어려운 구강 문제를 가진 외상당한 청소년 환자의 소구치 자가이식 및 심미적 회복: 증례 보고
Autotransplantation of Premolars and Esthetic Rehabilitation in a Traumatized Teenage Patient with Challenging Oral Problems: A Case Report
Article information
Abstract
어린이의 맹출 중인 치아는 느슨한 치주 인대와 덜 석회화 된 치조골로 둘러싸여 있기 때문에 외상에 취약하다. 외상에 의한 치아의 완전 탈구는 상악 중절치에 가장 빈번하게 발생한다. 탈구된 치아의 재식 후 예후는 구강 외 보존 시간과 상태에 영향을 받는다. 외상당한 전치의 예후가 불량한 경우 소구치의 전치부 자가 이식은 임플란트 보철이 어려운 성장기 청소년 환자의 적절한 치료 방법으로 받아들여진다.
이 증례 보고는 외상당한 전치와 불량한 구강 위생 및 심한 총생을 가진 청소년 환자에서 치근이 완성된 소구치의 전치부 자가 이식을 통한 심미적 회복의 결과를 기술하고 있다. 복잡하고 어려운 구강 문제의 개선을 위해 포괄적이고 장기간에 걸친 치료가 진행되었다.
Trans Abstract
The loosely structured periodontal ligament and low mineralized bone surrounding erupting teeth provide minimal resistance to an extrusive force. The maxillary central incisors are the most frequently avulsed due to trauma. The prognosis of replanted teeth is affected by extra-alveolar period and conditions. Implant-supported restorations are contraindicated in adolescent patients with poor prognosis traumatized teeth. Autotransplantation of premolar to the anterior region provides a viable treatment alternative.
This case report describes the autotransplantation of premolars and esthetic rehabilitation in a teenage patient with traumatized incisors, poor oral hygiene, and severe crowding. Comprehensive and long-term treatments were performed to improve complex and challenging oral problems.
Ⅰ. Introduction
In children from 7 to 9 years of age, avulsion of teeth occurs most often due to the loosely structured periodontal ligament and low calcified bone surrounding erupting teeth[1]. The maxillary central incisors are the most frequently avulsed teeth[2]. The root resorption of replanted teeth after avulsion is associated with the type and length of extra-alveolar storage[3,4]. The degree of contamination and the period of dryness were the major risk factors for resorption[5]. Treating a teenager with hopeless traumatized anterior teeth can be very challenging and requires comprehensive long-term management because implant-supported restorations are contraindicated during continuous growth of the alveolar process[6]. Autotransplantation of premolars to the anterior region can provide a viable treatment alternative that addresses complex challenges[7].
This case report presents the detailed procedure of esthetic rehabilitation with premolar autotransplantation in a traumatized teenage patient. Comprehensive treatment and management were required in challenging oral problems such as severe gingival inflammation and crowding.
Ⅱ. Case Report
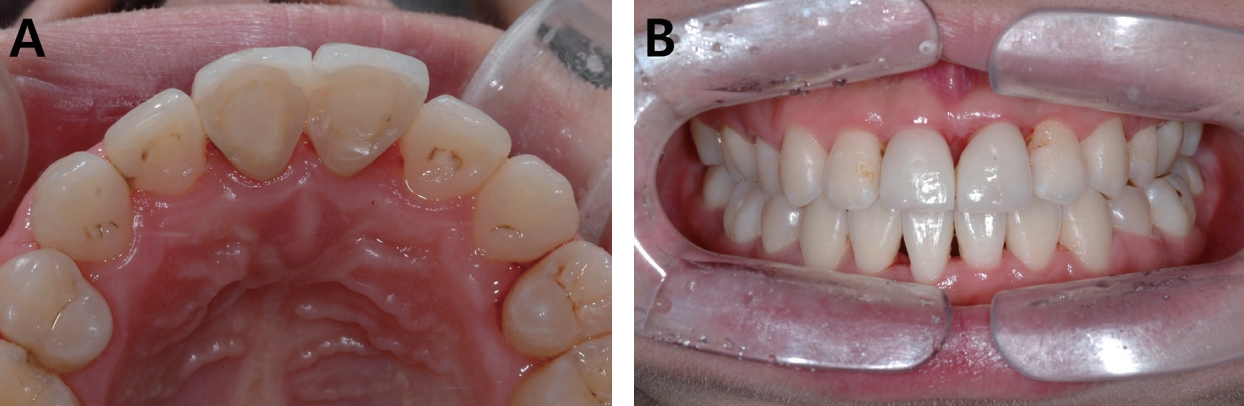
A 9-year-old boy visited Gangneung-Wonju National University Dental Hospital with a chief complaint of “3 hours ago, I fell and injured my teeth”. The patient’s bilateral maxillary central incisors had been stored in milk after avulsion. Resinwire splinting after emergency replantation of avulsed teeth was performed in department of oral & maxillofacial surgery (OMFS). The next day, the patient was referred to the pediatric dentistry from OMFS for comprehensive evaluation and followup treatment. On radiographic examination, nearly complete root developments of replanted teeth were observed (Fig. 1). Risk of root resorption was high due to delayed replantation more than 3 hours. For these reasons, pulp extirpation of the replanted central incisors and apexification with calcium hydroxide were performed (Fig. 2A).
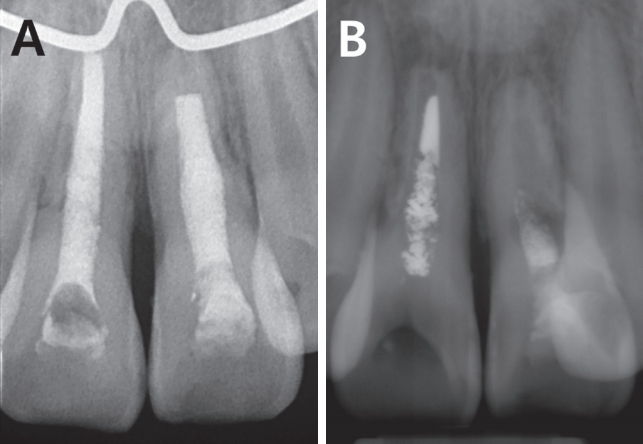
Periapical radiographs of the maxillary central incisors after filling the root canals with calcium hydroxide paste. (A) 8-month follow-up, (B) 50-month follow-up.
The patient did not come to follow-up after recall visit at 11-year of age. The patient returned to the pediatric dentistry 3 years later and oral hygiene was severely poor. In periapical radiograph, internal and external root resorptions of the maxillary central incisors were observed (Fig. 2B). Changing of calcium hydroxide paste was performed but long-term prognosis of maxillary central incisors was poor. Since the patient had a severe crowding in permanent dentition, orthodontic treatment was performed. (Fig. 3A). The clinical examination showed an acute nasolabial angle and convex lateral profile (Fig. 3B). The cephalometric analysis demonstrated a Class Ⅱ skeletal relationship. The maxillary and mandibular anterior teeth were proclined and lips were protrusive (Fig. 3C). Based on the pre-orthodontic measurements and analysis, it was decided to extract 4 first premolars for improvement of facial profile and occlusion. Autotransplantation of the mandibular premolars into the anterior region after extraction of maxillary central incisors was included in treatment plan. Prior to orthodontic treatment with autotransplantation, management of gingival inflammation and oral hygiene was required. Scaling, lower anterior flap surgery, upper anterior and posterior curettage were performed. Continuous plaque control including chlorhexidine application and patient instruction were required over the entire period of treatment.

Pre-orthodontic photographs and radiograph. (A) Intraoral photograph, (B) Extraoral photograph; lateral view, (C) Cephalometric radiograph.
1 year after start of orthodontic treatment, maxillary central incisors were extracted. The donor mandibular first premolars were extracted slowly and as atraumatically as possible. The recipient sockets of anterior region were prepared a little larger than root of premolars. Surgical round bur at low speed under saline cooling was used for preparation of the socket. Both premolars were autotransplanted in same side extraction socket of the maxillary central incisors (Fig. 4A). Fixation of premolars was maintained for seven weeks. The root canals of the autotransplanted premolars were filled with calcium hydroxide paste (Fig. 4B). Seven weeks after autotransplantation, copper Ni-Ti wire was inserted into the #11 (#44) and #21 (#34) brackets for levelling (Fig. 5). At the same time, occlusal reduction of #11 and 21 was performed.

Periapical radiographs of autotransplanted mandibular first premolars. (A) Immediately after autotransplantation, (B) Root canals filled with calcium hydroxide state, (C) Root canals filled with gutta percha.
Bony healing around the transplanted premolars was observed 1 year after autotransplantation. The root canals were permanently filled with gutta percha because additional apical lesions or symptoms were not observed (Fig. 4C). After 2 years and 2 months of orthodontic treatment, all orthodontic appliances were removed (Fig. 6). The patient was referred to the prosthodontics for maxillary anterior prosthesis. 9 years after the patient’s first visit, the final setting of porcelain-laminate veneers was completed (Fig. 7).
Ⅲ. Discussion
Long-term prognosis of an avulsed tooth worsens the longer the tooth is out of socket. The best alternative storage medium is milk if culture media such as Hanks balanced salt solution (HBSS) is not available[8]. Most replanted teeth demonstrate ankylosis followed by inflammatory or replacement resorption after a certain period of time[9]. At the first visit of this patient, maxillary central incisors were stored in milk and replantation of teeth was performed 3 hours after injury occurred. External root resorptions were observed 10 months after replantation and internal root resorptions were also observed when the patient returned to the hospital 3 years later.
Placement of implants in growing regions is found to be inappropriate in children and young adolescents[10]. The osseointegrated implants stay in their original position and do not participate in growth[11]. Autotransplantation of premolars to the anterior region is a treatment modality with high success rates[12]. In long-term studies of autotransplanted teeth with immature root development, the 10-year survival rate was reported to be 87 - 95%[13]. This survival rate appears to be equal to implants and fixed prosthetic appliances. The healing potential of periodontal ligaments can be as low as 55% in autotransplantation of the teeth with closed apex[14]. Success of transplantation of mature teeth can be ensured with adequate endodontic therapy of the pulp space[15]. Periodontal ligament cells can be damaged mechanically during extraction or bio-chemically due to various extra-oral conditions and favorable periodontal ligament healing is the critical factor for success. In the present case, the patient was 16 years old at the time of premolar autotransplantation and root development was completed with a closed apex. At the 3-year follow-up after autotransplantation, clinically no discomfort or pain was occurred and well-defined periodontal ligament space with lamina dura was observed in periapical radiograph (Fig. 8).
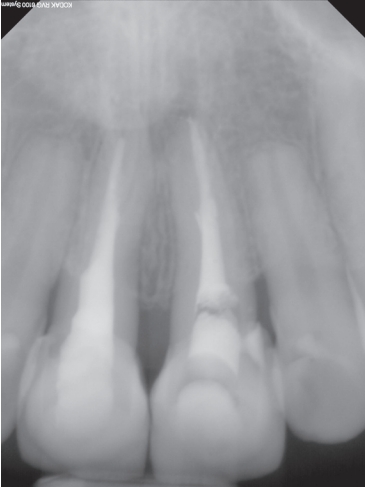
Periapical radiograph of autotransplanted premolars at 29-month follow-up after autotransplantation surgery.
Treating traumatized teeth in teenagers requires long-term observation and management. Pubertal hormonal changes and inadequate plaque control induce interdental papillary swelling[16,17]. Maintaining oral hygiene is more difficult in crowded dentition. In teenage patients, esthetic and functional rehabilitation of challenging oral problems such as trauma, caries, gingival inflammation and malocclusion is essential in terms of self-confidence and psychological development. Pediatric dentists play a vital role in the long-term and comprehensive management of complex oral problems in children and adolescents.
Ⅳ. Summary
Treating a teenage patient with avulsed maxillary incisors, severe crowding and gingival inflammation can be challenging. In this patient, autotransplantation of premolars to anterior region was performed and esthetic rehabilitation was achieved through comprehensive and long-term treatments including orthodontic treatment and management of oral hygiene.