 |
 |
| J Korean Acad Pediatr Dent > Volume 46(4); 2019 > Article |
|
초록
매복된 영구 대구치의 치료 방법으로는 교정적 견인, 외과적 재위치, 자가치아이식, 매복치아의 발치 등이 있으며, 이 중 가장 보존적인 방법인 교정적 견인이 권장된다. 그러나 매복된 영구 대구치의 교정적 견인 시 치아를 이용한 고정원의 확보는 고정원의 상실을 동반할 수 있으며, 이러한 한계를 극복하기 위한 노력의 일환으로 골성 고정원 장치가 개발되었다. 본 증례 보고에서는 영구 대구치가 맹출하지 않는다는 주소로 본원에 내원한 3명의 환자에서 매복치아를 외과적으로 노출하여 교정 장치를 부착하고 골성 고정원 장치를 식립하여 성공적으로 견인하였음을 보고하는 바이다.
Abstract
Treatment options for impacted permanent molars include orthodontic traction, surgical repositioning, transplantation, and extraction of the impacted teeth. Orthodontic traction is recommended because it is the most conservative method. However, it has limitations, such as loss of tooth anchorage. In an effort to overcome these limitations, skeletal anchorage devices tailored for orthodontic use were developed. In this case report, 3 patients were diagnosed with impacted permanent molars. The impacted teeth of these patients were surgically exposed, the orthodontic devices were attached, and the skeletal anchorage devices were implanted for the successful traction of the impacted teeth.
Permanent teeth such as the maxillary and mandibular 3rd molars, the maxillary canines, the mandibular 2nd molars, and the mandibular 1st premolars are frequently impacted[1-3]. The prevalence of impaction of permanent molars, excluding the 3rd molar, has been reported to be 1.8% to 9.2%[4-6]. The main causes of impacted permanent molar are insufficient arch length, an ectopic position of the follicle, obstacles in the path of eruption, and failure of the eruption mechanism[7,8]. Eruption of the permanent molar is important because it provides harmony of facial growth and sufficient occlusal support for normal chewing. Failure of this tooth to erupt can cause many problems, such as a decrease in the vertical dimensions of the lower face, extrusion of opposing teeth, malocclusion, the formation of a follicular cyst, pericoronal inflammation, and root resorption in adjacent teeth[9,10].
Treatment options for impacted permanent molars include orthodontic traction, surgical repositioning, transplantation, and extraction of the impacted teeth. Orthodontic traction is recommended, because it is the most conservative method. Surgical repositioning or transplantation can be associated with unwanted side effects, such as ankylosis, replacement resorption, and loss of tooth vitality. In a recent study, transplantation of permanent molars showed a success rate of 11%. In contrast, orthodontic traction showed a success rate of 70%[11].
Anchorage is essential for successful orthodontic treatment. However, tooth anchorage is associated with limitations, such as mobility of the anchor teeth. In an effort to overcome these limitations, skeletal anchorage devices tailored for orthodontic use were developed. The development of skeletal anchorage devices has opened a new paradigm in orthodontic treatment, offering treatment options for many difficult conditions that were untreatable by conventional methods. Absolute anchorage can be achieved with skeletal anchorage devices because the anchorage device is fixed in bone, eliminating anchorage loss that causes dental shifting or tilting, side-effects commonly seen with conventional intraoral anchorage appliances[12]. Additionally, these skeletal anchorage devices are easily manipulated, able to target specific treatment goals, simplify treatment mechanics, and shorten total treatment times[13].
In this case report, 3 patients presenting with a chief complaint of unerupted permanent molars were treated orthodontically. The impacted teeth of these patients were surgically exposed, the orthodontic devices were attached, and traction of the impacted teeth was performed by utilizing skeletal anchorage devices.
A 13-year-old girl was referred to our clinic with a supernumerary tooth in the maxillary left 2nd molar region. In the intraoral examination, the maxillary left 2nd molar was not seen in the oral cavity (Fig. 1A, 1B). Radiographic examination via panoramic and periapical radiographs showed the presence of a supernumerary tooth around the maxillary left 2nd molar (Fig. 1C, 1D). The 3-dimensional cone-beam computed tomography (CBCT) view revealed a supernumerary tooth on the buccal side of the maxillary left 2nd molar (Fig. 1E-1F).
It was determined that the maxillary left 2nd molar was impacted due to the presence of supernumerary tooth on the buccal side of the occlusal surface. Hence, orthodontic force was applied to the impacted tooth after the removal of the supernumerary tooth. It was decided that skeletal anchorage would be used to prevent undesirable loss of tooth anchorage, and to apply effective orthodontic force to the tooth.
The supernumerary tooth was removed under general anesthesia. The maxillary left 2nd molar was surgically exposed, and the button was attached to expose the wire connected to the button in the oral cavity. The mandibular left 3rd molar was extracted and a miniplate (4-hole straight plate; Gssem, Seoul, Korea) was fixed on the ramus using 2 miniscrews (1.6 mm diameter, 6.0 mm length; Gssem, Seoul, Korea). The miniplate was bent and exposed to the buccal side of the mandibular left 2nd molar (Fig. 2).
After 1 week of operation, traction of the impacted maxillary left 2nd molar was initiated with an elastic on the wire connected to the button on the maxillary left 2nd molar and the miniplate exposed in the mandibular left 2nd molar region. A tractional force of 75 gm was applied and measured using a dontrix gauge (Dentaurum, Germany). The end of the wire connected to the button was bent into a shape of a hook and a resin ball was formed to allow placement and removal of the elastic by the patient. Patient was instructed to remove the elastic during meals and to replace it after the meal, as mouth opening could be difficult or the elastic may drop out during mastication. After 4 months, the maxillary left 2nd molar erupted in the oral cavity (Fig. 3). During the traction, a fixed orthodontic appliance was attached to align the crowding dentition due to space deficiency in the upper and lower anterior teeth. After 1 year of traction, the maxillary left 2nd molar completely erupted, the miniplate was removed, and the orthodontic treatment was terminated 27 months after the initiation of fixed orthodontic treatment (Fig. 4).
A 12-year-old girl visited our clinic because her mandibular right molars were not erupted. In the intraoral examination, the mandibular right 2nd premolar and 2nd molar were not seen in the oral cavity (Fig. 5A, 5B). On panoramic radiograph and CBCT view, small cysts surrounding the mandibular right 2nd premolar, the 2nd molar crown were observed (Fig. 5C-5I).
It was determined that the mandibular right 2nd premolar and 2nd molar were impacted due to the cysts in the mandibular right 2nd premolar and 2nd molar regions. Hence, orthodontic force was applied to the impacted teeth after enucleation of the cysts. It was decided that skeletal anchorage would be used to prevent undesirable loss of tooth anchorage, and to apply effective orthodontic force to the teeth.
Under general anesthesia, the mandibular right 3rd molar was extracted and cyst enucleation of the mandibular right 2nd premolar and 2nd molar was performed. Then the impacted mandibular right 2nd premolar and 2nd molar were surgically exposed, and the buttons were attached to expose the wire connected to the button in the oral cavity. And 2 miniscrews (2.0 mm diameter, 6.0 mm length; Gssem, Seoul, Korea) were placed on the buccal side between the maxillary right 2nd premolar and the 1st molar, and between the 1st molar and the 2nd molar (Fig. 6).
After 1 week of operation, 75 gm of orthodontic force was applied to the impacted mandibular right 2nd premolar and the 2nd molar with elastic on the wire connected to the button on the mandibular right 2nd premolar and 2nd molar and the miniscrews placed in the maxilla. Patient was instructed to remove the elastic during meals and to replace it after the meal. After 3 months of traction, the miniscrew placed between the maxillary right 1st molar and the 2nd molar was shaken, removed, and repositioned with a longer miniscrew (1.6 mm diameter, 8.0 mm length; Jeil medical, Seoul, Korea). To prevent the extrusion of the opposing teeth during traction of the impacted teeth, a resin wire splint utilizing multi-strand wire was applied from the maxillary right 1st premolar to the 1st molar. During the traction, a fixed orthodontic appliance was attached to align the entire dentition. After 18 months of traction, the mandibular right 2nd premolar and the 2nd molar were erupted in the oral cavity (Fig. 7). The orthodontic treatment was terminated 22 months after the fixed orthodontic appliance were attached (Fig. 8).
A 13-year-old girl was referred to our clinic with odontoma around the mandibular right 1st molar and tooth impaction. In the intraoral examination, all the 2nd molars and the mandibular right 1st molar were not seen in the oral cavity, and the maxillary right 1st molar was extruded (Fig. 9A, 9B). On panoramic radiograph and CBCT view, an odontoma on the lingual side between the mandibular right 2nd premolar and the 1st molar was observed, and the mandibular right 1st molar, which was locked by the mesially tilted mandibular right 2nd molar and displaced distally, was observed (Fig. 9C-9G).
It was determined that the mandibular right 1st molar was impacted due to the odontoma between the mandibular right 2nd premolar and the 1st molar. Hence, orthodontic force was applied to the impacted tooth after the removal of the odontoma. It was decided that skeletal anchorage would be used to prevent undesirable loss of tooth anchorage and to apply effective orthodontic force to the teeth.
Under general anesthesia, the odontoma between the mandibular right 2nd premolar and the 1st molar was removed. The impacted mandibular right 1st molar was surgically exposed, and the button was attached to expose the wire connected to the button in the oral cavity. A miniscrew (1.6 mm diameter, 6.0 mm length; Jeil medical, Seoul, Korea) was placed on the buccal side between the mandibular right 1st and 2nd premolar for mesial traction, because the impacted tooth was displaced distally and was locked by the posterior tooth. And 2 miniscrews were placed on the buccal and palatal side between the maxillary right 2nd premolar and the 1st molar to apply intrusive force to the extruded maxillary right 1st molar (Fig. 10).
After 1 week of operation, 75 gm of orthodontic force was applied to the impacted mandibular right 1st molar with an elastic on the wire connected to the button on the mandibular right 1st molar and the miniscrew placed on the buccal side between the mandibular right 1st and 2nd premolar. An intrusive force was applied to the maxillary right 1st molar using miniscrews placed in the maxilla. After 6 months of traction, the mesial movement of the mandibular right 1st molar was completed, and extrusive force was applied on the tooth using a miniscrew placed on the buccal side of the maxillary right 1st molar (Fig. 11). Patient was instructed to remove the elastic during meals and to replace it after the meal. During the traction, a fixed orthodontic appliance was attached to align the entire dentition. The orthodontic treatment was terminated 18 months after the fixed orthodontic appliance was attached (Fig. 12).
Tooth impaction is defined as a tooth failing to erupt because of its functional position relative to the occlusal plane due to ectopic eruption, a physical barrier in the path of eruption, or an abnormal eruptive direction[14,15]. If the impaction is due to a physical barrier blocking the path of eruption, the recommended treatment is to provide adequate space in the arch and then remove obstacles, such as odontogenic tumors, cysts, or a supernumerary tooth. If the desired path of eruption is not along the long axis of the impaction, uncovering the tooth, bonding an attachment, and the application of orthodontic traction may be needed. Force level recommended for extrusion of impacted tooth range from 60 to 75 gm[16,17].
In this report, impaction of permanent molars due to physical obstruction was observed in all of the cases. In the past, it was presumed that impacted teeth could spontaneously erupt if the space was acquired and the obstacles were removed. Evidence-based studies, however, show that spontaneous eruption occurs in only 54 - 78% patients and can be delayed for 3 years. In a limited number of patients, spontaneous eruption followed by an acceptable alignment in the oral cavity is possible[18-20]. The possibility of spontaneous eruption varies according to the formation stage of the impacted tooth. The probability of spontaneous eruption failure is 2 times higher in teeth with completed root length growth than in teeth with about three quarters of their root length formed, and more than 3 times higher in teeth with a closed root apex[21]. In cases 1 and 2 of the present case report, the impacted permanent molars had complete growth of the root length but did not have a completely closed root apex at the time of the initial examination. In case 3, the impacted permanent molar had completed both root length growth and root apex closure at the time of the initial examination. Therefore, successful spontaneous eruption was unlikely to occur, and the patients as well as their parents requested orthodontic treatment and traction of the impacted teeth. Hence, immediate orthodontic force was applied to the impacted teeth without waiting for spontaneous eruption.
When a traction force is applied to a tooth, the force required varies depending on the type of tooth to be moved. The greater the root surface area, the greater the force required to move the tooth, and the greater the amount of anchorage required[22]. In this case report, as the impacted permanent molars were to be orthodontically extruded, increased force and anchorage were required compared to that for an anterior tooth or a premolar. When a tooth is used as an anchor, an impacted tooth may not react sufficiently to the traction force. Besides, the tooth used as an anchor, may itself move, leading to undesirable results. In particular, this phenomenon may occur when an impacted tooth is ankylosed. The diagnosis of tooth ankylosis has been considered challenging among clinicians because of the lack of a proper clinical diagnostic tool. A study has shown that the diagnosis of tooth ankylosis can be established by monitoring the response to the traction force. The diagnosis could be made only by therapeutic measures[23]. Hence, application of orthodontic force to tooth using skeletal anchorage is an effective and safe method for orthodontic traction of a heavily impacted tooth. Such procedures should be monitored using radiographs and periodic observation of the reaction. If orthodontic traction of impacted tooth is planned, treatment should be initiated only after providing patients and their parents with a complete information regarding the possibility of failures and alternative modes of treatment.
Absolute anchorage can be achieved with skeletal anchorage devices because the anchorage devices are fixed in bone, eliminating anchorage loss that can cause dental shifting or tilting, side-effects commonly seen with conventional intraoral anchorage appliances[12]. Such skeletal anchorage devices can be easily manipulated, are able to target specific treatment goals, can simplify treatment mechanics, and can shorten total treatment times[13]. However, the skeletal anchorage device may fail or cause complications. A study has reported that most cases of skeletal anchorage device failure occur during the initial 1 to 2 months, and more than 90% failures occur in the initial 4 months[24]. Thus, if the skeletal anchorage device can withstands the orthodontic force for 4 months or more, it can be regarded as stable. In adolescents, cortical bone is thin and has a poor bone quality, and oral hygiene control is often poor. Therefore, there is a high possibility of failure caused by soft tissue inflammation around the skeletal anchorage device[25]. Nevertheless, studies have reported that there is no significant relationship between failure of the skeletal anchorage device and age[26,27]. Consequently, if the skeletal anchorage device is appropriately placed according to guidelines and oral hygiene management is performed well, the possibility of failure can be reduced, even in adolescent patients[24]. In case 2 of the present case report, a miniscrew placed between the maxillary right 1st molar and the 2nd molar was removed after 3 months because of the redness of the surrounding soft tissue and mobility of the screw. After that, a miniscrew of 2.0 mm longer than the existing miniscrew was placed at the adjacent position and successfully maintained. In the case of a patient who requires a strong anchorage because of the need for traction for a severely impacted tooth, a skeletal anchorage device can be considered in patients aged 11 years or older. Both, the patients and their parents should be aware of the possibility of skeletal anchorage device failure and emphasize oral hygiene management.
In this case report, orthodontic traction of impacted permanent molars was performed using skeletal anchorage devices. The suspected obstacles, such as supernumerary tooth, the cyst, and the odontoma, were removed. The impacted teeth were surgically exposed and an orthodontic appliance was attached. A miniscrew or a miniplate was placed as an anchor at the site where the traction would be applied in the desired direction. As a result, all the impacted teeth responded to traction and successfully erupted to a functional chewing position on the occlusal plane.
Fig 1.
At first examination. The line arrows represent the maxillary left 2nd molar and the dotted arrows represent the supernumerary tooth. (A,B) intraoral photograph. The maxillary left 2nd molar is not seen in the oral cavity. (C) Panoramic radiograph. The presence of a supernumerary tooth around the maxillary left 2nd molar. (D) Periapical view. The presence of a supernumerary tooth around the maxillary left 2nd molar. (E-F) CBCT image, horizontal and coronal view. The supernumerary tooth is present on the buccal side of the maxillary left 2nd molar.
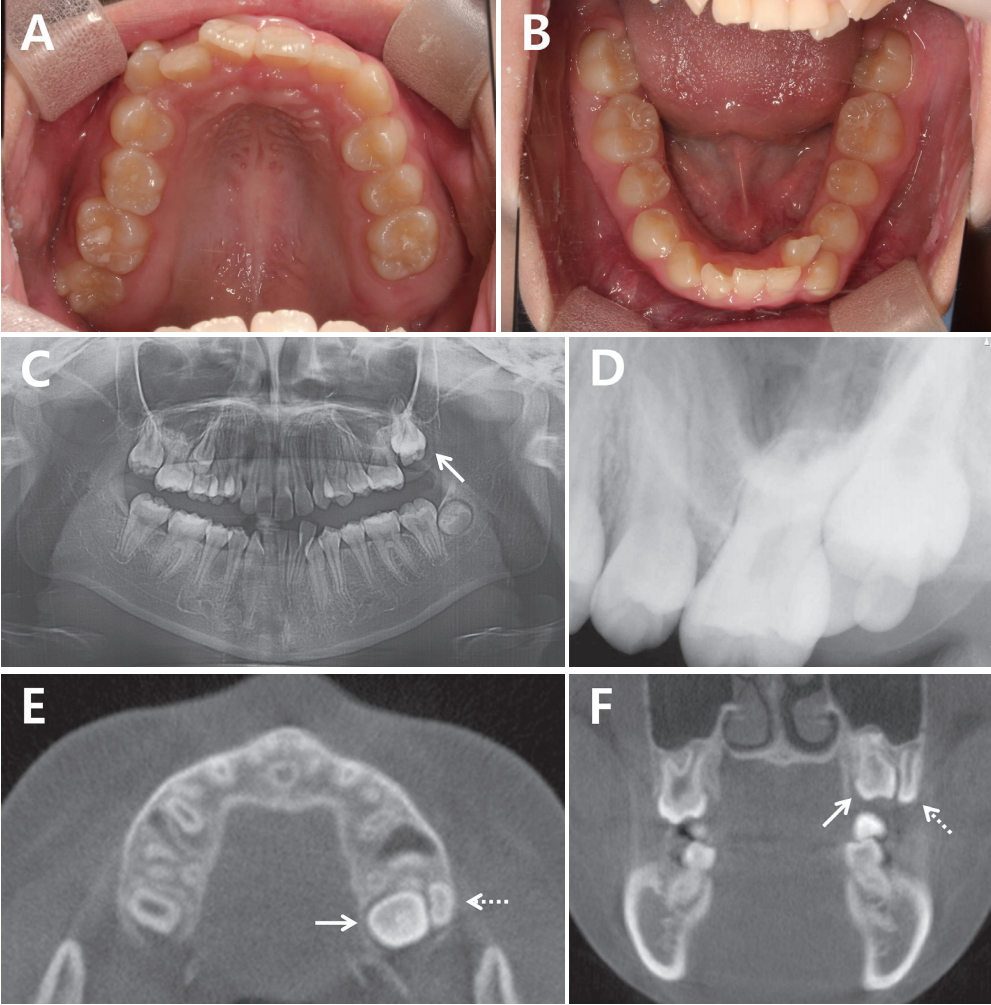
Fig 2.
After implantation of the miniplate and bonding of the attachment. (A-B) Intraoral photograph. (C) Panoramic radiograph. The line arrow represents the maxillary left 2nd molar and the dotted arrow represents the miniplate.
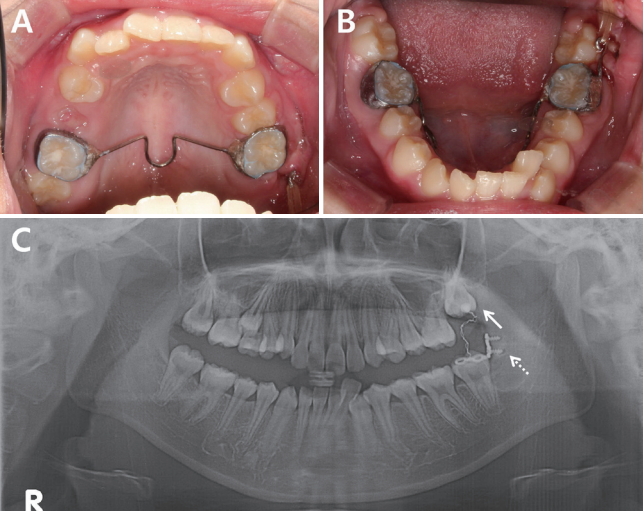
Fig 3.
At 4 months after orthotraction. The maxillary left 2nd molar was erupted in the oral cavity.

Fig 4.
At 27 months after orthodontic treatment. The maxillary left 2nd molar was completely erupted into occlusion.
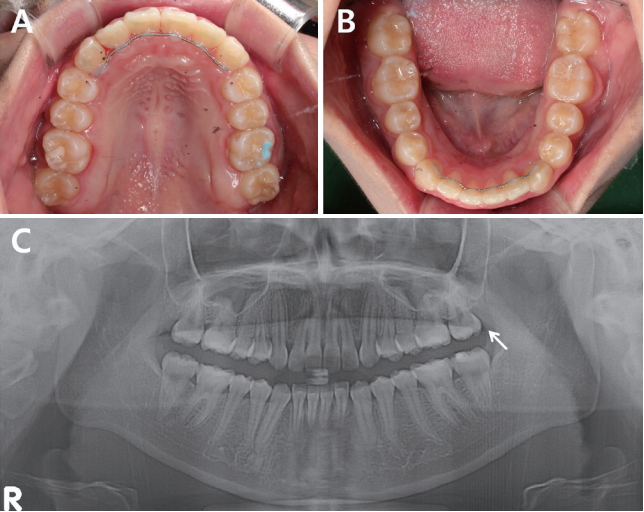
Fig 5.
At first examination. The line arrows represent the mandibular right 2nd premolar and the dotted arrows represent the mandibular right 2nd molar. (A,B) intraoral photograph. The mandibular right 2nd premolar and the 2nd molar are not seen in the oral cavity. (C) Panoramic radiograph. The presence of small cysts surrounding the crown of the mandibular right 2nd premolar and the 2nd molar. (D-F) CBCT image, horizontal, coronal and sagittal view. The presence of a small cyst surrounding the crown of the mandibular right 2nd premolar. (G-I) CBCT image, horizontal, coronal and sagittal view. The presence of a small cyst surrounding the crown of the mandibular right 2nd molar.
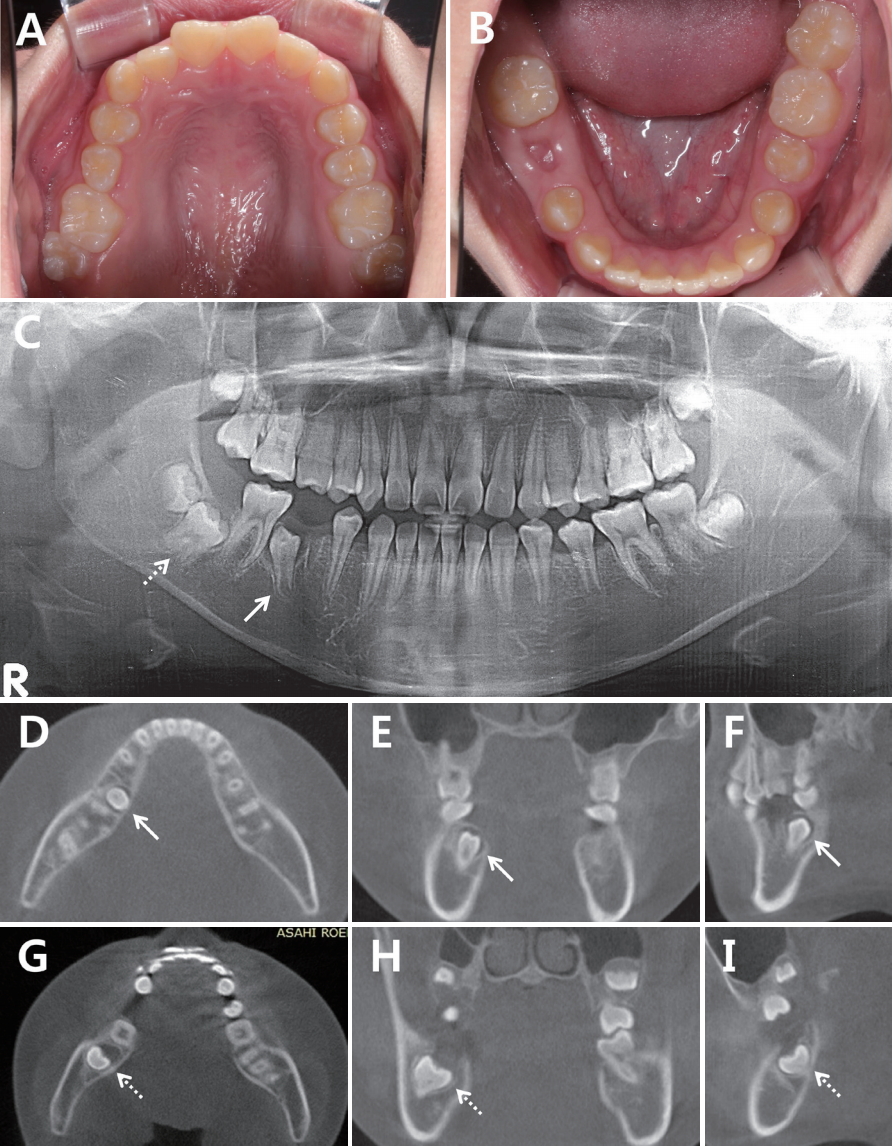
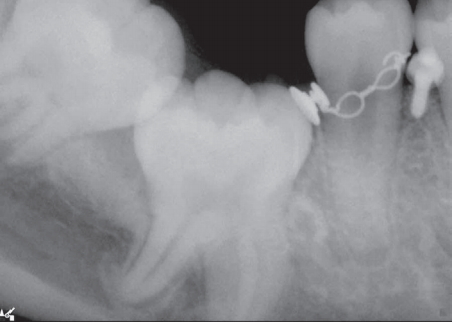
Fig 6.
After implantation of the miniscrews and bonding of the attachments. (A-C) Intraoral photograph. (D) Panoramic radiograph. The line arrows represent impacted teeth and the dotted arrows represent miniscrews.
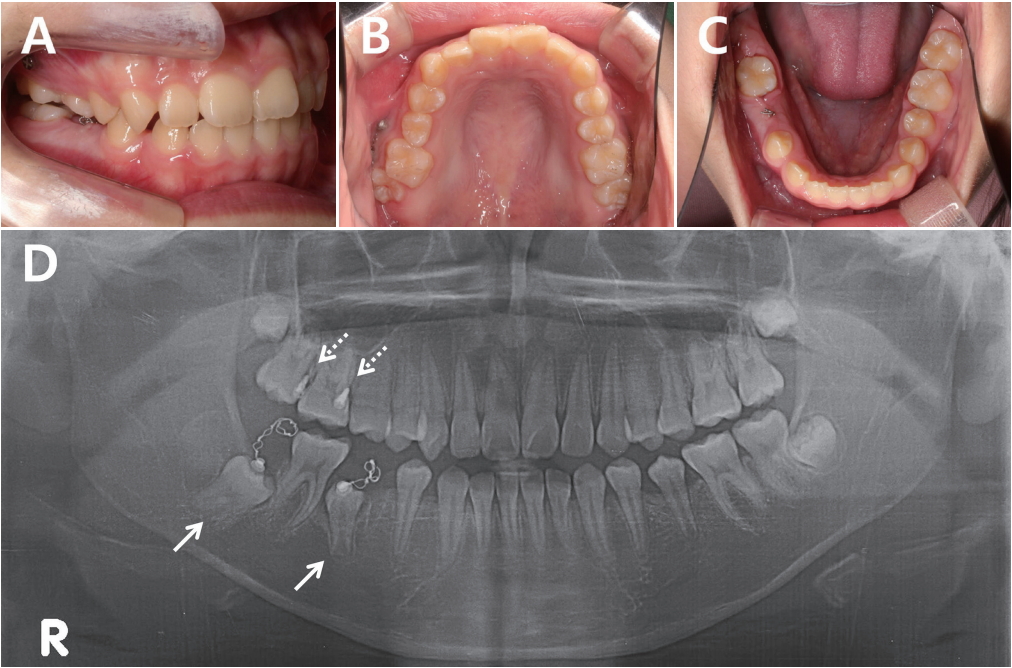
Fig 7.
At 18 months after orthotraction. The mandibular right 2nd premolar and the 2nd molar were erupted in the oral cavity.

Fig 8.
At 22 months after orthodontic treatment. The mandibular right 2nd premolar and 2nd molar were completely erupted into occlusion.
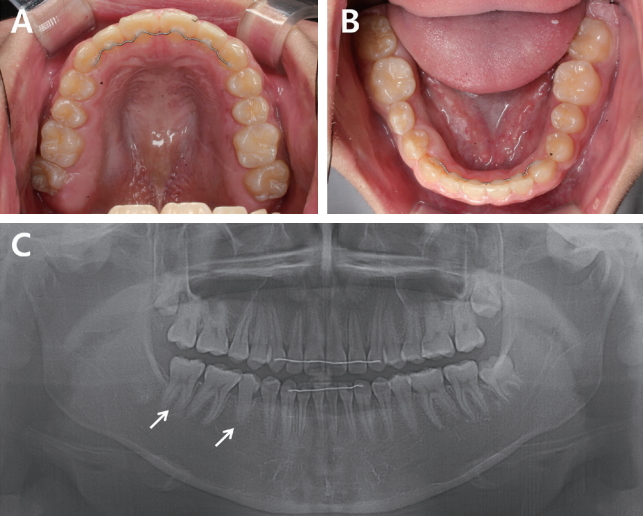
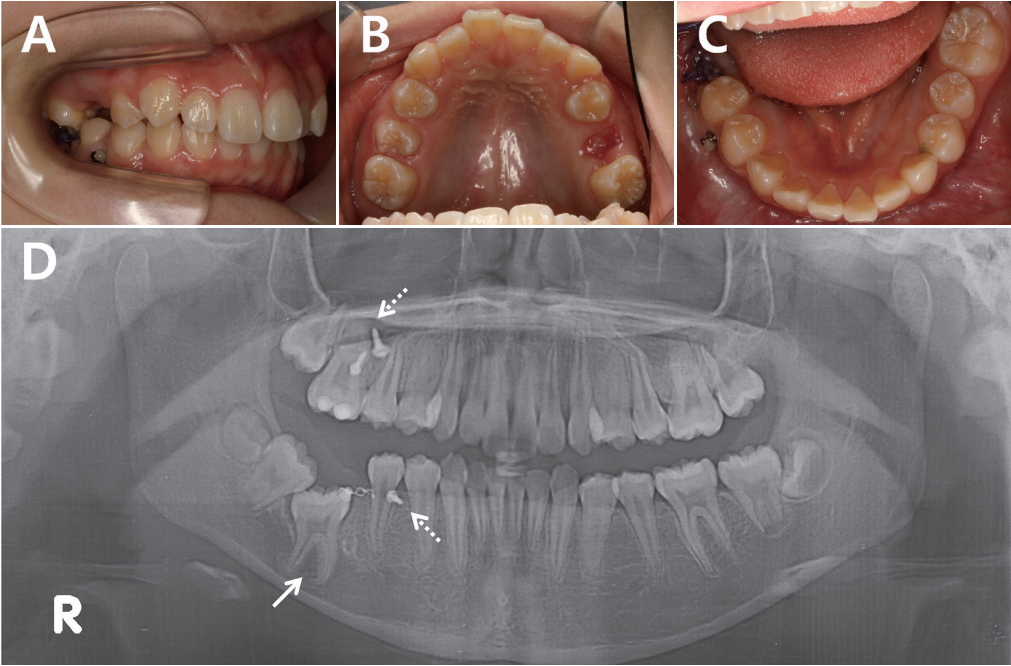
Fig 9.
At first examination. The line arrows represent the mandibular right 1st molar and the dotted arrows represent odontoma. (A,B) intraoral photograph. The mandibular right 1st molar is not seen in the oral cavity. (C) Panoramic radiograph. The odontoma is present at the lingual side between the mandibular right 2nd premolar and the 1st molar. The mandibular right 1st molar that is locked in the mandibular right 2nd molar and displaced mesially. (D-E) CBCT image, coronal and sagittal view. The odontoma is present at the lingual side between the mandibular right 2nd premolar and the 1st molar. (F-G) CBCT image, coronal and sagittal view. The mandibular right 1st molar that is locked in the mandibular right 2nd molar and displaced mesially.

Fig 10.
After implantation of the miniscrews and bonding of the attachment. (A-C) Intraoral photograph. (D) Panoramic radiograph. The line arrow represents an impacted tooth and the dotted arrows represent miniscrews.
References
1. Aitasalo K, Lehtinen R, Oksala E : An orthopantomographic study of prevalence of impacted teeth. Int J Oral Surg, 1:117-120, 1972.


2. Grover PS, Lorton L : The incidence of unerupted permanent teeth and related clinical cases. Oral Surg Oral Med Oral Pathol, 59:420-425, 1985.


3. Dachi SF, Howell FV : A survey of 3,874 routine full-month radiographs. Oral Surg Oral Med Oral Pathol, 14:1165-1169, 1961.


4. Campoy MD, González-Allo A, Pinho T, et al. : Dental anomalies in a Portuguese population. Int Orthod, 11:210-220, 2013.


5. Topkara A, Sari Z : Impacted teeth in a Turkish orthodontic patient population: prevalence, distribution and relationship with dental arch characteristics. Eur J Paediatr Dent, 13:311-316, 2012.

6. Aitasalo K, Lehtinen R, Oksala E : An orthopantomographic study of prevalence of impacted teeth. Int J Oral Surg, 1:117-20, 1972.


7. Flaitz CM, Hicks J : Delayed tooth eruption associated with an ameloblastic fibro-odontoma. Pediatr Dent, 23:253-254, 2001.

8. Johnsen DC : Prevalence of delayed emergence of permanent teeth as a result of local factors. J Am Dent Assoc, 94:100-106, 1977.


9. Raghoebar GM, Boering G, Vissink A, Stegenga B : Eruption disturbance of permanent molars: a review. J Oral Pathol Med, 20:159-166, 1991.


10. Ahmad S, Bister D, Cobourne MT : The clinical features and aetiological basis of primary eruption failure. Eur J Orthod, 28:535-540, 2006.



11. Magnusson C, Kjellberg H : Impaction and retention of second molars: diagnosis, treatment and outcome. Angle Orthod, 79:422-427, 2009.


12. Tsui WK, Chua HD, Cheung LK : Bone anchor systems for orthodontic application: a systematic review. Int J Oral Maxillofac Surg, 41:1427-1438, 2012.


13. Costa A, Raffainl M, Melsen B : Miniscrews as orthodontic anchorage: a preliminary report. Int J Adult Orthodon Orthognath Surg, 13:201-209, 1998.

14. Raghoebar GM, Boering G, Vissink A, Stegenga B : Eruption disturbances of permanent molars: a review. J Oral Pathol Med, 20:159-166, 1991.


15. Proffit WR, Vig KW : Primary failure of eruption: a possible cause of posterior open-bite. Am J Orthod, 80:173-190, 1981.


16. Vibhute PK : Versatile auxiliary orthodontic spring for orthodontic correction of impacted teeth. J Ind Ortho Soc, 45:40-47, 2011.

17. Maeng Y, Oh Sohee : Orthodontic traction of impacted posterior teeth: case reports. J Korean Acad Pediatr Dent, 36:613-618, 2009.
18. Di Biase DD : The effects of variations in tooth morphology and position on eruption. Dent Pract Dent Rec, 22:95-108, 1971.

19. Mitchell L, Bennett TG : Supernumerary teeth causing delayed eruption-a retrospective study. Br J Orthod, 19:41-46, 1992.


20. Gardiner JH : Supernumerary teeth. 12:63-73, 1961.
21. Lee JS, Yoo KJ, Nam SH, et al. : Factors affecting spontaneous eruption of impacted mandibular first molars after surgical exposure. 28:25-32, 2018.

22. Freeman DC : Root surface area related to anchorage in the Begg technique. Am J Orthod Dentofacial Orthop, 53:139-140, 1967.

23. Kim SJ, Kim JW, Choi TH, Lee KJ : Restoration of a vertical alveolar bone defect by orthodontic relocation of a mesially impacted mandibular first molar. Am J Orthod Dentofacial Orthop. 122-132, 2015.

24. Moon CH, Lee DG, Baek SH, et al. : Factors associated with the success rate of orthodontic miniscrews placed in the upper and lower posterior buccal region. Angle Orthod, 78:101-106, 2008.


25. Park HS, Jeong SH, Kwon OW : Factors affecting the clinical success of screw implants used as orthodontic anchorage. Am J Orthod Dentofacial Orthop, 130:18-25, 2006.


26. Park HS : Clinical study on success rate of microscrew implants for orthodontic anchorage. Korea J Orthod, 33:151-156, 2003.
- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 3,276 View
- 167 Download
- Related articles
-
Minor Orthodontic Treatment Using NiTi Wire Exerting Light Force: Case Reports2022 November;49(4)




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



