowns. The ΔEn values of the 0.5-mm-thick crown fabricated from the SmS3 block cemented with A2-shade cement and the 0.6-mm-thick crown fabricated from the SmS2 block cemented with A2-shade cement were also below the color threshold. The zirconia crown fabricated with SmS2 block had a color similar to that of the natural teeth, irrespective of thickness; therefore, the SmS2 zirconia block is optimal for fabricating crowns for the primary anterior teeth.
In this study, shade measurement of the specimens attempted to simulate the intraoral conditions. However, there were several limitations. First, the limitation that a dentiform cannot reproduce the wet intraoral environment. It is well known that difference in humidity can affect shade matching. Second, the limitation that crowns were filled with resin cement without abutment teeth. As the color of the abutment also affects the shade of final restoration, this study has limitation in that it could not assess the effect of abutment teeth. However, utilizing the resin artificial teeth as the abutment teeth have limitation in that the color and characteristic is different from natural teeth, and it is difficult to obtain uniform natural teeth sample having the same shade and shape for abutment teeth. Third, zirconia crowns fabricated in this study had a consistent labial thickness of 0.5 mm or 0.6 mm, while the labial thickness of Nu-smile zirconia crown varies with region of the crown. Since it was impossible to scan the inner surface of the Nu-smile zirconia crowns, the limitation was that the shape of fabricated crowns did not completely coincide with the Nu-smile crowns. Finally, there was a limit to the variety of zirconia blocks used in this study. Considering these limitations, further study using other zirconia block products and natural teeth abutment is necessary.
Within the results of this study, it was found that the commercially available preformed zirconia crowns differed in shade from the natural primary teeth, and the crowns fabricated from other zirconia blocks resulted in more esthetic shade. Therefore, improvement of shade of preformed zirconia crown or development of new kinds of zirconia crown will be needed for esthetic restoration of primary teeth.
Ⅴ. Conclusion
This study aimed to identify the composition of zirconia crown restorations that resulted in a color most similar to that of the maxillary primary incisors. Based on the results of this study, A2-shade resin cement is recommended for zirconia crown restoration in anterior primary teeth compared to TRshade resin cement for more esthetic restoration. However, since restorations with Nu-smile zirconia crowns which are widely used on primary anterior teeth were not esthetically favorable in terms of shade, improvement of the shade characteristics of the product or development of a new kind of zirconia crown is required.