소아 및 청소년의 영구치 치관 파절시 파절편 재부착술의 추적 관찰
Long-Term Outcome of Reattached Tooth Fragment in Permanent Anterior Teeth of Children and Adolescents
Article information
Abstract
이 연구의 목적은 소아 및 청소년의 영구치 치관 파절시 파절편 재부착술의 추적 관찰 결과를 평가하고자 함에 있다. 21명의 27개의 영구치 파절편 재부착술을 시행한 환자를 대상으로 임상 사진, 방사선 사진 및 의무기록을 활용하여 평가하였다. 파절편 탈락은 총 17개 치아에서 관찰되었으며 반복적인 외상이 가장 빈번한 실패 원인이었다. 파절편 재부착술과 치수치료 시행 유무는 통계적으로 유의미하지 않았다(p > 0.05). 평균 파절편 비율은 0.482 ± 0.147이며 성공률은 파절편 비율과 유의미한 상관관계를 나타냈다(p = 0.018). 평균 파절편 유지 기간은 72개월이며 파절편 유지 기간과 파절편의 비율은 통계적으로 유의미한 상관관계를 나타냈다(p = 0.003). 소아 및 청소년의 영구치 치관 파절시 파절편 비율이 50% 미만인 환자에서 파절편 재부착술은 예측 가능한 치료 방법이 될 수 있다고 판단된다.
Trans Abstract
This study aimed to evaluate the long-term outcomes of teeth treated with reattachment technique in children and adolescents. Twenty seven permanent anterior teeth from 21 patients treated with fragment reattachment were evaluated. Clinical photos and medical records were used to assess treatment outcomes. Effect of pulp treatment and the ratio of fragment on success rate were statistically analyzed. Detachment of fragment was observed in 17 teeth, and their duration of retention was 21.41 ± 23.39 months. Repeated trauma was found to be the most frequent causes of failure. Pulp treatment before reattachment did not affect the success rate (p > 0.05). The mean ratio of fragment was 0.482 ± 0.147, and the success rate was affected by the ratio of fragment (p = 0.018). The median retention time of the teeth was 72 months if the ratio was under 0.5, and 8 months for that of the others. A significant correlation was found between the ratio of fragment and retention time (p = 0.003). Reattachment can be a predictable treatment option for crown fracture in anterior teeth in children and adolescents when a fracture involves less than 50% of the clinical crown.
Ⅰ. Introduction
Traumatic dental injuries (TDIs) occur frequently in children and adolescents[1,2]. Among TDIs in the permanent dentition, the crown fracture is the most common type of tooth injury and the maxillary central incisors are the most commonly involved teeth[1,2]. Further, crown fracture can cause the loss of tooth structure and damage pulpal health. As the maxillary anterior teeth have a large esthetic role, this type of injury can negatively affect self-image and quality of life in children and adolescents[3-5].
Reattachment is a restorative technique that puts fractured tooth fragments together using resin-based composites[6,7]. This technique enables quick, conservative, and predictable reproduction of the shape and function of the natural tooth[6-8]. The wear rates of reattached fragments are similar to those of adjacent teeth, whereas composite restorations wear off more rapidly[9]. This reattachment technique is expected to be a reliable treatment option for fractured anterior teeth.
Most clinical studies on reattachment of fractured tooth fragments were case reports describing the advantages of this technique[10-13]. Several studies suggested various techniques increasing the bonding strength of reattachment, such as the additional preparation prior to reattachment and dental post[14,15]. Although the advantages of this technique have been proven widely, long-term data on the survival of teeth treated with this technique remain insufficient.
The purpose of this study was to evaluate the long-term outcomes of teeth treated with reattachment technique in children and adolescents.
Ⅱ. Materials and methods
This study proposal was reviewed and approved by The Ethics Committee of Kyung Hee Dental Hospital, Kyung Hee University, Seoul, Korea (KH-DT19024). Data from all patients who visited the Department of Pediatric Dentistry, School of Dentistry, Kyung Hee University, Seoul, Korea for the treatment of crown fractures between 2006 and 2013 were evaluated.
Only patients who were treated with the reattachment technique in their permanent anterior teeth by 5 experienced pediatric dentists were included in the present study. The fragments were reattached to fractured teeth without additional preparation. After the reattachment, the patients were followed-up every 3 months. The patients whose follow up period was shorter than 2 years were excluded. To this end, from a total of 302 patients who visited our department for the treatment of crown fractures during the study period, 27 teeth were selected for the study.
The included cases were retrospectively evaluated using clinical photographs and medical records. A successful treatment was defined as fragment retention and failure was defined as fragment detachment from the affected tooth during the follow-up period. Time from the reattachment to detachment was regarded as the duration of retention.
To determine the ratio of fragment to clinical crown, clinical photographs of the cases were imported into Adobe Photoshop CC 2017 (version 18.0.0; San Jose, CA, USA). Using the software, the pre- and post-treatment photographs were superimposed for each case, and the ratio of fragment to clinical crown was calculated (Fig. 1). Following this, the teeth were allocated into 2 groups based on the ratio of fragment to clinical crown; group I was composed of teeth with ratio under 0.5 and group II consisted of teeth with ratio over 0.5.
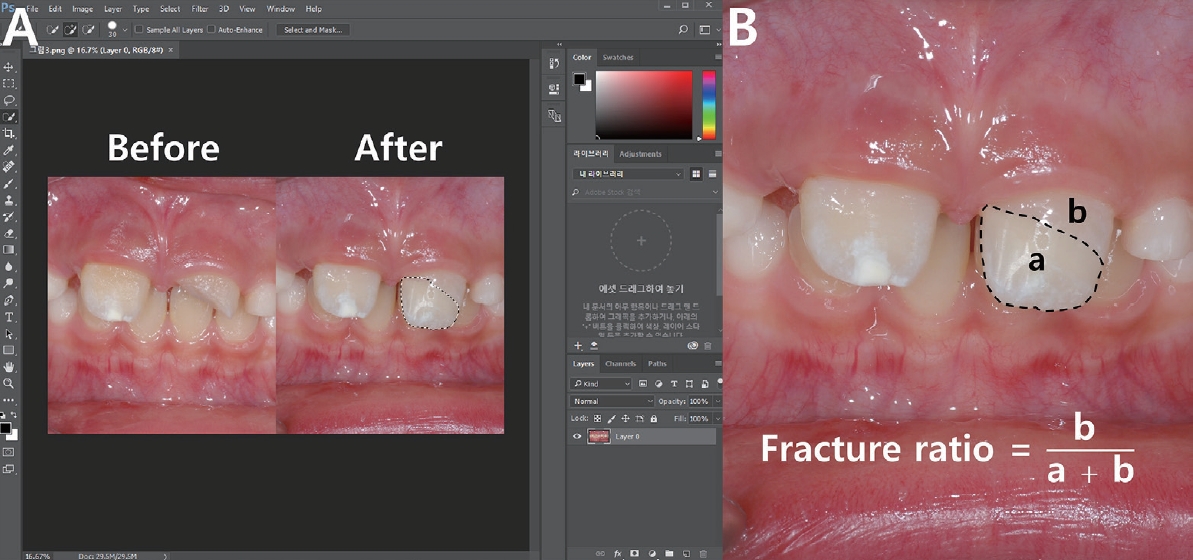
Ratio of fragment to clinical crown calculation. (A) Pre- and post-treatment clinical photographs were imported to Photoshop CC software and superimposed. (B) The ratio of fragment to clinical crown was defined as surface area of fragment divided by whole tooth surface area.
The duration was evaluated according to the pulp treatment and the ratio of fragment to clinical crown. Pulp treatments included direct pulp capping, partial pulpotomy, and root canal treatment.
Statistical analyses were performed using SPSS software (version 26.0 for Windows; IBM Corp., Armonk, NY, USA). The relationship between success rates and pulp treatment and the ratio of fragment to clinical crown were analyzed using Fisher’s exact test. Long-term survival was evaluated using the Kaplan-Meier product-limit estimator in SPSS and compared with the Log-rank test.
Ⅲ. Results
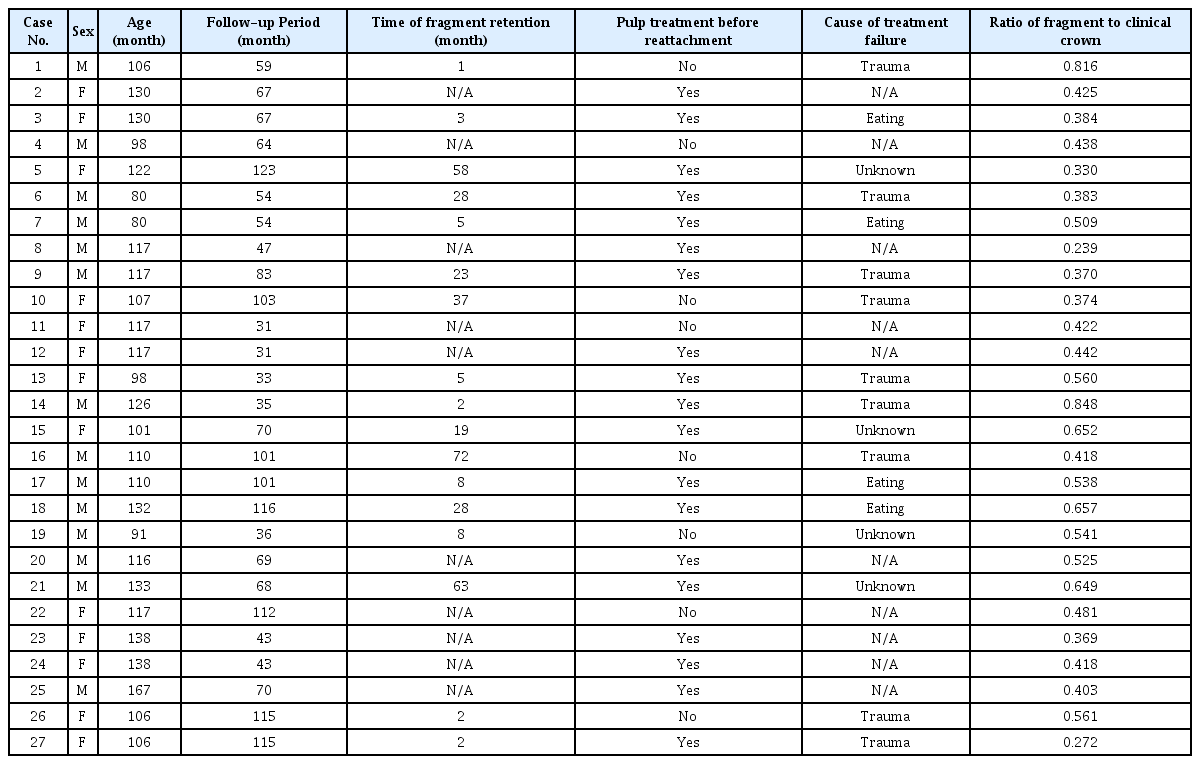
The mean age of the patients was 115.19 ± 18.78 months and the age ranged from 80 to 138 months. There were 12 male patients with 14 teeth and 9 female patients with 13 teeth. The male to female ratio of teeth treated with the reattachment technique was 1.08. All the injured teeth were maxillary central incisors. One tooth was involved in 15 patients and 2 teeth were involved in 6 patients (Table 1).
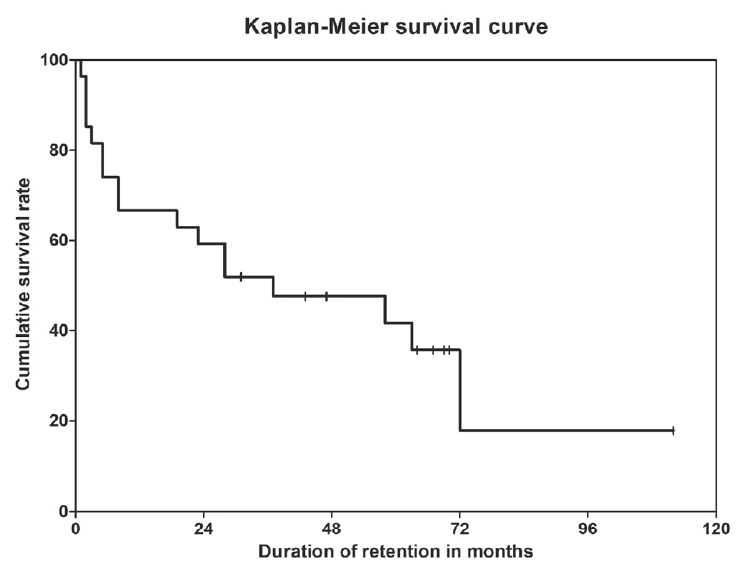
Follow-up period ranged from 31 to 123 months, the mean follow-up period was 70.74 ± 29.98 months. Treatment failure was observed in 17 teeth, and their duration of retention was 21.41 ± 23.39 months. After Kaplan-Meier survival analysis, the estimated mean retention time was 46.55 months, and the median time was 37 months (Fig. 2). Repeated trauma followed by unknown reasons and eating-related causes was the most frequent causes of failure (Table 2).
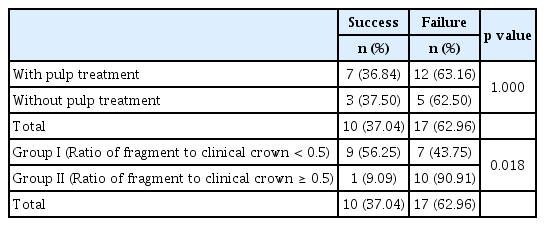
Of all the teeth we evaluated in this study, 19 teeth were treated after pulp treatment and fragments from 8 teeth were reattached without pulp treatment. During the follow-up period, 36.84% of the teeth with pulp treatment and 37.5% of the teeth without pulp treatment presented successful outcomes (Table 3). The success rate was not affected by pulp treatment (p > 0.05). Based on the Kaplan-Meier survival analysis, the estimated mean retention times of teeth with and without pulp treatments were 50.28 and 37.83 months, respectively (Fig. 3). The median retention time of teeth with and without pulp treatments were expected to be 37 months and 28 months, respectively. Similar to the statistical result from Fisher’s exact test, there was no difference between both survival curves (p > 0.05).

Kaplan-Meier survival curves of teeth with and without pulp treatments. The both curves were not significantly different (p = 0.639).
The number of teeth in group I was 16 and that in group II was 11. The mean ratio of the fragment to the clinical crown was 0.482 ± 0.147. The success rate of teeth in group I was 56.25%, the teeth in group II presented a 9.09% success rate. Contrary to the result with pulp treatments, the success rate was affected by the ratio of fragment to clinical crown (p = 0.018).
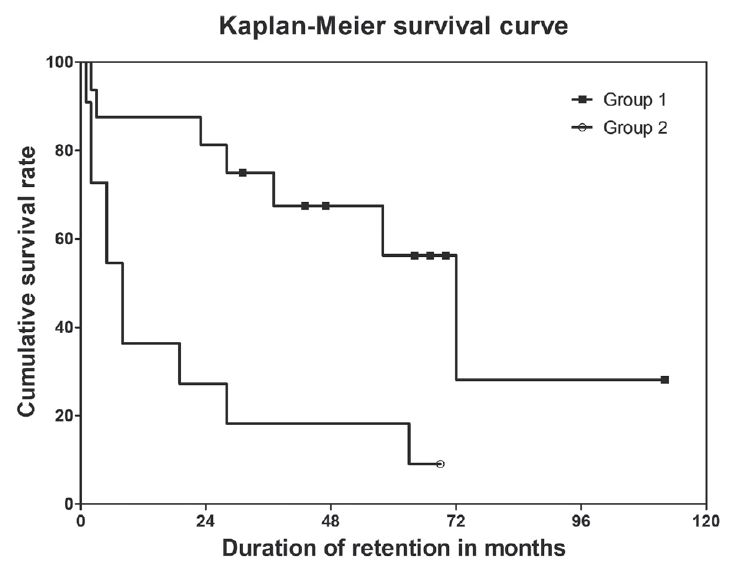
The mean retention time of group I was expected to be 64.55 months and that of group II was expected to be 19.09 months (Fig. 4). The expected median time of group I and group II was 72 months and 8 months, respectively. A significant correlation between the ratio of fragment to clinical crown and retention time was determined by the Log-rank test (p = 0.003).
Ⅳ. Discussion
Reattachment of fractured tooth fragments is a conservative technique that could restore the shape of fractured teeth predictably with easy and simple procedures. And, this technique has been supported by several clinical studies[6-8]. Despite its advantages, long-term survival data for teeth treated with reattachment of fractured tooth fragments were rare. In this study, the outcomes of tooth fragment reattachment from long-term follow-up data were evaluated.
In this study, 37.04% of reattached fragments were retained during the follow-up period, in comparison to previous studies where the success rates varied from 25% to 77.8%[16-18]. This difference in success rate among the studies might be attributed to different timing of assessing treatment success. In the current study, the tooth which retains its fragment stable until the last visit was regarded as a successful treatment case. Considering that follow-up periods were different for each patient and even in a single tooth, there was no certain point or time for determining treatment success. In other words, as there was no certain point to determine treatment success, this study could include not only the successfully treated cases but also the failed cases until their last follow-up visit. This made the present study more appropriate for outcome evaluation. Unlike previous studies which were conducted mainly with adult patients, reattachment in children and adolescent patients were evaluated in this study. This could also be attributed as a reason for the different success rates compared to that of previous studies.
In a clinical study of fractured anterior tooth restorations with composite resin, the 24-month survival rate was 82.14%[19]. Difference in defining the treatment success could account for varied success rate among the studies. In this study, the treatment was regarded as successful case only if the fragment was intact at the last visit of follow-up. While previous study was conducted mainly with adult patients, children and adolescents were recruited for this study. And this could affect the success rate of treatment.
In a previous study, it was reported that 49% of patients with TDIs experience repeated dental trauma[20]. In this study, more than half of treatment failures were caused by repetitive trauma. This finding indicates that dentists should be aware of repetitive TDIs, and traumatized children and their guardians should be counseled to be careful about the possible repetitive dental injuries. The use of a mouth guard is recommended to prevent the teeth and surrounding tissues from incurring additional injuries[21].
Based on the findings of this study, the pulp treatment was not the factor that deteriorated the stability of reattached fragments. As the tooth fragments of this study were reattached by a conventional bonding technique whose strength depended primarily on the micromechanical locking between composite resin tag and etched enamel as well as on the hybrid layer above the dentinal tubules, it was reasonable that the success rate was not affected by pulp treatments[22]. It can be considered that the reattachment of fragments may be utilized for treatment not only of uncomplicated crown fractures but also of complicated cases.
Concerning the ratio of fragment to clinical crown, the success rate was demonstrated to be higher in group I than in group II. Kaplan-Meier curves indicated that only 27.27% of reattached fragments in group II were expected to survive after 24 months of follow-up, about 81.25% of fragments in group I were expected to survive. This finding indicated that the reattachment of tooth fragments cannot provide long-term clinical success when fractures involve more than 50% of the crown surface area. This could be demonstrated by the Class II lever principle (Fig. 5). Supposing 3 imaginary points consisting of a class II lever on the axis of a tooth with a fixed length, it can be assumed that the longer the reattached fragment, the bigger force would be applied onto the fracture line. A tooth with a bigger ratio of fragment to clinical crown could be at an even bigger risk of detachment than a tooth with a smaller ratio when subjected to the same external forces.
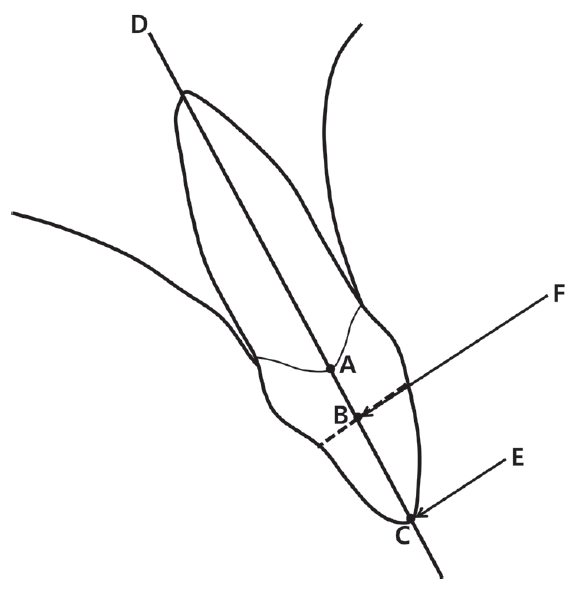
A diagram describing forces causing detachment by class II lever principle. (A) A point on the junction of clinical crown and the rest of tooth serving as a fulcrum. A mobility of tooth can be restricted by root embedded in the alveolar socket. (B) A point on the fracture line (black dotted line) serving as a resistance. (C) A point where the external force is exerted. (D) An axis of tooth. (E) The input external force such as repetitive trauma. (F) The output force applied to fracture line.
In cases with a fragment that is larger than 50% of the clinical crown, dentists should improve their reattachment procedure by observing the recommended bonding technique. It is advised to follow additional techniques recommended by previous studies such as preparation of dentin grooves, overcontouring technique, chamfering, and beveling to improve treatment outcomes[7,9,23,24].
This study has several limitations. First, individual causal parameters, such as occlusal interferences, daily eating patterns, oral habits, state of fragments and patient cooperation which could contribute to the failure of reattachment were not considered. As they are possible factors that could deteriorate treatment outcomes after a dental trauma, further studies including them are required. Second, considering the age of patients from our study, some teeth could be in a partially erupted state. The ratio of fragment to clinical crown can be changed during the follow-up period due to eruption. In this study, eruption stages of teeth were not considered to simplify superimposition and calculation procedures. A study including the eruption stages of traumatized teeth should be conducted in the future. Third, as this study was conducted with medical record of patients who were treated with 5 experienced pediatric dentists, it should be considered that inter clinician variability in clinical experiences and degrees could affect the survival rate of fragments.
Within the limits of this study, a reattachment technique can be a predictable treatment option for crown fracture in anterior teeth of children and adolescents only when a fracture involves less than 50% of the clinical crown. In cases presenting severe crown fracture, additional clinical techniques were required to improve the stability of the fragment. Patients and their guardians should be counseled to be careful about repetitive dental trauma.