하악 유구치부에서 발생한 선양 치성 종양의 증례 보고
Adenomatoid Odontogenic Tumor in the Posterior Mandible of a Young Child : A Case Report
Article information
Abstract
선양 치성 종양(adenomatoid odontogenic tumor)은 소아에서 드물게 발생하는 악골의 치성 기원의 종양이다. 보통 10대에서 상악 견치부분에 발생한다.
이 증례는 3세 여환으로 하악 제2유구치의 미맹출을 주소로 개인병원에서 의뢰되었다. 부종과 통증의 병력은 없었다. 파노라마 사진에서 매복된 하악 제2유구치의 주변으로 방사선투과상 병소가 관찰되었고, Cone Beam Computed Tomography (CBCT) 에서는 골 팽창과 함께 방사선 불투과상 병소들이 관찰되었다. 하악 제2유구치의 발치와 함께 병소의 적출과 조직 생검이 시행되었다. 술 후 1년 검사에서 재발을 보이지 않았다.
임상적, 방사선학적 검사를 통해 이 병소는 소아 청소년의 하악 구치부에서 호발하는 법랑모세포 섬유치아종(Ameloblastic fibroodontoma)로 진단되었다. 하지만 생검의 결과를 통해 이 병소는 선양 치성 종양으로 확진 되었다. 이 증례 보고는 매우 어린 나이에 하악 유구치에 발생한 흔하지 않은 선양 치성 종양 증례를 기술하고 있다.
Trans Abstract
Adenomatoid odontogenic tumor (AOT) is a rare benign odontogenic jaw lesion. It usually occurs in the anterior maxilla and is mostly related to impacted canines in teenagers.
A 3-year-old girl was referred from a local dental clinic due to delayed eruption of the right primary mandibular 2nd molar. There was no history of pain or swelling. Radiography revealed a large radiolucency lesion with radiopacities around the unerupted right primary mandibular 2nd molar. Surgical enucleation with extraction of the right primary mandibular 2nd molar and surgical biopsy were performed. Based on the clinical and radiological findings, this lesion was defined as an ameloblastic fibro-odontoma which often develops in the mandible of adolescents. However, this lesion was diagnosed as AOT from the results of the histological examination.
This report aimed to present a rare case of AOT in the posterior mandibular area in a very young patient.
Ⅰ. Introduction
Adenomatoid odontogenic tumor (AOT) is a benign, noninvasive lesion with slow but progressive growth[1]. AOT is rare odontogenic tumor accounting for 3% - 7% of all odontogenic tumors[2-4]. It is commonly located in the anterior region of the maxilla, and only 9% of AOTs develop in the posterior region of the mandible. The age range of patients with AOT is from 3 to 82 years[5]. No less than 68.6% of AOTs are diagnosed in the second decade of life, and more than half of the cases develop in teenager (13 - 19 years)[1,6,7]. There is a difference in sex distribution according to race, but the female to male ratio for all age groups is 2.3:1 generally[8,9]. It is usually associated with unerupted permanent teeth, especially canines.
This report aimed to present a rare case of AOT of a very young child in the posterior mandibular area.
Ⅱ. Case Report
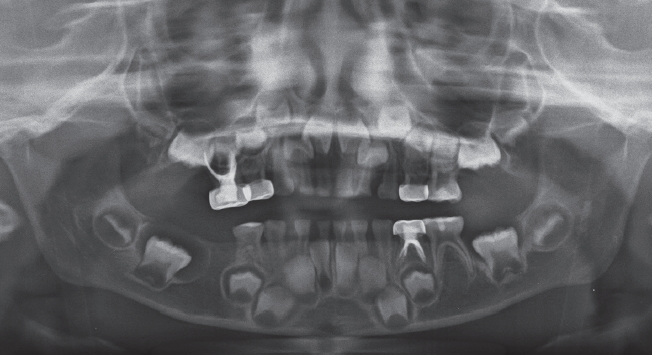
A 3-year-old girl was referred from a local dental clinic due to delayed eruption of the right primary mandibular 2nd molar. Intraoral examination showed an unerupted right primary mandibular 2nd molar and supra erupted right primary maxillary 2nd molar. The patient had no history of pain or swelling. Panoramic radiography revealed a large well-circumscribed unilocular radiolucent lesion involving the unerupted right primary mandibular 2nd molar and displacement of the developing right mandibular 1st molar (Fig. 1). Cone beam computed tomography (CBCT) showed the external boundary of the lesion attached to the middle third of the root of the impacted tooth and faint radiopaque materials in the center of the lesion. The axial view of CBCT showed faciolingual bone expansion of the lesion. A preliminary diagnosis was established as ameloblastic fibro-odontoma (AFO) which commonly develops in the posterior mandible of children. Based on the initial diagnosis, surgical biopsy and enucleation of the lesion were scheduled.

Panoramic view (A) showed a well-defined unilocular radiolucent lesion (white arrow) related with unerupted right primary mandibular 2nd molar and displacement of the developing right mandibular 1st molar. The saggital cone beam computed tomography (CBCT) view (B) showed the external boundary of the lesion was attached to the middle third of the root of the impacted tooth and faint radiopacity (white arrow) in the center of lesion. The axial CBCT view (C) showed expansion of mandibular buccal and lingual cortical plate.
Under general anesthesia, the lesion around the impacted tooth was completely enucleated. Calcified masses were observed inside the lesion (Fig. 2). The excised surgical specimen was sent for histopathologic examination.
The specimen was stained with hematoxylin and eosin (Fig. 3). The duct-like structures, which are typical features of AOT, were prominent in the specimen and the central space in these structures was surrounded by a layer of columnar epithelial cells. Small foci of calcification were scattered across the lesion. From these histopathologic findings, it was confirmed as an AOT.
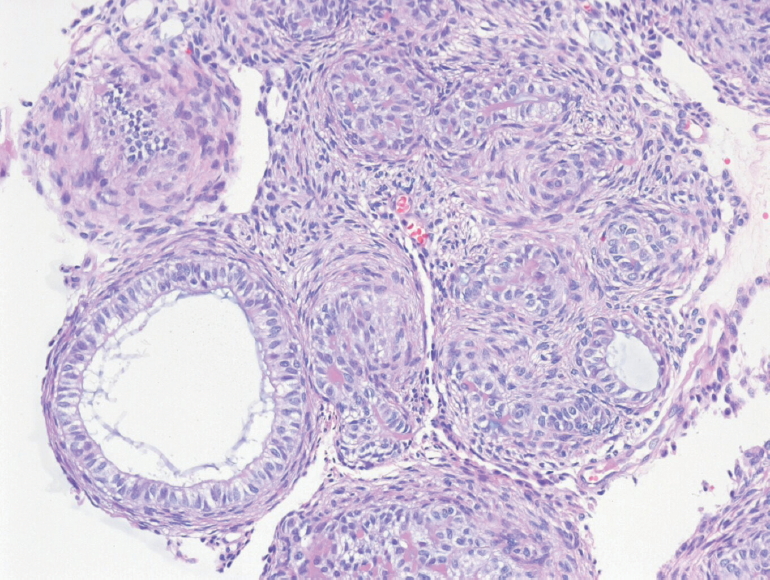
Histological examination Original magnification X 200. The duct-like structures were surrounded by a layer of columnar epithelial cells. The nuclei of these cells were polarized away from the central space.
During the regular examination period, panoramic radiographs were obtained to monitor the eruption of distally displaced right permanent mandibular 1st molar because it was critical to manage the space of the missing right primary mandibular 2nd molar. No evidence of recurrence was observed in the 1st year postoperatively (Fig. 4).
Ⅲ. Discussion
In the 2nd edition of “Histological Typing of Odontogenic Tumours”[10] introduced by World Health Organization, AOT was defined as a tumor of odontogenic epithelium with ductlike structures and with varying degrees of inductive change in the connective tissue. The tumor may be partly cystic, and in some case the solid lesion may be present only as masses in the wall of a large cyst. It is generally believed that the lesion is not a neoplasm.
Philipsen and Reichart[1] established 3 variants of AOT as follows : follicular, extrafollicular and peripheral types. The follicular type is a central intraosseous lesion with an impacted tooth. This type appears as a well-defined, unilocular and radiolucent lesion mimicking dentigerous or follicular cyst. Of the follicular types, 77% are often misdiagnosed as dentigerous cysts[11]. The extrafollicular type is also an intraosseous lesion which is not associated with an impacted tooth. It is located between, above, or superimposed on the roots of erupted teeth. This appearance often leads to a preoperative diagnosis of a residual, radicular, lateral periodontal cyst depending on the site. The peripheral type arises from the gingival tissue and is similar to gingival fibroma or labial gingival epulis.
In previous research that observed the incidence and site of AOT, 60% of the follicular AOT was found in any one of the four canines, while the upper canines alone accounted for 42%. They also reported that the occurrence of AOT was rare in permanent molars, and extremely rare in deciduous teeth[1]. Swasdison et al.[12] reported that only 1 case involved with the maxillary deciduous canine among 67 AOT cases in the Thai population. There was 1 case of follicular AOT with an unerupted deciduous canine in the Japanese population[13]. Other AOT cases involving deciduous teeth were peripheral types[14,15]. In addition to this, Philipsen and Reichart[1] found only 26 out of 532 cases (4.9%) diagnosed as AOT before 9 years of age. Therefore, AOT in this case which was involved with the primary mandibular molar and diagnosed at the age of 3 was exceedingly rare.
Approximately 70% of AOTs are follicular types, in which their radiographic features are well-defined, unilocular radiolucent lesions associated with impacted teeth. The radiographic features of AOT often resemble those of other odontogenic lesions such as dentigerous cyst, calcifying odontogenic cyst, ameloblastoma, ameloblastic fibro-odontoma and periapical disease[5,11,16]. Radiopaque calcification in the lesion is a distinct AOT characteristic that makes a differential diagnosis easier. However, the degrees of radiopacity in the radiographic images vary among the studies on AOT. As reported by Philipsen and Reichart[1], approximately 2/3 of AOT cases had radiopaque calcification inside the lesion. Arotiba et al.[17] found that only 7.1% of cases presented radiopaque foci inside. Faint radiopacities were observed only in CBCT, but not in panoramic radiography in this case. Dare et al.[18] found that periapical radiography tended to assess radiopacities better than panoramic radiography even with minimally calcified materials. A similar study performed by Jiang et al.[19] reported that CBCT was better than panoramic radiography in AOT diagnosis. They reported that only CBCT was able to detect thin and minimal calcifications. Therefore, it was important to perform CBCT to observe radiopacities which were the important features in AOT diagnosis.
The AOT diagnosed in this case was the follicular type. This lesion was easily misdiagnosed as a dentigerous cyst. Dentigerous cyst was distinct from AOT because it only surrounded the coronal part of the impacted tooth. In contrast, AOT usually enclosed both coronal and radicular parts of the impacted tooth. In this study, the lesion attached to the middle third of the root of the impacted deciduous tooth, and the radiopacities in the CBCT helped to rule out dentigerous cyst.
Before histopathologic examination, the lesion was considered as an AFO because it commonly occurs in the posterior mandible of children aged under 10 years. AFO is a rare and benign odontogenic tumor mostly associated with an unerupted tooth[20]. Furthermore, AFO displays a well-defined radiolucent area containing various radiopaque materials in radiographs. AFO usually develops in 9-year-old children on average, which is an important factor to consider in differential diagnosis[21-25].
Surgical enucleation and curettage are first-line treatment modalities for AOT. Considering the nonaggressive characteristics of this tumor, the latest treatment trend regarding AOT is performing a conservative surgical approach by maintaining the affected tooth[26,27]. There were many successful cases of AOTs treated without extraction of the affected teeth[13,28-30]. In most cases with marsupialization of AOT, orthodontic repositioning of the involved tooth was achieved. However, in this case, the tooth had been pushed to nearly the cortical bone of the mandible, and the size of the lesion justified the decision to extract a tooth with the lesion. Further, considering the impatience of children, compliance to orthodontic treatment was questionable. If the tooth was properly positioned for orthodontic movement and other conditions (e.g. age, size of lesion, anatomical structure) were favorable, it would be worth saving the tooth.
Recurrence of AOT is exceptionally rare. It was noted in only 3 of 750 cases in the Japanese population[31]. The patient in this case maintained healthy oral conditions without any sign of recurrence. The space for the congenitally missing #45 tooth was resolved by mesial drift of #46.
In this study, it was difficult to make a definitive diagnosis without examining the specimen under a microscope. Characteristic features, such as duct-like structures, confirmed the presence of AOT. Clinical features and radiographic findings were used to obtain a tentative diagnosis, but they were insufficient for making a final diagnosis. Therefore, histopathologic examination must be performed for a definitive diagnosis. Being aware of rare varieties of the tumor like this case would allow early diagnosis, proper investigation, and prompt treatment.
Ⅳ. Summary
AOTs are uncommon odontogenic benign lesions that are mostly observed in the 2nd decade of life and usually associated with maxillary canines.
In this report, a 3-year-old patient had an AOT located in the right primary mandibular 2nd molar. Since its location and age were uncommon, this lesion was provisionally diagnosed as an AFO. However, histopathologic examination confirmed that this lesion is an AOT. Clinical and radiographic features easily led to a misdiagnosis. Therefore, additional histopathologic examination was necessary in providing a final diagnosis.