ŌģĀ. Introduction
Among the permanent teeth, the first permanent molars play the greatest role in occlusion, function, and development of the dentition[
1,
2]. Proper crown coverage is essential when a permanent first molar is extensively damaged by severe caries or hereditary anomalies, such as molar incisor hypomineralization (MIH), dentinogenesis imperfecta (DI), or amelogenesis imperfecta (AI)[
3]. This task is compounded by the fact that young permanent teeth are partially erupted and will continue to erupt and alter their position in the mouth, which will change the margins of any existing restoration[
4]. Moreover, moisture-control problems, difficulty with coordination due to young age, and short crown height make treatment difficult. In such cases, preformed metal crowns (PMCs, also known as stainless steel crowns) may be useful.
PMCs have long been used to cover molars with defective enamel and they are still recommended as a treatment option for MIH of the posterior teeth[
5,
6]. In many cases of severely damaged permanent first molar crowns in children, PMCs are a successful interim restorative option until a permanent restoration, usually of the full coverage type, can be placed later[
4]. No other type of restoration offers the convenience, low cost, durability, and reliability of such crowns when interim full coronal coverage is required[
7]. They prevent further tooth loss, control sensitivity, and establish correct interproximal and proper occlusal contacts. PMCs have a very long history of use, although their use in the primary dentition is by far the most common. Several studies have reported survival times in excess of 5 years and success rates of 92 - 94% in the primary dentition[
8]. Although the use of PMCs in permanent first molars is widespread, only limited data on their long-term prognosis are available[
9]. Therefore, this study was carried out to evaluate the longevity of PMCs in permanent first molars and identified clinical preoperative variables that may correlate with treatment outcomes.
ŌģŻ. Discussion
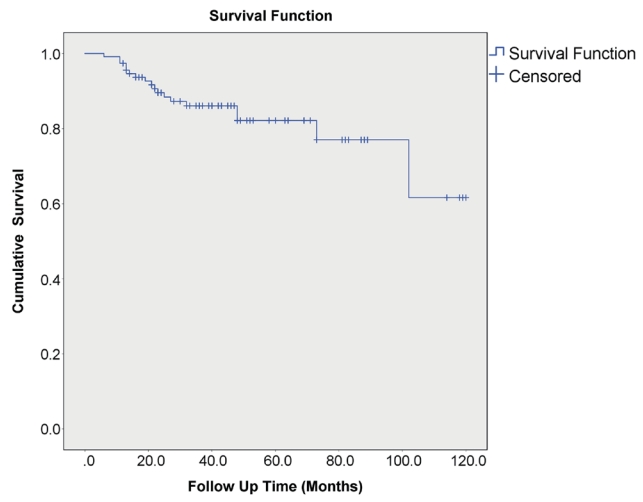
The longevity of dental restorations depends on many different factors related to the restorative material, the patient, and to the dentist[
11]. Although limited data are available on the longevity of PMCs, they are considered long-lasting by many dentists. This is confirmed by the 82.8% 5-year survival rate for PMCs on permanent molars in the present study. Similarly, other studies have shown promising results for PMCs. Chen
et al.[
12] found that most PMCs were judged as clinically acceptable (22/23, 96%) from an evaluation based on modified US Public Health Services criteria with at least 52 months of clinical service. Discepolo and Sultan[
4] reported an 88% overall success rate during an average service period of 45.18 months. Moreover, significant success was noted in patients less than 9 years of age in their study. In contrast, greater success was noted for older subjects in the present study. Teeth emerge, and coordination improves, with age, which may promote proper tooth isolation and adaptation. However, there was no statistical correlation between age and success rate.
In this study, a commonly observed problem was defective restorations. This finding is in agreement with the report by Chen
et al.[
12], who studied permanent molars with AI. They found that 9 out of 27 PMCs were placed with faulty marginal limits, most likely due to the nature of a prefabricated crown and the operatorŌĆÖs inability to identify the size required correctly. Poor marginal sealing may allow microleakage along the interface between the tooth and crown[
13]. This lack of adaptation would allow for bacterial invasion, and thus failure of any present endodontic treatment. Debonding failure can also occur if the crown is not seated properly or does not adapt well to the margins of the tooth, leading to cement washout[
4,
13]. Thus, defective restorations, debonding, and pulp pathology are all closely related.
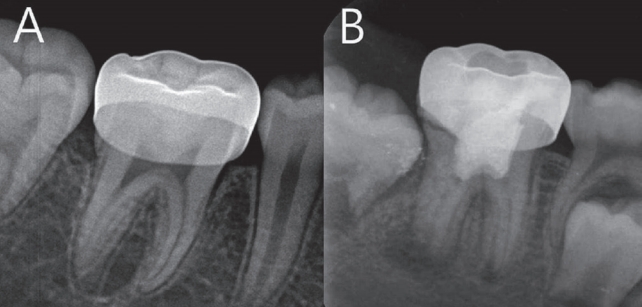
Defective restorations, such as a short crown with open margins, an overall poor fit, or lodging, were predominantly related to initial seating. In view of the potential longevity of these crowns, a periapical or bitewing radiograph is recommended before cementation to check the marginal fit mesially and distally, as it is often not possible to check these areas adequately using an explorer[
14].
The number of proximal contacts was significantly associated with survival, in that teeth with distal cavities failed at 9.225 times the rate of teeth with two proximal contacts. The significant decrease in the survival of teeth with distal cavities may be the result of increased difficulty of the preparation procedure due to compromised access, restricted visibility, and moisture-control problems[
12]. It is often inevitable to place a PMC margin subgingivally in partially erupted permanent molars. Increased subgingival crown height makes isolation and margin placement difficult compared to mesial cavities[
12,
14]. This problem is particularly serious if the permanent second molar is close to emergence.
With regard to dental arch, mandibular molars showed a higher failure rate than did maxillary molars within the confines of this study. This may be related to the fact that the rate of distal cavities in the maxilla was 13.6%, whereas it was 26.8% in the mandible. Jeong
et al.[
15] reported that the repair rate of composite resin restorations in the permanent first molars of children under 12 years old was 1.4 times higher in the mandible than in the maxilla. This may be because the posterior operculum lasts longer in the mandible than in the maxilla, which makes it more difficult to isolate clinically[
15,
16].
In relation to pulp involvement, pulpotomy showed the lowest success rate, Presumably, the lower survival rate of PMCs with pulpotomy occurred because the failure of pulp treatment caused the failure of the PMCs. Moreover, bacterial contamination can occur through the marginal gap of the coronal restoration; thus jeopardizing the long-term success of the pulpotomy procedure[
17]. However, this was not found to be significant according to the Cox multivariate hazard model.
Based on precipitating the need for crown placement, AI and DI had the highest success rate. This was probably because AI and DI teeth are often covered with PMCs for preventive purposes before post eruptive breakdown occurs. This might have led to the higher success rate of PMCs.
This study was performed retrospectively based on medical records, and thus it was difficult to establish a cause of failure when pulp pathology was involved, and failure may in fact have been multifactorial in origin. Roberts
et al.[
18] assessed PMC failure as ŌĆśtrueŌĆÖ and ŌĆśfalseŌĆÖ failures. Crown loss following cement failure or perforation of the occlusal surface as a result of wear was considered true failure, and failure related to endodontic treatment was considered false failure. False failure of PMCs may occur when a pulpotomy is not carried out when it should have been, or when a pulp treatment is performed but fails due to operator error. An example of true failure of a restoration resulting from pulp pathology would be when endodontic therapy is carried out but failure occurs as a result of restoration leakage leading to a recurrence of pulp inflammation[
19]. In addition, coronal leakage is often associated with endodontic failure and a well-constructed coronal restoration has a greater effect on endodontic success than the quality of the endodontic obturation[
20-
22]. Therefore, it is not clear whether pulp pathology is due mainly to a defective restoration or a failed pulp treatment. However, in this study, all pulprelated complications were classified as failures, therefore overestimation of PMC failure might have occurred.
The record review method for identifying PMC failure relies exclusively on data from patientsŌĆÖ electronic dental records and radiographs. Only events documented in patientsŌĆÖ electronic dental records are included in the analysis; therefore, available information regarding events in the records may be insufficient for failure assessment. When conducting routine clinical examinations, perforation due to wear and loosening of PMCs due to cement loss may be overlooked, thus leading to underestimation of PMC failure.
The retrospective nature of this study made it impossible to identify a true causative relationship between preoperative parameters and survival rate. Therefore, the effects of preoperative parameters should be further evaluated in future prospective randomized controlled trials.
Nonetheless, this study is significant in that it evaluated sequelae of PMCs over a long-term follow-up period and determined factors influencing the outcome of PMCs in permanent first molars. The results imply that PMCs can be used in permanent first molars as interim restorations until a permanent restoration can be placed. Interim PMCs do not replace the need for permanent restorations in the future, but the interval allows for the practitioner to determine the optimal timing for replacement. This study identified the factors that influence the success rate of PMCs and may be helpful in establishing treatment guidelines for extensively damaged permanent first molars.











 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



