 |
 |
| J Korean Acad Pediatr Dent > Volume 47(3); 2020 > Article |
|
ìŽë¡
êžëìŠë§ íìíë¬Žë ¥ìŠ(Glanzmann Thrombasthenia, GT)ì ììŒì첎 ìŽì± ì ì ìŒë¡ ëíëë í¬ê·í ì ì²ì± ì§íìŒë¡ íìí êž°ë¥ì ìŽììŽ ììŽ íì¡ ìê³ ì¥ì 륌 볎ìŽë©° ëíì ìž ìŠìì ì§íìŽ ì ëì§ ìë ì¶íìŽë€. 1918ë
ìì곌ìì¬ êžëìŠë§ì ìíŽ ì²ì ë³Žê³ ëììŒë©° êžëìŠë§ìšë³(Glanzmannâs disease)ìŽëŒê³ ë ë¶ëŠ¬ ìŽë€.
GTë ëšì±ê³Œ ì¬ì±ìì ëë±íê² ëíëê³ , ì€ë, ìžë íëì€ ë± ê·Œì¹ê²°íŒì íë ê³³ìì ë§ìŽ ë°ìíë©°, ëëµ 1,000,000ëª
ë¹ 1ëª
ìì ë°ê²¬ëë€. ì°ëŠ¬ëëŒììë 2018ë
ì§ë³êŽëŠ¬ë³žë¶ í¬ê·ì§í곌ì ë°ë¥Žë©Ž 200ì¬ëª
ì íìê° ë³Žê³ ëê³ ìë€.
ìììŠìì ì ìì¶í, ë°ìì¶í, ë¹ ì¶í, ì¹ì ì¶í ë±ìŽ êŽì°°ëê³ , ì ì¹ì ìë°ì íëœììë ìíì ê³ ë €íŽìŒ í ì ëì ì¶íìŽ ë°ìí ì ìë€. ì¹ë£ì ìŒë°ì ìž ëª©íë ì¶í ì방곌 ì§íìŽë€. ì¬ë¬ ê°ì§ ì§íì ìí ì²ì¹ìë ì¶íìŽ ì§ìëë©Ž íìí ìíì íŽìŒ íë€.
ììì¹ê³Œìì¬ë 구ê°ì ì²ê²°í íì¬ ì¹ììŒê³Œ ì¹ì ì°ììŠì ìë°©íšìŒë¡ìš ì¹ì ì¶íì ìµìííê³ , êµ¬ê° ìì곌 ê·ì¹ì ìž ì¹ê³Œ ê²ì§ì ì€ìì±ì 죌ì§ììŒìŒ íë©°, ì¹ê³Œì¹ë£ì ì¶íì ëë¹í ì¹ë£ê³íì ì늜 ë° ìžì¬í ì§ë£ê° íìíë€.
GT륌 ëë°í ë§6ìž ì¬ìë¡ ì¹ìì°ììŠì 죌ìë¡ ëŽìíì¬ ìì°íì§ì-ì°ì륌 ìŽì©í í¡ì
ì§ì íì ë ì§ìë³µì ìííììŒë©° ì í ì¹ë£ë¶ìì ìë°ì§íìŽ íìíìë€.
Abstract
Glanzmannâs thrombasthenia (GT) is a rare, autosomal recessive inherited congenital disorder, characterized by impaired blood coagulation due to platelet dysfunction. It was first reported by the pediatrician Glanzmann in 1918.
GT affects both males and females, and it is more common in regions of the Middle East, India, and France, where intermarriage is common. It has an incidence of about 1 in 1,000,000 people. In South Korea, according to the Division of Rare Diseases, Korea Centers for Disease Control and Prevention, around 200 cases have been reported in 2018.
Clinical symptoms include petechia, ecchymosis, epistaxis, and gingival bleeding. The spontaneous loss of deciduous teeth can result in excessive bleeding with that blood transfusion should be considered. Preventing hemorrhages and hemostasis are most important factors in dental treatment. Local bleeding can be controlled by compression, but platelet transfusion can be required by prolonged bleeding.
Pediatric dentists can minimize the gingival bleeding by control of the oral hygiene to prevent gingivitis and dental caries. The importance of oral hygiene and periodic recall check-up should be emphasized. During dental treatment, the examination and the treatment plan of patient should be modified to prevention of hemorrhages carefully.
A 6-year-old girl with GT was referred for the treatment of dental caries, and resin restoration was performed under nitrous oxide inhalation sedation. After treatment, compression was required for the bleeding control.
Glanzmannâs thrombasthenia (GT) is a rare, autosomal recessive inherited bleeding disorder due to platelet dysfunction[1]. It was first described by the pediatrician Eduard Glanzmann in 1918, and it is called Glanzmannâs disease also. It is a congenital bleeding disorder with normal platelet count and morphology, but impaired platelet function. The abnormal formation of glycoprotein (GP) IIb/IIIa impairs the platelet function, which is essential for blood coagulation, resulting in improper hemostasis[2,3].
The main clinical manifestation of GT is hemorrhage and difficult-to-control bleeding[4]. The prolonged bleeding time, mild to moderate bleeding tendency, and poor aggregation of platelets are observed in common. The bleeding tendency was variable. Patients typically experience mucocutaneous bleeding during the neonatal period and infancy, bruising and nose bleeding in childhood, and excessive menstrual bleeding in adolescence. Trauma, surgery, and dental treatment could cause to prolonged bleeding tendency. Excessive bleeding is expected during delivery.
Children are often diagnosed before the age of 5 years by unexpected spontaneous mucocutaneous bleeding. Excessive bleeding after deciduous tooth extraction is often the first sign of GT[5].
The purpose of this case report was to present the clinical findings and dental considerations while treating pediatric GT patients.
A 6-year-old girl was referred from a pediatric dentist to the dental hospital for the treatment of dental caries.
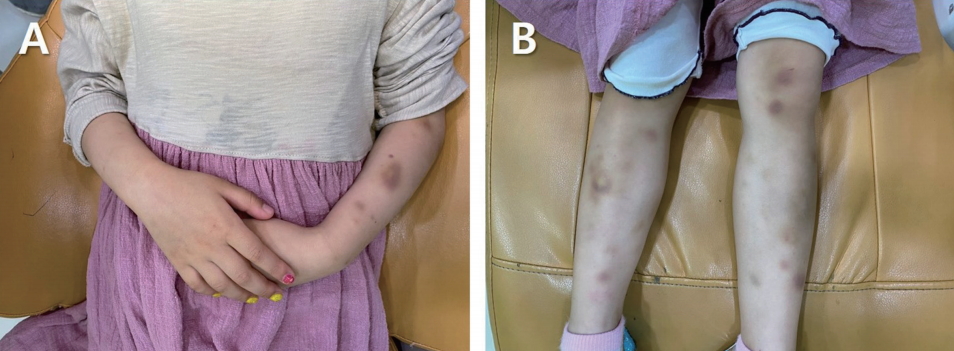
The information was obtained from parents. When the patient was 1 month old, a bruise was observed on the cheek and bruises spread out to the elbow at 2 months later. The patient diagnosed with GT from various tests. The patient would bruise easily on the skin, and often experienced oral bleeding and gingival bruising after toothbrushing.
From the medical consult, the patient was having outpatient follow-up visits and no prescription for GT. No pre-medication for dental treatment was required. Blood transfusion would be needed during dental treatment due to excessive bleeding.
At the first examination, multiple bruises were seen on the arms and legs (Fig. 1). Several teeth with caries were observed and bruising was shown on the buccal gingiva of the right maxillary deciduous lateral incisor to molar area, and the labial gingiva of the mandibular anterior area (Fig. 2). On the radiographic examination, interproximal dental caries of the right deciduous maxillary molars and the both right and left deciduous mandibular molars were observed (Fig. 3).
The patient was afraid of treatment due to frequent examinations and hospital visits, and the behavior pattern was Frankl rating scale 1. Treatment plan to restore dental caries with composite resin under nitrous oxide inhalation sedation has been established. Considering the gingival bleeding, the treatment was divided into three visits to treat one quadrant each time. For the excessive bleeding, platelet transfusion was arranged with the pediatrician.
The patient was treated under nitrous oxide inhalation sedation. A rubber dam was used while treating the proximal surfaces of the left deciduous mandibular molars, and resin restorations were performed as usual. After treatment, there were gingival bleedings where the rubber dam clamp and wedge were placed. Even though compressed the bleeding spot with gauze for 30 minutes, the blood was oozing from the gingiva (Fig. 4). The bleeding seemed not too severe, the patient was discharged with the parental consent, and instructed to call back if the bleeding persisted. The parents informed by phone that blood was oozing for 4 hours after returning home.
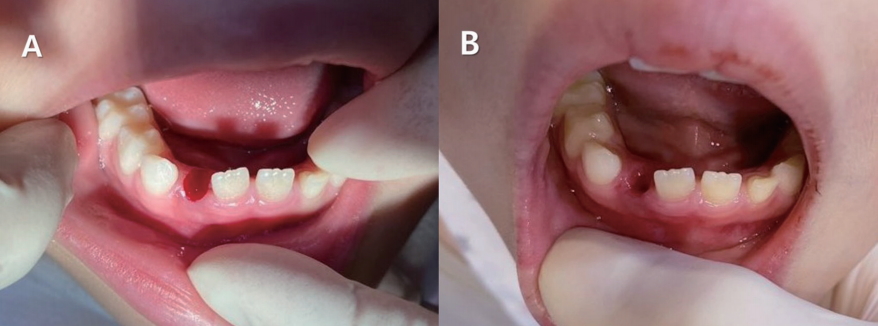
At the second visit for treatment, there was bruising on the labial gingiva of the left mandibular central incisor, buccal gingiva of the left deciduous mandibular canine to second molar area, and buccal gingiva of the right mandibular second molar (Fig. 5). Resin restorations of the proximal surfaces of the right mandibular molars were performed, and the bleeding was lesser than the first treatment (Fig. 6). The patient was discharged after compression for hemostasis.
At the third visit for treatment, there were no specific findings in the oral cavity. Resin restorations were performed on the proximal surfaces of the right deciduous maxillary molars, and gingival bleeding was similar to the first treatment (Fig. 7). After 30 minutes of compression, the bleeding was reduced, and the patient was discharged. The parents confirmed by phone that there were no bleeding problems.
The patient visited with a chief complaint of a mobility of right deciduous mandibular lateral incisor. The tooth was extracted after applying topical anesthetics. After 30 minutes of biting a gauze, the bleeding was controlled (Fig. 8).
The patient and parents were instructed the importance of periodic dental examinations and oral hygiene practices at home for the prevention of gingivitis and dental caries.
Hemostasis is a physiological well-controlled complex process. This process has three main components including vascular system, platelets, and coagulation factors. Congenital bleeding disorders occur when deficiencies of these components. The most well known is Hemophilia. Hemophilia is a coagulation disorder caused by deficiency of factor VIII (hemophilia A) or factor IX (hemophilia B). It is inherited as X-linked recessive condition[6]. von Willebrand disease is the commonest congenital bleeding disorder characterised by abnormalities in platelet adhesion and aggregation due to a deficient of von Willebrand factor. It is an autosomal dominant condition, and affects both males and females[6]. GT is an extremely rare bleeding disorder caused by inherited platelet function disorders. Its clinical manifestation include abnormalities in bleeding time, clot retraction, and a normal platelet count and morphology[7].
GT occurs because of genetic mutations that result in the absence or low levels of platelet surface GP IIb/IIIa, resulting in platelet dysfunction. The genes for both GP are on chromosome 17[8]. GP IIb and IIIa are receptors of fibrinogen, and when they are deficient, the fibrinogen cannot link the platelets together. The deficiency of GP IIb/IIIa interrupts platelet aggregation and causes a bleeding tendency[3]. Since GT patients show normal levels of platelet count, prothrombin time, and activated partial thromboplastin time, it is important to ask for the patientâs bleeding tendency and history thoroughly.
Menorrhagia during initial menstrual cycles is most common among GT patients, followed by petechia, ecchymosis, epistaxis, and gingival bleeding. Gastrointestinal bleeding, hematuria, and hemarthrosis are rare[4]. Epistaxis can occur due to the common childhood habit of nose picking, which damages the blood vessels in the nasal mucosa and often leads to excessive bleeding. It rarely occurs in adults, as the risk of bleeding decreases with age[2]. Gingival bleeding is a common symptom, and it is often caused by gingivitis due to poor oral hygiene. Spontaneous loss of deciduous teeth can cause excessive bleeding that requires blood transfusion[4]. It is difficult to estimate the intensity of hemorrhages, because the intensity can differ even between related patients carrying the same mutation[4,9].
The major goal of management is to prevent hemorrhages and achieve hemostasis. Physical activity that can cause bleeding should be avoided, and drugs that interfere with platelet functions, such as aspirin or non-steroidal anti-inflammatory agents, are contraindicated. Frequent hemorrhages can cause iron deficiency anemia. Especially during childhood and adolescence, when rapid development occurs, a large amount of iron is required. To prevent iron deficiency anemia, administration of iron supplements and folic acid is recommended[10]. Local bleeding can be treated by compression, but for prolonged bleeding, platelet transfusion may be required[11]. Repetitive platelet transfusions can cause alloimmunization, wherein antibodies against GP or human leukocyte antigens (HLA) could be formed on the surface of the donorâs platelets. Therefore, transfusion of HLA-compatible platelet concentrates should be considered[12].
GT is a very rare disease that is inherited as an autosomal recessive condition. It affects both males and females. It is more commonly observed in the Middle East, India, and France, where intermarriages are frequent[13]. There were 130 cases reported worldwide by 1969[14], and the disorder has an incidence of about 1 in 1,000,000 people[15]. In South Korea, it was first reported in 1979, and 15 cases were documented in 1992[10]. According to the Division of Rare Diseases, Korea Centers for Disease Control and Prevention, around 200 cases have been reported in 2018.
Pediatric dentists should instruct the importance of dental caries prevention and oral hygiene to minimize gingival bleeding due to gingivitis and dental treatment. Regular dental examination is needed for oral health maintenance. Local anesthesia of 2% lidocaine with 1 : 100,000 epinephrine can be administered without the risk of excessive bleeding[4]. For the bleeding control after tooth extraction or the loss of deciduous teeth, hemostasis can be achieved by applying resorbable oxidized cellulose or plastic splint, or suturing[4,5]. While preparing for hemorrhages that may occur with dental treatment, dentists should keep in mind the bleeding tendency and history of the patient. Medical consultation should be done to provide platelet transfusion when needed.
In this case, the patient did not have a severe bleeding tendency. Compression was enough to achieve hemostasis after dental treatment. After observing the hemostasis in the four visits, the long time required for achieving homeostasis at the first treatment was thought that caused by improper compression. Periodic examinations and oral hygiene maintenance are needed to prevent severe dental caries that may require root canal treatment and tooth extraction in the future. It is believed that thorough preparation will be needed for treatment that is expected to cause excessive bleeding.
Glanzmannâs thrombasthenia is a rare inherited disorder characterized by platelet dysfunction. The main symptom is uncontrolled bleeding. Pediatric dentists should minimize factors that cause oral hemorrhages by conducting periodic examinations and giving instructions regarding oral hygiene maintenance. The history of bleeding tendency and severity should be recorded and sufficient preparation for excessive bleeding that may occur during dental treatment is advisable.
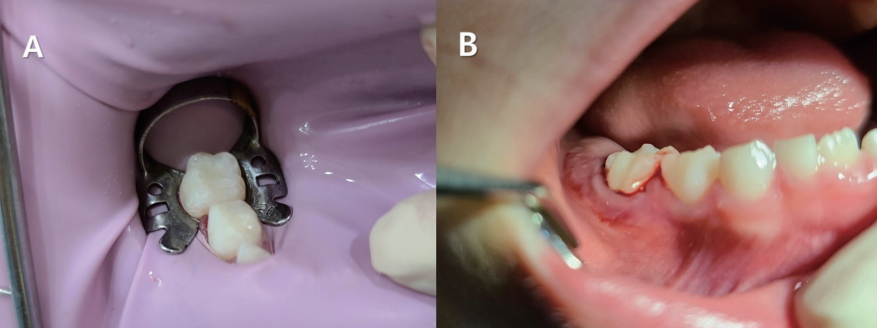
Fig 2.
Intraoral photographs at the first examination. (A, B) Bruising of gingiva in the right maxillary area and the mandibular anterior area.
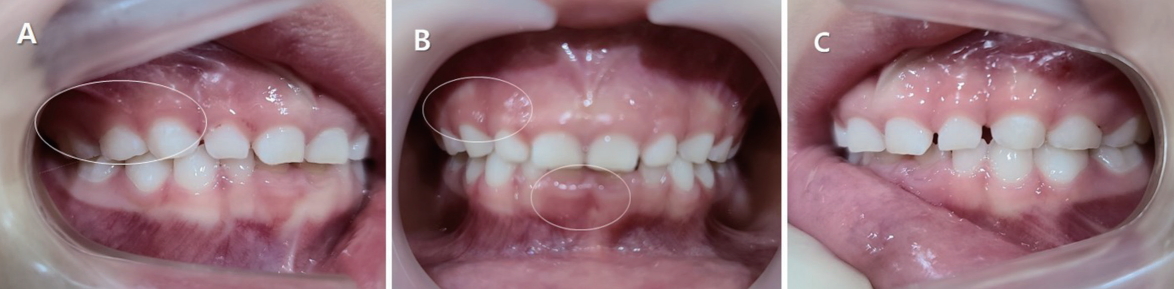
Fig 3.
Oral radiographs at the first examination. (A, C, D) Dental caries on the proximal surfaces of the deciduous molars.
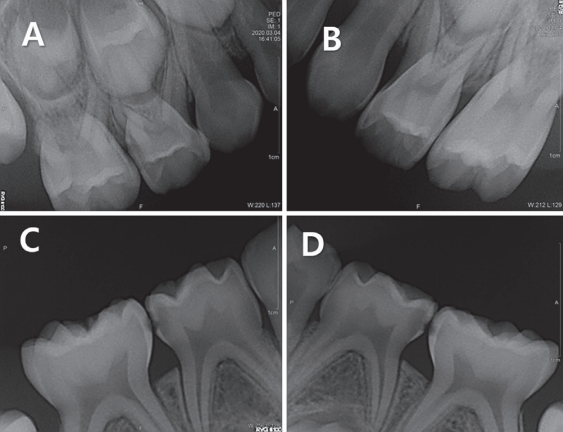
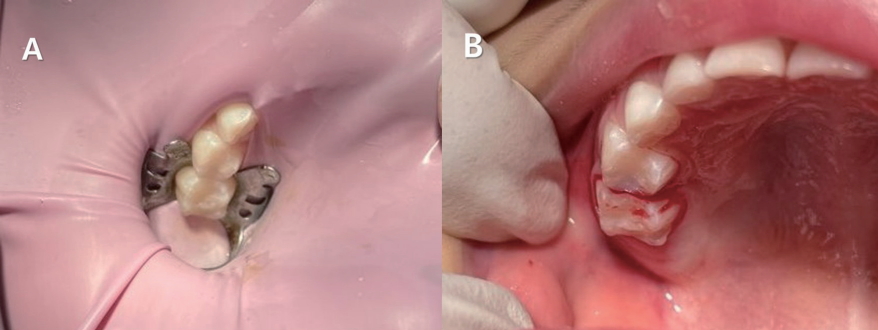
Fig 4.
Resin restorations of the left deciduous mandibular molars. (B) Gingival bleeding was seen after removal of the rubber dam.
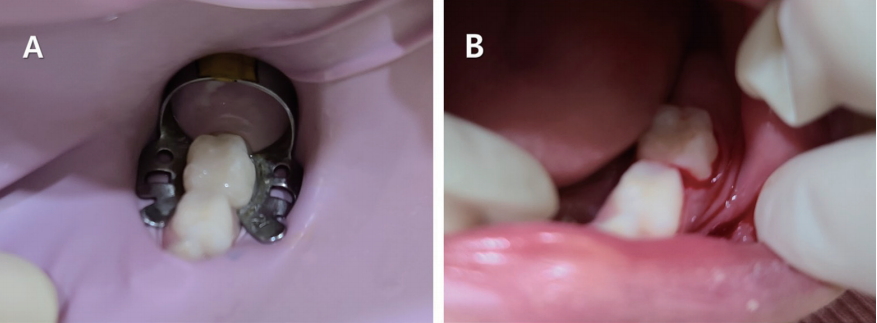
Fig 5.
Intraoral photographs at the second visit for treatment. Bruising of gingiva in the mandibular incisal and molar area.
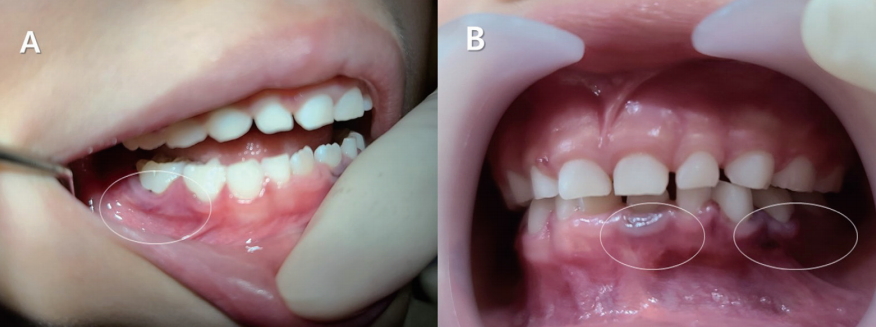
Fig 6.
Resin restorations of the right deciduous mandibular molars. (B) Gingival bleeding was seen after removal of the rubber dam.
References
1. Bellucci S, Caen J : Molecular basis of Glanzmannâs thrombasthenia and current strategics in treatment. Blood Rev, 16:193-202, 2002.


2. Caen JP, Castaldi PA, Bernard J, et al. : Congenital bleeding disorders with long bleeding time and normal platelet count. I. Glanzmannâs thrombasthenia : Report of 15 patients. Am J Med, 41:4-26, 1966.

3. Ranjith A, Nandakumar K : Glanzmann thrombasthenia: A rare hematological disorder with oral manifestations: A case report. J Contemp Dent Pract, 9:107-113, 2008.

4. George JN, Caen JP, Nurden AT : Glanzmann's thrombasthenia: The spectrum of clinical disease. Blood, 75:1383-1395, 1990.



5. Diana NM, Rupinder B : Dental considerations in the management of Glanzmannâs thrombasthenia. Int J Child Ped Dent, 3:51-56, 2010.

6. Brown DL : Congenital bleeding disorders. Curr Probl Pediatr Adolesc Health Care, 35:38-62, 2005.


7. Toygar HU, Guzeldemir E : Excessive gingival bleeding in two patients with Glanzmann thrombasthenia. J Periodontol, 78:1154-1158, 2007.


9. Bellucci S, Devergie A, Boiron M, et al. : Complete correction of Glanzmannâs thrombasthenia by allogeneic bone marrow transplantation. Br J Haematol, 59:635-641, 1985.


10. Doh YJ, Kim MH, Kim KY, et al. : A case of Glanzmann's thrombasthenia diagnosed with flow cytometry and SDSPAGE analysis of platelet membrane glycoprotein. Korean J Hematol, 27:443-451, 1992.
11. Park JB, Shin YS, Kim SH : Anesthetic experience for orthopedic surgery on a patient with Glanzmannâs thrombasthenia refractory to platelet transfusion-case report. Kor J Anesthesiol, 57:507-510, 2009.


12. Murphy MF, Waters AH : Immunological aspects of platelet transfusions. Br J Haematol, 60:409-414, 1985.


13. Seligsohn U, Rososhansky S : A Glanzmann's thrombasthenia cluster among Iraqi Jews in Israel. Thromb Haemost, 52:230-231, 1984.



14. Williams WJ, Beutler E, Ersler AJ : Disorders of hemostasis. Hematology. 2nd ed. McGraw-Hill, New York, 1368-1376, 1977.
- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 1,963 View
- 218 Download
- ORCID iDs
-
Miran Han

https://orcid.org/0000-0003-0312-6023Jongsoo Kim

https://orcid.org/0000-0001-8752-332X - Related articles
-
Oral Features in a Child with Noonan Syndrome : A Case Report2018 February;45(1)



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



