 |
 |
| J Korean Acad Pediatr Dent > Volume 48(3); 2021 > Article |
|
초록
Molar-incisor malformation (MIM)은 치관은 정상이나 치근의 비정상적인 형태를 보이는 것이 특징적이다. 제1대구치에 가장 많이 발생하며, 제2유구치나 상악 중절치도 때때로 이환된다.
이 증례 보고에서는 제1대구치를 포함해, 제2유구치에 MIM이 나타난 환자의 증례를 보고하고, 치근이 건전하게 발거된 제2유구 치의 micro computed tomography (CT)를 이용한 형태학적 분석을 시행하였다. 발거된 치아에서는 MIM의 외형적 특징인 치관 - 치 근 이행부의 cervical constriction을 육안상으로 확인할 수 있었으며, micro CT 분석에서 백악법랑경계부의 광화된 부위 (Cervical Minelarized Diaphragm), 많은 부근관과 막힌 근관 등의 복잡한 근관 형태, 근관 내 석회화 물질, 영구치에 비해 상대적으로 협착된 치 관부 치수강이 관찰되었다.
Abstract
Molar-incisor malformation (MIM) is characterized by malformation in the root with a normal crown. While MIM mostly occurs in the permanent first molar, it has also been reported in the maxillary central incisor and the primary second molar (PSM), but anatomical analysis of the primary teeth with MIM has not been studied to date.
In this case report, a patient with MIM was reported, and an extracted PSM with MIM was analyzed with micro computed tomography (CT).
A cervical constriction morphology of the cementoenamel junction (CEJ) can be observed in extracted PSM. In micro CT analysis, characteristics such a mineralized plate (cervical mineralized diaphragm) in the CEJ area, complex root canal morphologies, a calcified mass inside the pulp chamber, and constricted pulp chamber of crown portion were observed.
Molar-incisor malformation (MIM), a recently reported dental anomaly, appears as an anomaly in the root with a normal crown; it is characterized by a complex anatomical root canal structure[1]. There are various types of dental anomalies caused by genetic and environmental factor that include changes in the components or structures of the enamel or dentin[2]. Characteristics of MIM differs from other dental anomalies that have been previously reported[3,4]. Dentin dysplasia type 1 is different from MIM as it is a genetic disease and occurs in all teeth. Regional odontodysplasia is a nonhereditary developmental defect, shows anomaly of both enamel and dentin formation. In 2014, Witt et al .[1] first reported on MIM using the term ‘root malformation associated with cervical mineralized diaphragm (RM-CMD)’. The term of ‘MIM’ can often be confused with ‘molar-incisor hypomineralization (MIH)’, so there are studies using the term ‘molar root-incisor malformation (MRIM)’[5,6]. While MIM mostly occurs in the permanent first molar (PFM), it has also been reported in the permanent maxillary central incisor and the primary second molar (PSM)[7].
Many factors have been proposed as causative factors of MIM. The hypothesis that history of severe medical conditions, such as premature birth, experience of magnetic resonance imaging (MRI) scan, infections within 2 - 3 years after birth may affect tooth development, is convincing[6,8]. In particular, MIM may be related to problems with the nervous system, such as encephalomeningitis[9]. But, it is unclear yet, because rare factors like gene mutation have been reported[10].
While many case reports and studies on extracted teeth with MIM have been reported[1,9,11,12], no morphological study involving primary teeth with intact root has been described to date.
The purpose of this study is to report the case of a patient who had MIM in the PSMs and PFMs and to analyze the micromorphological characteristics of the patient’s extracted PSM with MIM.
A boy aged 10 years and 8 months visited the Department of Pediatric Dentistry, Gangneung-Wonju National University Dental Hospital. At 1 year after birth, surgery for insertion of a vascular closure stent was conducted under general anesthesia due to bilateral arteriovenous malformation, and the patient had been undergoing follow-up MRIs for every 2 years. At the first visit, panoramic and periapical radiographs revealed MIM morphology in all PFMs and both mandibular PSMs, but no clinical symptoms were observed. Distal root of mandibular right PFM was resorbed by mesial eruption of permanent second molar with locking tendency. Due to distal eruption of the mandibular right second premolar, the mesial root of the mandibular right PSM was not resorbed (Fig. 1).
After informed consent was obtained, extraction of the mandibular right PSM was planned to improve the eruption path of the permanent second premolar. If locking of the second molar is not resolved, the plan was to proceed with uprighting the second molar later. For fixation of the anterior teeth, a lingual arch with an orthodontic band on the lower bilateral first premolar was used.
After extraction of the mandibular right PSM and fixation of lingual arch, continuous observation was conducted every 3 - 6 months. Check-up panoramic radiograph was taken at 3 months follow-up (Fig. 2), and lingual arch was removed at 15 months follow-up.
In panoramic radiographs taken 2 years later, it shows improvements in the eruption path of the mandibular right second premolar and the mandibular right second molar (Fig. 3). All of PFMs with MIM showed no symptoms and are being followed up continuously.
The mandibular right PSM was extracted without any damage to the remaining mesial root. A cervical constriction morphology of the cementoenamel junction (CEJ) and a mineralized plate with opacity distinguishable from enamel or dentin was observed with bare eyes between the crown and the root (Fig. 4).
3D micro focus computed tomography (CT; Sky-Scan 1172TMm, Skyscan, Kontich, Belgium) was used to analyze the tooth sample. Image reconstruction was conducted by image analysis software (DataViewerTM, Skyscan, Kontich, Belgium).
The results from the micro CT analysis are shown in the Fig. 5. A mineralized area, so called cervical mineralized diaphragm (CMD), was observed in the area of the crown - root transition (See the solid arrow in Fig. 5A-C). It showed radiopacity between that of enamel and dentin[1], and is known as one of the characteristics of MIM.
From the coronal plane, many accessory root canals connected to the root furcation area existed and irregular canals with obliteration were observed (See the circle in the Fig. 5E). Complex root canal morphology furcating at the apical area of the root was seen (See the circle in the Fig. 5F). Inside the root canal, a calcified mass with radiopacity similar to that of dentin was observed (See the dotted arrow in the Fig. 5A, 5D). The pulp chamber was narrowed downwards and the top was positioned near or below the CEJ (Fig. 5).
In this case study, the patient had a PSM with MIM and his extracted lower right PSM was analyzed by micro CT. Wright et al .[6] reported the relationship between MIM and health issues that had been detected or occurred during the neonatal period of life. Lee et al .[8] reported that MIM was related to systemic disease occurring at 1 to 2 years of age. The patient in this case had a history of surgery under general anesthesia with bilateral cerebrovascular disease arteriovenous malformation at 1 year of age, which may be the cause of MIM development.
Normal root development takes place with interactions between the Hertwig’s epithelial root sheath (HERS) and the dental papilla after the crown is completely developed[12]. Impaired interactions between the HERS and the dental papilla might be involved in the mechanism of MIM. In previous epidemiological studies, PFMs are always affected by MIM, and root malformations in PSMs account for 50% of MIM cases[13,14]. The reason for the occurrence of MIM in both of PFM and PSM is not clear. As there is a time gap between the completion of crown formation in the PFM (age of 2.5 to 3 years), and that in the PSM (age of 10 to 11 months), the period of root development in the PFM and PSM is different[15]. If MIM occurred in maxillary central incisor, shortening of the root with a large pulpal obstruction, cervical constriction and wedge-shaped defect of crown can be observed. In this case, normal maxillary central incisor was observed[6,8].
In this study, micro CT analysis showed a CMD, which looked like a mineralized plate around the CEJ. It showed radiopacity between that of enamel and dentin. CMD is a structure specific to MIM and has not been observed in other dental anomalies. Witt et al .[1] reported that although the Ca/P ratio did not differ significantly, due to densely calcified globules in CMD, increased radiopacity can be observed. CMD originates from the dental follicle, develops during the formation of crown, and may be a role of mechanical obstacle to normal root development.
Complex morphologies such as accessory root canals near the root furcation area, constricted root canals, and root canals furcated near the apical area of the mesial root were observed. These findings were similar with the findings of previous studies on PFMs affected by MIM. Brusevold et al .[9] observed numerous oddly formed roots and root canals, and canals do not connected to the pulp chamber when examined by micro CT reconstruction. Choi et al .[12] used micro CT, and observed highly irregular canal anatomies with some of the canals penetrating the pulpal floor. Due to these complex anatomies of the root canal, conventional endodontic treatment is difficult, and Yue and Kim[16] reported cases of successful root canal treatment of an MIM-affected PFM using cone beam CT.
In the root canal, a calcified mass with similar radiopacity to that of dentin was observed. This is not common characteristics of MIM, but some cases with this morphology have been reported previously. Lee et al .[17] observed osteoid-like hard tissue, which showed a porous structure, and Lee et al .[18] reported generalized pulp stones in patient with MIM.
The volume of the pulp chamber in the crown was severely constricted and was smaller than the chamber size in the analysis of previous studies of MIM-affected PFMs. In studies of the PFM, the coronal pulp chamber was relatively normal[1,9,13]. It is thought that constricted pulp chamber of crown portion is more prominent due to the calcification associated with physiologic root resorption of primary teeth[19]. This is considered to be the biggest difference from the results of previous studies of the PFM with MIM. Due to this characteristics, root canal treatment of primary molars may present more difficulties - such as perforation occurring during the access opening stage - than of PFMs with MIM.
Due to root resorption caused by the eruption of successive permanent teeth, it is very difficult to obtain an intact root of an extracted primary molar with MIM. An observation worth noting in this case report was that when the patient first visited the hospital, the mesial root of his mandibular right PSM had not been resorbed, due to distal eruption of the mandibular right second premolar (a rare situation). PSM was extracted without any damage of mesial root, and micro CT analysis could be conducted for the first time.
Pulp necrosis with apical abscess of teeth with MIM is commonly observed, and extraction is used as a treatment option in many cases[20]. If MIM appears only in the PFM and the extraction of affected teeth is absolutely necessary, orthodontic treatment for space closure or implant prosthesis can be used[21]. However, the PSM is a crucial tooth compared to other teeth during the primary dentition period. If it is lost before the eruption of the PFM, it has a negative effect on maintaining the space, complicating the treatment plan, and jeopardizing the correct position of the permanent dentition[22].
In general, the PSM affected by MIM has a complex root canal structure, which causes difficulty with root canal treatment and a poor prognosis, leading to early loss of the PSM. For pediatric patients with MIM in the PSM, the first consideration is to prevent the need for root canal treatment, by conducting more thorough clinical and radiological observations than in patients with normal teeth. Second, when root canal treatment is inevitable, CBCT can be useful for better outcomes.
This study had a limitation, namely that it examined a single tooth in a single case. Since calcification associated with physiologic root resorption of primary molar may have affected the smaller pulp chamber of crown portion, it is not clear whether a constricted pulp chamber is a characteristics of primary molar with MIM. The results of this study serve as a foundation for various future studies on PSMs with MIM. It is necessary to conduct a variety of studies in the future based on the results of the present study to provide the most appropriate care for MIM patients.
This is the first case report that presented the results of anatomical analysis of the PSM with MIM using micro CT. A cervical constriction morphology of the CEJ and a mineralized plate were observed with bare eyes. In micro CT analysis, its characteristics such as CMD, complex canal morphologies, calcified mass were similar to those in PFMs with MIM, but pulp chamber of crown portion is more constricted than that of PFMs. It is important to carefully examine and manage MIM, especially among patients with MIM in the PSM.
Fig 1.
Radiographs at first visit (age of 10 years and 8 months). (A) Panoramic radiograph. All 4 permanent first molars and both lower primary second molars showed MIM. (B - E) Periapical radiographs. Distal root of mandibular right permanent first molar was resorbed by mesial eruption of permanent second molar with locking tendency. The mesial root of the mandibular right primary second molar was not resorbed due to distal eruption of the mandibular right second premolar.
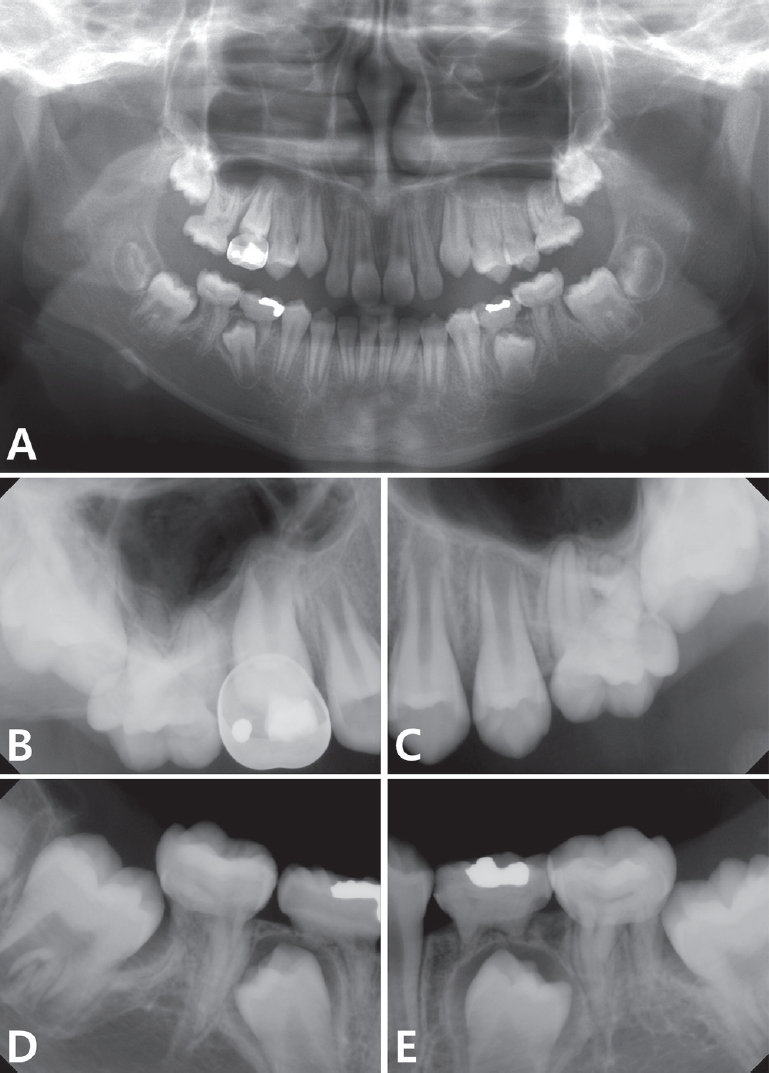
Fig 2.
Panoramic radiograph at 3 months follow up (age of 10 years and 11 months). After extraction of mandibular right primary second molar and fixation of lingual arch, continuous observation was conducted.
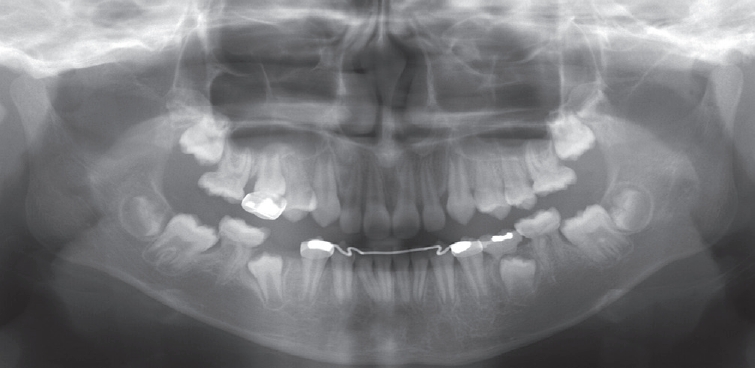
Fig 3.
Panoramic radiograph at 2 years follow up (age of 12 years and 8 months). The eruption path of the mandibular right second premolar and the mandibular right second molar was improved.
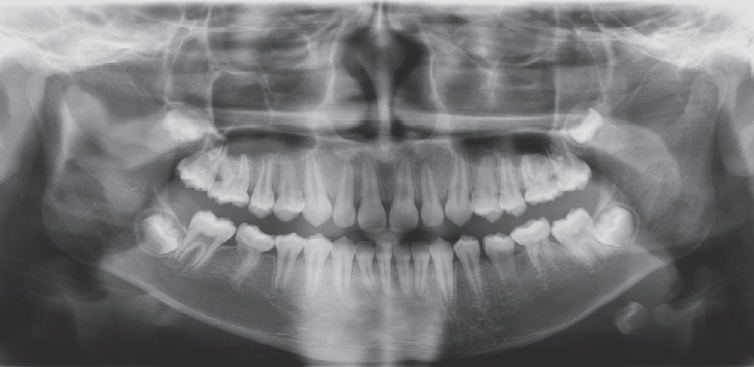
Fig 5.
Micro computed tomography analysis of the extracted primary second molar. The solid arrows indicate mineralized plate around cementoenamel junction. The dotted arrows indicate calcified mass in root canal. The circles indicate complex morphologies of root canal. (A) Mineralized plate around the cementoenamel junction and calcified mass in root canal (coronal plane view). (B) Mineralized plate around cementoenamel junction (horizontal plane view). (C) Mineralized plate around cementoenamel junction (sagittal plane view). (D) Calcified mass in the root canal (sagittal plane view). (E) Many accessory canals connected to furcation of roots (coronal plane view). (F) Complex root canal morphology furcating at the apical area of the root (sagittal plane view).

References
1. Witt CVA, Hirt T, Rutz G, Luder HU : Root malformation associated with a cervical mineralized diaphragm - a distinct form of tooth abnormality? Oral Surg Oral Med Oral Pathol Oral Radiol, 117:311-319, 2014.

2. Brook AH : Multilevel complex interactions between genetic, epigenetic and environmental factors in the aetiology of anomalies of dental development. Arch Oral Boil, 54:3-17, 2009.

3. Seow WK, Shusterman S : Spectrum of dentin dysplasia in a family: case report and literature review. Pediatr Dent, 16:437-442, 1994.

4. Spini TH, Sargenti NS, Loyola AM, et al. : Progressive dental development in regional odontodysplasia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 104:40-45, 2007.

5. Fagrell T : Molar incisor hypomineralization: morphological and chemical aspects, onset and possible etiological factors. Swed Dent J Suppl, 5:11-83, 2011.
6. Wright JT, Curran A, Kim JW, et al. : Molar root-incisor malformation: considerations of diverse developmental and etiologic factors. Oral Surg Oral Med Oral Pathol Oral Radiol, 121:164-172, 2016.


7. Kim JE, Hong JK, Huh KH, et al. : Clinico-radiologic features of molar-incisor malformation in a case series of 38 patients: A retrospective observational study. Medicine, 98:17356, 2019.
8. Lee HS, Kim SH, Song JS, et al. : A new type of dental anomaly: molar-incisor malformation (MIM). Oral Surg Oral Med Oral Pathol Oral Radiol, 118:101-109, 2014.


9. Brusevold IJ, Bie TMG, Espelid I, et al. : Molar incisor malformation in six cases: description and diagnostic protocol. Oral Surg Oral Med Oral Pathol Oral Radiol, 124:52-61, 2017.


10. Zschocke J, Schossig A, Kapferer-Seebacher I, et al. : Variable expressivity of TCTEX1D2 mutations and a possible pathogenic link of molar-incisor malformation to ciliary dysfunction. Archoral Biol, 80:222-228, 2017.

11. Kim MJ, Song JS, Hyun HG, et al. : Clinical considerations for dental management of children with molar-root incisor malformations. J Clin Pediatr Dent, 44:55-59, 2020.


12. Choi SJ, Lee JW, Song JH : Molar-incisor malformation: three cases of a newly identified dental anomaly. J Korean Acad Pediatric Dent, 44:370-377, 2017.

13. Lee EK, Kim YJ, Kim HJ, Nam SH : Aberrant root morphology in the permanent first molars. J Korean Acad Pediatric Dent, 42:172-179, 2015.
14. Huang XF, Chai Y : Molecular regulatory mechanism of tooth root development. Int J Oral Sci, 4:177-181, 2012.



15. Arthur JN, John RC, Martha HW, et al. : Pediatric dentistry. 6th ed. Elsevier, 194-197, 2018.
16. Yue W, Kim E : Nonsurgical endodontic management of a molar-incisor malformation-affected mandibular first molar: a case report. J Endod. 42:664-668, 2016.


17. Lee HS, Kim SH, Song JS, et al. : Microscopic analysis of molar-incisor malformation. Oral Surg Oral Med Oral Pathol Oral Radiol, 119:544-552, 2015.


18. Lee D, Shin J : Generalized Pulp Stones of Primary Dentition in a Patient with Molar-Incisor Malformation: A Case Report. J Korean Acad Pediatr Dent, 47:337-343, 2020.

19. Arys A, Philippart C, Dourov N : Microradiography and light microscopy of mineralization in the pulp of undemineralized human primary molars. J Oral Pathol Med, 22:49-53, 1993.


20. Pavlic A, Vrecl M, Nemec A, et al. : Case report of a molarroot incisor malformation in a patient with an autoimmune lymphoproliferative syndrome. BMC Oral Health, 19:49, 2019.







 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print




