성장기 아동의 수완부 골 성숙도를 이용한 정중구개봉합 성숙도 평가
Assessment of Midpalatal Suture Maturation by Skeletal Maturity on Hand Wrist Radiographs
Article information
Abstract
이 연구의 목적은 7세부터 15세 사이 소아청소년을 대상으로 정중구개봉합의 성숙도와 SMI 및 MP3 방법으로 평가된 골 성숙도와의 연관성을 분석하고 수완부 골 성숙도와 중지의 중절골 성숙도가 정중구개봉합 성숙 단계를 예측할 수 있는 지표로 사용될 수 있는지 알아보기 위함이다. 이번 연구 대상은 무작위로 선택된 7세부터 15세 사이 남자 132명과 여자 135명으로 교정 치료 전 교정 진단을 위해 촬영 되었던 CBCT 수평면 영상 이용하여 정중구개봉합의 성숙도를 5단계로 평가하였고 수완부 방사선 사진을 이용하여 골 성숙도를 평가하였다.
정중구개봉합 성숙도와 SMI 방법으로 평가된 골 성숙도는0.905, MP3 방법으로 평가된 골 성숙도는 0.830으로 강한 상관관계를 보였다. 정중구개봉합 성숙도와 연령의 상관관계는 0.868으로 나타나 비교적 높은 상관관계를 보였다.
이번 후향적 연구를 통해 골 성숙도 평가를 위한 SMI와 MP3 방법은 정중구개봉합 성숙도를 예측할 수 있는 지표로 사용될 수 있음이 증명 되었으며 SMI 방법이 MP3 방법보다 더 나은 신뢰성을 보였다. 따라서 정중구개봉합 성숙도 평가가 필요한 모든 소아환자들을 대상으로 CBCT촬영하는 것은 불필요할 수 있으며 CBCT와 대체 가능한 SMI 와 MP3 방법은 최소의 방사선 피폭으로 간단하게 성장기 아동의 악정형 장치의 최적의 치료 시기 결정의 참고자료로 활용될 수 있을 것이다.
Trans Abstract
The aim of this retrospective study was to evaluate the correlation between the midpalatal suture maturation and skeletal maturation in growing children aged 7 - 15 years and predict the maturational stages of the midpalatal suture corresponding to skeletal maturity assessed by the skeletal maturation indicators (SMI) and middle phalanx of the third finger (MP3) stages.
The group of this retrospective study was consisted of randomly selected 132 male and 135 female in age from 7 - 15 years. The maturation of the midpalatal suture was evaluated by using images from cone-beam computed tomography (CBCT) while the skeletal age was assessed by hand-wrist radiography. CBCT images and hand-wrist radiographs used in this study were obtained from all subjects for orthodontic diagnosis before orthodontic treatment.
The maturational stages of the midpalatal suture showed strong correlations with both SMI and MP3 stages. The correlation between the midpalatal suture maturation and SMI (Spearman’s correlation coefficient, ϒS = 0.905, p < 0.05) was slightly greater than that of MP3 stages (ϒS = 0.830, p < 0.05). There was a positive significant correlation between the midpalatal suture maturation and chronological age (ϒS = 0.868,p < 0.05).
CBCT for evaluation of the midpalatal suture maturational stages may be unnecessary in every pediatric patients because SMI and MP3 stages were both replaceable useful methods for assessing maturation of the midpalatal suture before orthopedic treatment. In this retrospective study, the diagnostic reliability of the SMI method for estimating midpalatal suture maturation showed better reliability than the MP3 method.
Ⅰ. Introduction
Maxillary sutures that separate the middle of the palate and the maxilla from the palatine bone are the important growth sites of the maxilla where the maxillary growth is possible to be modified. Dentofacial orthopedic appliances can be effectively used in growing patients with skeletal imbalances in order to improve skeletal relationships by manipulation and control of maxillary growth[1]. The main concept of orthopedic treatment for maxillary discrepancies is to apply additional force to stimulate the separation of the midpalatal suture and the maxillary sutural system[2].
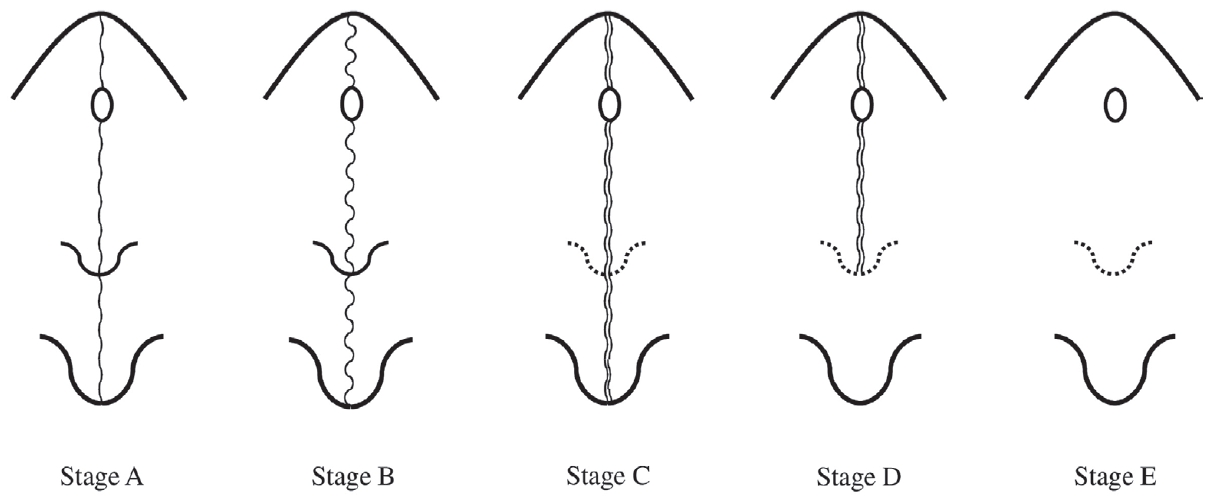
Angelieri et all .[3] classified the midpalatal suture maturation into five stages, stages A - E, by observing cone-beam computed tomography (CBCT) images. However, it is impossible to regularly obtain CBCT in all pediatric patients to evaluate the maturational stages of the midpalatal suture due to ethical concerns about unnecessary radiation exposure[4].
Recent studies have been conducted on relationships between the midpalatal suture maturation and skeletal development and reported that the maturation of the midpalatal suture is closely related to skeletal development[5-8]. These studies also have determined considerable variability in the chronologic age for ossification of the midpalatal suture[5,9]. However, there are the lack of previous investigations on utilizing skeletal maturity as a possible indicator to identify the maturational stages of the midpalatal suture.
Among several biologic methods to assess skeletal maturity, the skeletal maturation indicators (SMI) and the skeletal changes in the middle phalanx of the third finger (MP3) can be simply used by hand-wrist radiographs to evaluate skeletal maturity causing the least radiation risk[10].
The purpose of this study was to evaluate the correlation between the maturation of the midpalatal suture and the skeletal maturity assessed by SMI and MP3 stages in children aged 7 - 15 years and to analyze the diagnostic reliability of SMI and MP3 stages in predicting the maturational stages of the midpalatal suture.
Ⅱ. Materials and methods
This retrospective study was conducted at Ewha Womans University Mokdong Hospital and approved by the Institutional Review Board (IRB) of the hospital (IRB No.: 2020-05-009) prior to the research.
1. Study population
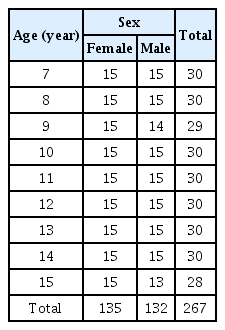
From January 2011 to December 2019, 267 pediatric patients aged 7 - 15 years who underwent CBCT and hand-wrist radiograph for orthodontic diagnosis prior to orthodontic treatment were randomly selected in this retrospective study. The total distributions for age and sex were shown in Table 1. Data were collected from each patient including CBCT images to evaluate the midpalatal suture and hand-wrist radiographs to assess the skeletal maturity. The exclusion criteria were specified as follows: congenital malformation affecting the assessment of the midpalatal suture morphology, history of previous orthodontic treatment, disease or medication affecting the bone metabolism, and congenital or acquired deformities to hand-wrist and third finger region.
All CBCT images were obtained with the following specifications: dose, 9 mAs; tube voltage, 80 kV; scanning time, 24 sec; and field of view, 20 × 15 cm. Hand-wrist radiographs were observed by using an imaging system (INFINITT Dental PACS; Infinitt, Seoul, Korea). All images were evaluated by one pediatric dentist and re-evaluated by the same examiner 2 weeks later in order to determine the intra-examiner reliability.
2. Study design
1) Evaluation of the midpalatal suture maturation
The CBCT cross-sectional images of the curved palate in the axial slices were analyzed from posterior to anterior regions of the midpalatal suture to evaluate the morphology of the midpalatal suture according to the classification scheme of Angelieri et all . (Fig. 1): stage A, a relatively straight high-density sutural line with no or little interdigitation; stage B, an irregular shape and a scalloped high-density line; stage C, 2 parallel, scalloped, high-density lines that are close to each other, separated by small low-density spaces; stage D, fusion of the suture occurred in the palatine bone; and stage E, fusion of the suture completed in the maxilla[3]. CBCT images of each maturational stage of the midpalatal suture are shown in Fig. 2.
3. Statistical analysis
The intraclass correlation coefficient was calculated for evaluation of the intra - examiner agreement. The Spearman’s correlation test was used to determine the correlations between the midpalatal sutures and the skeletal maturity assessed by SMI and MP3 stages. Positive likelihood ratios (LHRs) were calculated to establish the diagnostic reliability of each SMI and MP3 stage for the identification of each corresponding maturational stage of the midpalatal suture. The data were statistically analyzed by IBM SPSS Statistics software version 22.0 (SPSS Inc., IBM, Chicago, IL, USA).
Ⅲ. Results
The intraclass correlation coefficients for the evaluation of intra-examiner agreement for the maturational stage of the midpalatal suture and MP3 stage were 0.806 and 0.836, respectively. The reproducibility of SMI was evaluated with intraclass correlation coefficient as 0.993.
1.Correlation between the midpalatal suture maturation and SMI
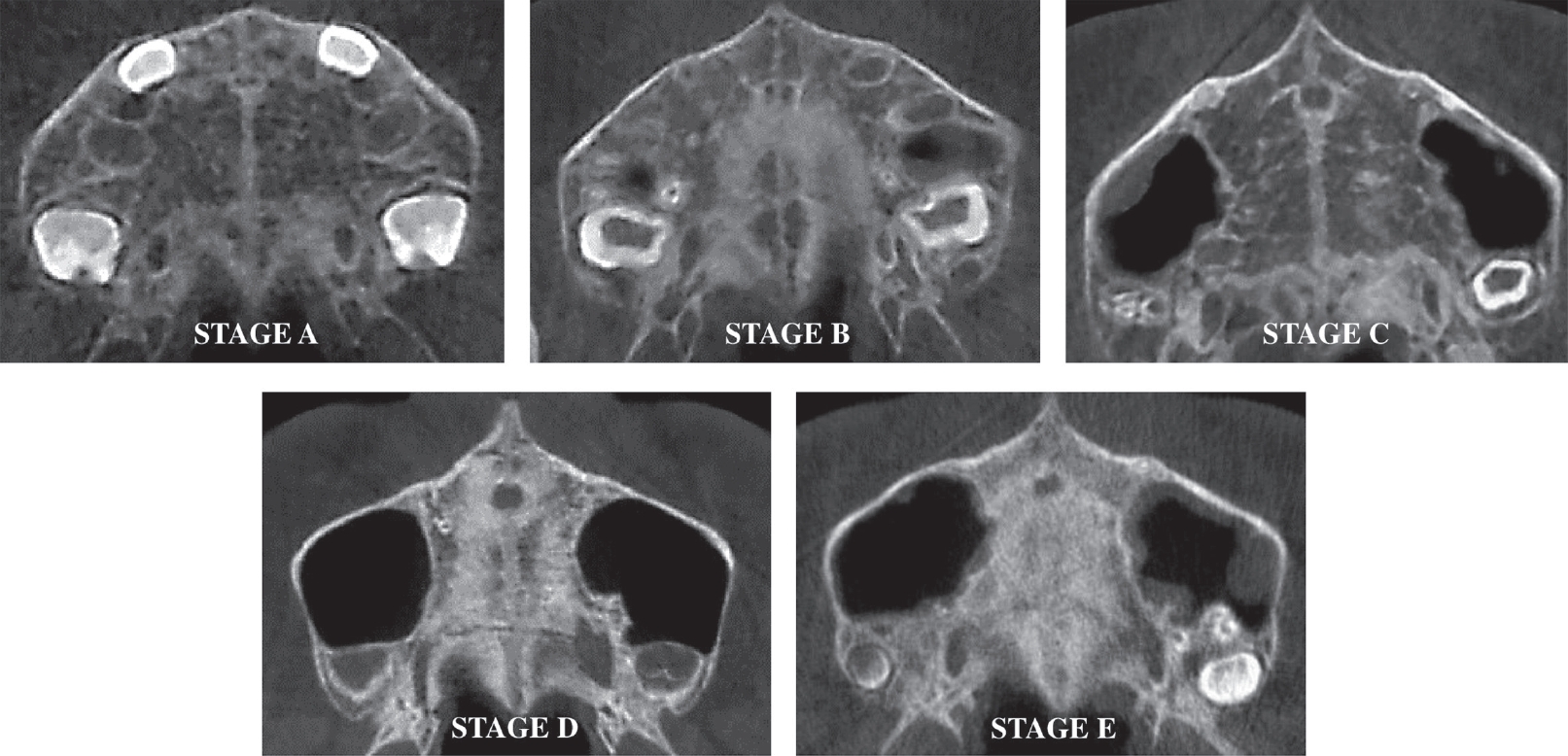
Detailed relative distributions of the different SMI according to the maturational stages of the midpalatal suture are presented in Table 2 and Figure 3. The degree of correlation between the maturational stages of the midpalatal suture and the SMI was investigated by using the Spearman rank correlation coefficient. The results showed there were statistically significant positive correlations (ϒs = 0.905, p < 0.05).

Distributions of maturation stages of the midpalatal suture by the skeletal maturation indicators (SMI).
The percentage of exact agreement of the SMI with the corresponding maturational stages of the midpalatal suture ranged between 53.8% (SMI 11/stage E) and 84.4% (SMI 1/stage A). The positive likelihood ratios of different SMI and the corresponding midpalatal suture maturation stages are summarized in Table 3.
Positive likelihood ratios for the skeletal maturation indicators (SMI) for the diagnosis of midpalatal suture stages
The positive LHRs ranged between 0.068 (SMI 1 - 2/stage C) and 7.264 (SMI 1 - 2/stage A). The values of positive LHRs of SMI 1 - 2, SMI 3, SMI 4 - 6, and SMI 10 - 11 were greater than 5 for the identification of stage A, B, C, and D/E in the midpalatal suture, respectively (Table 3). It indicates a reliable increase in the likelihood of estimating the maturational stages of the midpalatal suture.
2.Correlation between the midpalatal suture maturation and MP3 stages
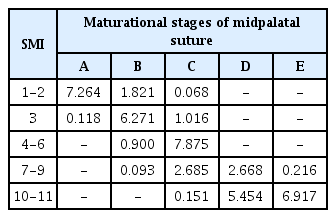
The relative distributions of the different MP3 stages according to the maturational stages of the midpalatal suture are reported in Table 4 and Figure 4. There were statistically significant positive correlations between the maturational stages of the midpalatal suture and the SMI (ϒs = 0.830, p < 0.05). The percentage of exact agreement of the MP3 stages with the corresponding maturational stages of the midpalatal suture ranged between 60.8% (MP3 I/stage D) and 70.3% (MP3 FG/stage C).

Distributions of the midpalatal suture stages according to the middle phalanx of the third finger (MP3) stages

Distributions of maturation stages of the midpalatal suture by the middle phalanx of the third finger (MP3) stages.
The positive LHRs of the different MP3 stages and the corresponding maturational stages of the midpalatal suture are given in Table 5. The positive LHRs ranged between 0.089 (MP3 H/stage B) and 6.917 (MP3 I/stage E). The values of positive LHRs of MP3 FG for the identification of stage C and of MP3 I for the identification of stages D and E in the midpalatal suture were greater than 5, indicating a reliable increase in the likelihood of determining the maturational stages of the midpalatal suture (Table 5).
3.Correlation between the midpalatal suture maturation and chronological age in male and female
The relative distributions of chronological age in male and female according to the maturational stages of the midpalatal suture are reported in Table 6 and Table 7. There were statistically significant positive correlations between the maturational stages of the midpalatal suture and chronological age in both sex (ϒs = 0.864 in male and ϒs = 0.892 in female, p < 0.05).
Ⅳ. Discussion
Maxillary discrepancy is one of the most common skeletal problems in orthopedic practice, which can mainly cause crossbite and dental crowding[13]. An adequate procedure for correction of skeletal imbalances is to manipulate and control growth of the maxilla. The effects of growth modification treatment to improve dentofacial discrepancy in the maxilla can be manifested when the orthopedic force for splitting the midpalatal suture exceeds the limits required for orthodontic tooth movement[14]. Also, the success or failure of the orthopedic treatment such as maxillary expansion and protraction relies on individual maturation levels of the midpalatal suture[15].
According to Melsen[9], as the maturation and the interdigitation of the midpalatal suture increase with increasing skeletal maturity, the effect of skeletal change is reduced whereas the effect of tooth movement is increased. In an adolescent reached to moderate levels of interdigitation of the midpalatal suture, it is possible to separate the suture with enough intraoral force across the palate with a jackscrew for expansion, but extraoral force from a facemask cannot exceed much force for protraction[16]. Therefore, it is very important to understand individual maturational state of the midpalatal suture in growing patients to achieve the maximum skeletal change at optimal treatment timing and to predict the skeletal outcomes[3,17].
This study investigated whether the hand-wrist methods were able to be used as diagnostic alternatives to predict the maturational stage of the midpalatal suture. The 3 - dimensional images from CBCT can provide the exact amount of ossification of the midpalatal suture without image overlapping of surrounding structures; therefore, it allows a reliable diagnosis of the maturational stage of the midpalatal suture[5]. However, it is impossible to regularly take CBCT with effective dose ranged between 19 and 368 μSv[18] from every pediatric patients due to ethical concerns about unnecessary radiation exposure[4,18]. Radiation exposure to pediatric patients who are more radiosensitive than adults can be reduced by using reliable indicators such as hand-wrist radiographs with effective dose 0.16 μSv[10] for predicting the midpalatal suture maturation instead of CBCT imaging.
The midpalatal suture maturation has been related with skeletal maturation as well as the transverse growth pattern of the maxilla[19]. Individual skeletal maturity has been assessed in previous studies by hand-wrist[11] and CVM methods[20] for evaluating the adolescent growth peak. Although CVM method has been commonly used, it has some limitations for estimating skeletal age; for example, certain landmarks such as C2 and C3 could not be detected with the use of a thyroid collar for protection of the thyroid gland from radiation[21] and the effect dose of a lateral cephalogram without a thyroid collar was higher than a hand-wrist radiograph as 5.03 μSv[10]. As a result, hand and wrist methods have been shown to be safer for growing children in terms of the least radiation exposure and presented more reproducibility and accuracy in predicting skeletal maturity[8,10].
In this study, skeletal maturity evaluated by SMI and MP3 methods showed strong correlations with the midpalatal suture maturation, indicating that the midpalatal suture maturation is highly related to skeletal development. These results were similar to the findings of Jang et all .[8] who verified strong correlations between the midpalatal suture maturation and skeletal age. Although SMI and MP3 methods both showed relatively high Spearman’s coefficients, SMI showed higher coefficient as 0.905 than MP3 method with coefficient 0.830. This illustrates that SMI method is more suitable for estimating maturational status of the midpalatal suture.
While several previous studies have been only investigated on correlation of the midpalatal suture maturation with skeletal maturity assessed by hand-wrist methods, this study conducted not only on their relationships but also the diagnostic reliability of the hand-wrist methods for determining the maturational stages of the midpalatal suture. Positive LHRs were calculated to verify the validity of SMI and MP3 stages for estimating the maturational stages of the midpalatal suture. The range of the LHR varied from 0 to infinity and its interpretation was intuitive: the bigger the LHR, the greater the probability of disease[22]. A result smaller than 1 indicated a decrease in the likelihood of disease while a result greater than 1 indicated an increase in the likelihood of disease[23]. In this study, a positive LHR of 5 or more for any SMI or MP3 stage is considered to be a reliable diagnostic indicator for the estimation of any maturational stages of the midpalatal suture.
Based on the results in this study, SMI 1 - 2, SMI 3, SMI 4 - 6, and SMI 10 -11 can be used for reliable identification of stages A, B, C, and D & E, respectively (Table 3) and MP3 FG stage and I stage can be used as valid indicator of stages C and D & E, respectively (Table 5). None of patients before SMI 6 and MP3 FG was presented in stage D or E, resulting similar to a prior study[8]. From a clinical point of view, these results are favorable since a patient before SMI 6 and MP3 FG should show a decent response to orthopedic treatment by modifying growth with more skeletal effect. In these instances, CBCT was unnecessary until SMI 6 and MP3 FG stage because these stages were correspondent to the midpalatal maturational stage C where the fusion of the midpalatal suture has not yet occurred.
On the other hand, patients at SMI 7 - 9 and MP3 G or H stage mostly distributed in stages C and D might need CBCT for evaluation of the midpalatal suture before making a decision for optimal treatment plan because initiated fusion of the midpalatal suture may hamper efforts to control sutural movement and reattachment[9]. For patients at SMI 10 - 11 and MP3 I stage corresponding to stages D and E, surgically assisted or miniscrew-assisted palatal expansion may be a better choice to obtain effective skeletal expansion without side effects such as dental tipping, gingival recession, palatal tissue necrosis, and fenestration of buccal cortical bone[24,25].
In a previous research, it was proposed that less resistant forces and favorable skeletal changes can be obtained by growth modification treatment at stages A and B[3]. Similarly, based on the results from this study, the prepubertal phases of skeletal maturation (SMI 1 - 2 and 3) can reliably correspond to the maturational stages A and B of the midpalatal suture. Thus, these results are able to support the findings of Baccetti et all .[26] that the most favorable skeletal changes can be achieved when dentofacial orthopedics is initiated prior to the pubertal growth spurt.
Although some previous histologic studies have indicated that there was large variability in chronologic age for ossification of the midpalatal suture[9,19,27], chronologic age showed relatively high correlation with the midpalatal suture maturation in this study; correlation coefficients were 0.864 in male and 0.892 in female (Table 6 and 7). These results correspond to the findings of Algelieri et all .[6], who stated that chronologic age was equally effective as skeletal maturity and able to be used as a viable alternative to evaluate the maturational stages of the midpalatal suture especially on the early stages when skeletal maturity is impossible to be assessed.
This study had a limitation related to the lack of interpretation on SMI 7 - 9 stages whether corresponding to the midpalatal suture stage C or D. Most of the patients in SMI 7 - 9 were distributed at stages C and D where are the critical border line to make a treatment decision whether try conventional orthopedic treatments. Therefore, further studies complementing this limitation would be encouraged to analyze the maturational stages of the midpalatal suture of growing patients in SMI 7 - 9 by using other maturity indicators found in hand and wrists.
Although the hand - wrist radiograph is the most common method to evaluate the skeletal development due to its objective and simple interpretation, high reproducibility, and minimal radiation exposure, it is not yet described as an absolute “gold standard” for the skeletal maturity[28]. As a result, if more studies on prediction of midpalatal suture maturation with various other methods to assess the skeletal maturity will be proceeded, the midpalatal suture maturation can be more accurately determined.
Ⅴ. Conclusions
In this study, the diagnostic reliability of skeletal maturity on hand-wrist radiographs for the evaluation of the midpalatal suture maturation was evaluated. SMI and MP3 methods both show overall satisfactory diagnostic agreements with the classification of the midpalatal suture maturation. The diagnostic reliability of the SMI method for predicting the midpalatal suture maturity shows better reliability than that of the MP3 method. Prepubertal SMI stages (SMI 1 - 2 and 3) can be utilized as reliable indicators for the midpalatal suture stage A and B. SMI 4 - 6 and SMI 10 - 11 reliably correspond to the midpalatal maturational stage C and stage D & E, respectively. It is necessary to take CBCT for patients in SMI 7 - 9 to evaluate the midpalatal suture more thoroughly before the clinical decision.