선천성 무통 무한증 환자의 치과적 관리 증례보고
Dental Management in a Patient with Congenital Insensitivity to Pain with Anhidrosis : A Case Report
Article information
Abstract
선천성 무통무한증(Congenital insensitivity to pain with anhidrosis, CIPA)은 NTRK1 유전자의 돌연변이에 의해 발생하는 드문 유전질환으로 통증에 대한 무감각 및 땀을 흘리지 못하는 것이 특징이다. 지적장애를 동반하는 경우가 많으며, 구강내 임상검사에서는 자해로 인한 병소를 제외하고 특징적인 병소가 발견되지 않으므로 초기 감별진단이 중요하다. 소아치과의사는 이 질환과 동반되는 조절되지 않는 체온, 지각 과민, 통증 반사의 부재와 같은 다양한 임상증상 등을 인지하고 있어야 하며 이를 치과 치료에서 고려해야만 한다. 이 연구는 본원에 첫 내원 이후 6년여간 경과 관찰 중인 선천성 무통무한증 환아의 치험례를 통하여 이 질환의 감별진단 및 치과 치료에서의 주의사항 등을 알아보고자 하였다.
Trans Abstract
Congenital insensitivity to pain with anhidrosis (CIPA) is a rare, autosomal recessive disorder; affected patients are characterized by inability to feel pain and to sweat over the entire body, as well as by mental retardation. Because, in the oral examination, no specific findings on soft or hard tissue may be found except possible lesions due to selfmutilation, early recognition and diagnosis are essential for these patients. Pediatric dentists must be aware of the clinical manifestations and treatment considerations related to uncontrolled body temperature, tactile hyperesthesia and lack of pain reflex. In this case report, dental management of CIPA was suggested by presenting a 6-year follow-up of young patient.
Ⅰ. Introduction
Congenital insensitivity to pain with anhidrosis (CIPA; MIM 256800) is a rare genetic disorder characterized by absence of pain sensation, inability to sweat and mental retardation as well as by normal tactile sensation, lacrimation, and salivation[1,2].
Although the worldwide CIPA prevalence is still unknown, a prevalence of 1/600,000 - 950,000 had been reported in Japan[3], and the specific ethnic background is reported to be consanguineous Israeli-Bedouin[4]. Affected patients have lossof-function mutations in the NTRK1 that encode TrkA (tropomyosin-related kinase A), which is a receptor for nerve growth factor (NGF)[5]. Because NGF functions as an inflammatory mediator associated with pain and a neurotrophic factor for establishing neural networks of interception and emotional response, reciprocal communications between the central and peripheral neural systems are impaired in CIPA patients[6].
The disease itself is not fatal; however, CIPA is a clinically serious illness. Recurrent, unexplained hyperthermia in early ages, accidental injuries with fractures, osteomyelitis, burns without autonomic response to painful stimuli threaten these patients. While general appearances of patients are normal, most of intra and extra oral findings are related with pain insensitivity. Oral findings of CIPA usually accompany selfmutilating lesions of soft and hard tissues. Tongue and lower lip biting are common while upper lip and buccal mucosa are less affected. Tooth luxation is also found and missing can be followed due to self-mutilation, and surgical extraction of teeth may be considered to prevent future oral injuries[7]. In severe cases of CIPA, recurrent bone fractures and systemic infections were reported, resulting from self-mutilation and anhidrosis that are often concurrent with unexplained, uncontrolled hyperpyrexia[3].
Kouvelas and Terzoglou[8] suggested that general considerations for CIPA patients include use of a mouth guard and education about self-mutilation for cooperative patients or dentures for uncooperative patients. In addition, routine dental procedures including pulp treatment may be performed without local anesthesia due to lack of pain; however, local anesthesia may be preferred as a vasoconstrictor during extractions.
In this case report, dental management of CIPA patients was suggested based on lessons learned in the case of a 7-yearold girl.
Ⅱ. Case report
A 7-month-old girl was referred by pediatrician to the dental hospital for oral bleeding. Except for a 0.5 cm laceration on the dorsal surface of the tongue, no other specific pathologic findings were found on intraoral examination, and topical ointment was applied with a chlorhexidine dressing on the same day. Despite regular dressings, healing of the tongue laceration was inhibited due to recurrent biting. Recurrent lacerations and ulcerations were usually found on the tongue during routine follow-ups from the age of 1 year. Frequent self-mutilating behaviors of fingers and tongue were described by her mother. Delayed development with mental retardation was suspected and the behaviors were not effectively prevented by patient education. Due to persisted tongue biting, tongue tip missing was prominent around the age 3 years (Fig. 1).

Intraoral examination of the CIPA female at the age of 5 years. Tongue tip missing and ulceration are found which are typical types of intraoral self-mutilation of CIPA.
Based on the delayed development, the patient visited pediatrician. In a language test around the age of 2 years, severely delayed language development below 1% of the Sequenced Language Scale for Infants (SELSI) and expressive language was found. The degree of intellectual disability was also implied depending on a low score of intelligence test (K-ABC).
While in the test, if the situation did not go well with her intention, the patient bite her fingers and pounded her head on the floor. Her parents recalled a lack of sweating over the past summer, recurrent fever, and pain insensitivity after burn from hot water bottle. Based on above symptoms including self-mutilation, the patient was examined for genetic analysis by pediatrician and was finally diagnosed with CIPA at the age of 3 years.
During follow-up treatment, oral hygiene was poor and caries were found from an early age, and due to deep caries and crown fractures on the primary maxillary anterior teeth, nonvital pulp treatment was started at the age of 14 months (Fig. 2A). Despite a preventive approach for dental caries, including fluoride application and professional tooth cleaning, right primary anterior tooth was extracted for severe mobility with periapical abscess at 4 years of age (Fig. 2B) and all posterior teeth were restored with composite resins and stainless-steel crowns with or without pulp treatment up to 5 years of age. During a dental treatment of caries, local anesthesia was usually applicated, while posture and vital signs as well as body temperatures were periodically monitored by assistance in the event of a relatively long-lasting treatment.

Periapical radiographs of primary maxillary anterior teeth. (A, B) The teeth were treated for periapical abscess at the age of 1 year and 4 years, respectively.
Regular dental visits for check-up were occasionally skipped or delayed because of unexpected repeated admissions due to unnoticed bone fractures, burns, and secondary infections. The patient was uncooperative and exhibited hyper-response to noise and contact with dental instruments. For these reasons, dental treatment of the patient was provided in the least invasive manner possible, with less chair time and under appropriate use of physical restraints for limiting unpredictable behaviors. The use of physical restraints was carefully evaluated because of its possible iatrogenic effects on uncontrolled fever and body temperature.
The patient intentionally luxated her tooth and was brought to the clinic at 6 years of age. The extruded mandibular right central incisor was splinted to adjacent teeth with resin and stainless-steel wire. However, repeated self-luxation of the tooth inhibited tooth-bone interface healing and caused prolonged hypermobility following extraction (Fig. 3). At present, the patient is 7 years of age; lack of eruption space for the buccal segment is expected. A Nance holding arch was applied to the maxilla, and serial extraction is planned for space supervision (Fig. 4).
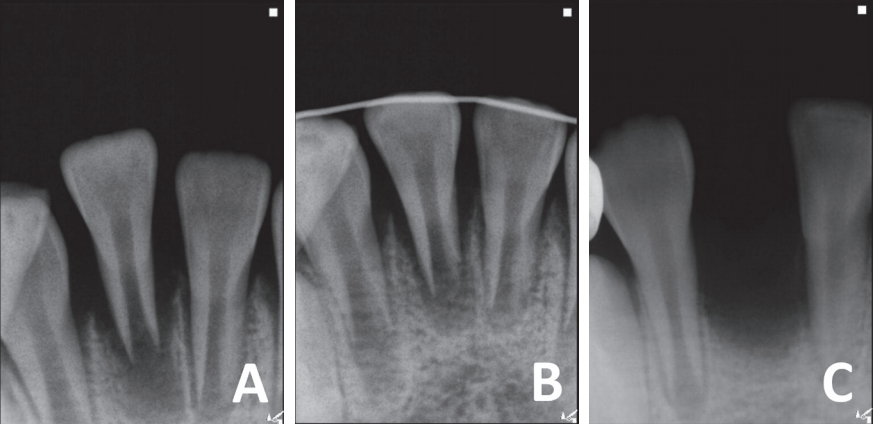
Tooth missing from self-mutilation of mandibular central incisor. (A, B) Selfluxated right mandibular central incisor was splinted to adjacent teeth at the age of 5 years. (C) The affected tooth was extracted due to hypermobility with severe bone loss. (A) Initial visit (B) 2 days, and (C) 6 months after the initial visit.
Ⅲ. Discussion
In this study, dental management of CIPA was described by presenting a 6-year follow-up of CIPA patients who initially visited the dental hospital at 7 months of age and was diagnosed with CIPA at the age of three.
At the patient’s first dental visit, some possible underlying diseases could be suspected from self-oral injuries; however, oral injury itself is not specific to the underlying disease[9]. Because, evaluation of other accompanying symptoms or signs is necessary for differential diagnosis, relevant extra-oral manifestations should be examined and referral to a pediatrician for further evaluation, diagnosis should be considered. Multimodal treatment could be adopted depending on symptoms related with unperceived damages while progression of the CIPA itself is still impossible.
Congenital insensitivity to pain is also called to hereditary sensory and autonomic neuropathies (HSAN) and be subdivide into 5 types. Each can be distinguished by the stage of onset, additional symptoms, and causative genetic mutations. HSAN 1 manifests in adolescence to adulthood and is autosomal dominant genetic disease. Other forms of HSAN are due to autosomal recessive mutations of genes highly expressed in peripheral neurons. While HSAN 2 is expressed in childhood, HSAN 3 - 5 are expressed congenitally. Congenital types of HSAN are differentiated by an absence of fungiform papillae of the tongue in HSAN 3 and accompanying mental retardation with anhidrosis of HSAN 4, which is compatible with CIPA. Patient with HSAN 5 is distinguished from type 4 due to accompanying hypohidrosis and normal mental status[10,11]. Similar to CIPA, self-mutilating behavior and mental retardation are also found in Lesch-Nyhan syndrome (LNS) that results from a defect of the HFPRT1 gene[12]; however, the dystonic movement disorder and hyperuricemia found in LNS are not accompanied in CIPA[12,13].
The first dental case reports of CIPA were released in 1989, describing the necessity of local anesthesia due to vasoconstriction in the case of extractions[8]. However, unnecessity of local anesthesia during ordinary dental procedures cannot be elicited from inability to feel pain. In our case, patient pain expression was observed during caries removal; however, it is not certain whether it equated to the common meaning of pain. The patients who can express a little of pain as well as hot or cold sensation were described previously. For CIPA patients, tactile hyperesthesia is usually found, which is suspected to compensate for algesthesia, and postoperative pain might correspond to unpleasant sensation[14]. Therefore, the use of local anesthesia during ordinary dental procedures can be considered to prevent undue tactile sensation. If the expected extent of dental procedure or anticipated patient reaction to treatment is severe, sedation or general anesthesia can be also considered. Due to dysfunctions of autonomic nervous system, patients with CIPA are prone to regurgitate gastric contents and have hemodynamic instability. Therefore, the sedative or general anesthetic management of CIPA patients can be challenging for its increased risk of regurgitation, aspiration, hyperthermia, and bradycardia that should be carefully managed in the perioperative stages. The types of anesthetic agents and anesthetic procedures are not critical for outcome while the use of anticholinergic drugs for bradycardia is controversial because of the risk of hyperthermia[14-16].
Inability to regulate body temperature with anhidrosis is a specific characteristic of CIPA, and around 20% of these patients die from hyperpyrexia in the first 3 years of life[17]. Inability of sweating due to lacking sympathetic nerve innervation, make difficult to manage body temperature[18,19]. Due to the lack of a homeostatic mechanism in body temperature, dental practice should be carefully strategized to prevent sudden hyperthermia, such as shorter chair time, stress relief methods, and appropriate use of physical restraints. Body temperature could be monitored by manually or automatic continuous device depending on treatment duration and severity. Generally, perioperative body temperature during general anesthesia have been known to be within normal range while in some cases of hyperthermia, it could be controlled by management of room temperature and use of heat insufflation device or cooling blanket. It has been reported that as the nonsteroidal anti-inflammatory drugs, diclofenac and indomethacin which are non-selective COX inhibitors may not effect to hyperthermia while underlying mechanisms are still unknown. Perioperative sedation should be considered to reduce fever from excitement[14]. Besides body temperature, patient position when physical restraints are applied should be monitored as these patients cannot notice twisted or pressured joints due to lack of a pain reflex. If treatment need of patient is not inevitable or urgent, treatment could be delayed if maintaining vital signs as well as body temperature are difficult.
Many threats could be decreased with cautious behaviors; unfortunately, such behaviors cannot be effetely corrected and/or prevented due to accompanying mental retardation[19]. Because secondary infection is suggested to be arised from self-injuries and unperceived damages, use of full denture followed by extractions and patient education for not to bite themselves can be recommended depending on cooperation of the patients and their guardians[8]. Not all damages are prevented and detected through routine follow-up examinations, pediatric dentists should aware possible injuries of intra and extra-oral space and request medical consultation if needed.
Ⅳ. Summary
Despite its low prevalence and lack of subjective symptoms, pediatric dentists should be aware of the characteristics of CIPA and consider various aspects of clinical procedures and their impact on patients, including shorter chair times, stress relief including appropriate use of local anesthesia, and physical restraints in caring for these patients. Referral for medical consultation, medical management, and final diagnosis is necessary, and education for prevention of selfinjury is needed for both patients and guardians.
