1. Khandelwal S, Patil S : Oral mucoceles - review of the literature.
Minerva Stomatol, 61:91-99, 2012.

2. Hayashida AM, Zerbinatti DC, Almeida JD,
et al. : Mucus extravasation and retention phenomena: a 24-year study.
BMC Oral Health, 10:1-4, 2010.



3. Chi AC, Lambert PR, Neville BW,
et al. : Oral mucoceles: a clinicopathologic review of 1,824 cases, including unusual variants.
J Oral Maxillofac Surg, 69:1086-1093, 2011.


4. Re Cecconi D, Achilli A, Carrassi A, et al. : Mucoceles of the oral cavity: a large case series (1994-2008) and a literature review. Med Oral Patol Oral Cir Bucal, 15:551-556, 2010.
5. Harrison JD : Salivary mucoceles.
Oral Surg Oral Med Oral Pathol, 39:268-278, 1975.


6. Oliveira DT, Consolaro A, Freitas FJ : Histopathological spectrum of 112 cases of mucocele.
Braz Dent J, 4:29-36, 1993.

7. Rao PK, Hegde D, Shenai P, et al. : Oral mucocele-diagnosis and management. J Dent Med Med Sci, 2:26-30, 2012.
8. Baurmash HD : Mucoceles and ranulas.
J Oral Maxillofac Surg, 61:369-378, 2003.


9. Morton RP, Bartley JR : Simple sublingual ranulas: pathogenesis and management.
J Otolaryngol, 24:253-254, 1995.

10. Itro A, Cassaro E, Marra G : Nonsurgical treatment of a sublingual ranula in a ten-month-old baby.
J Clin Pediatr Dent, 24:31-33, 1999.

11. Roh JL, Kim HS : Primary treatment of pediatric plunging ranula with nonsurgical sclerotherapy using OK-432 (Picibanil
®).
Int J Pediatr Otorhinolaryngol, 72:1405-1410, 2008.


12. Delbem ACB, Cunha RF, Ribeiro LLG,
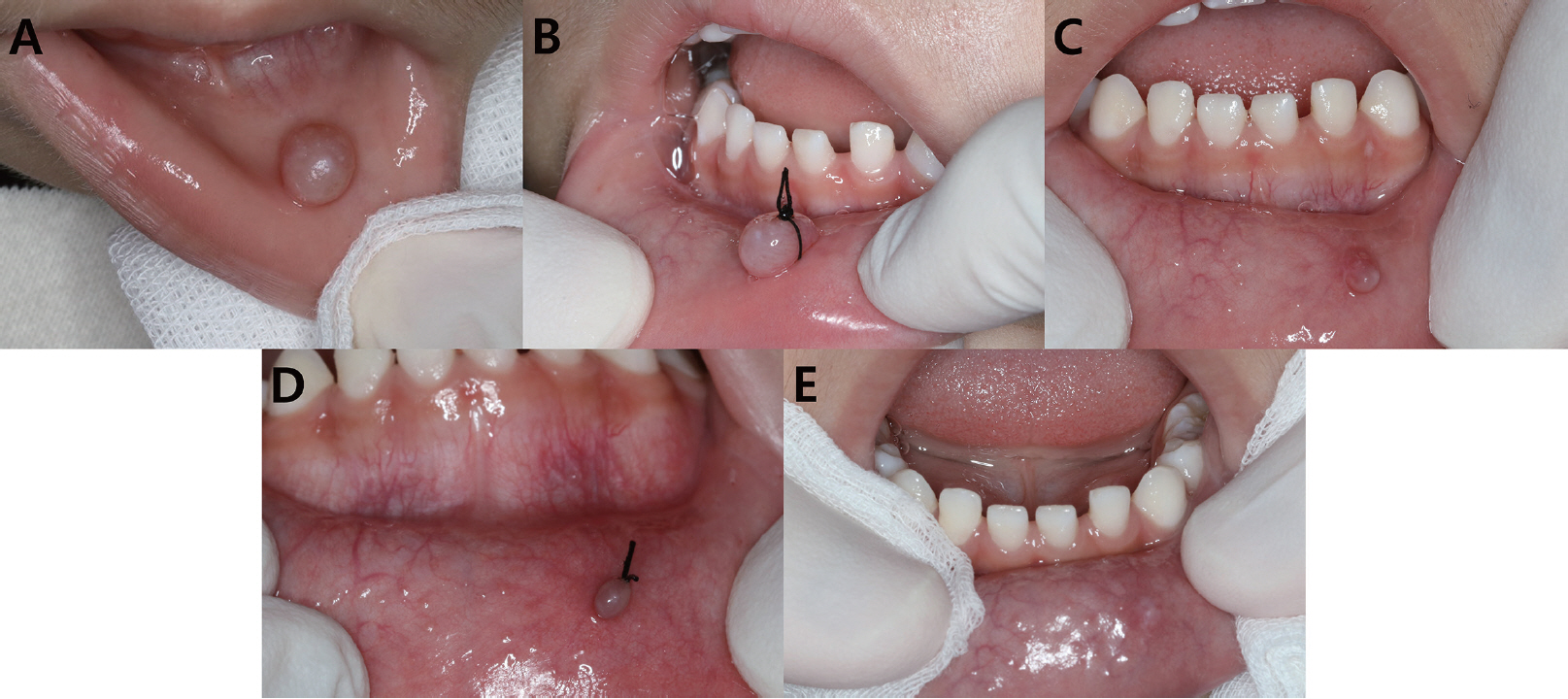
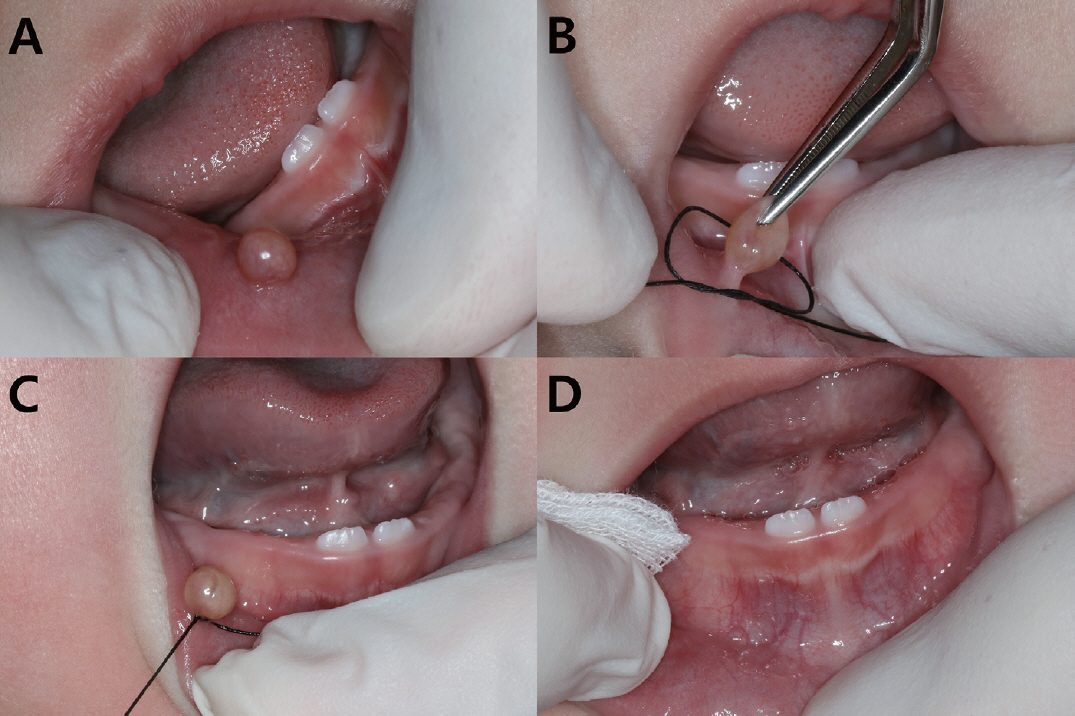
et al. : Treatment of mucus retention phenomena in children by the micromarsupialization technique.
Pediatr Dent, 22:155-158, 2000.

13. Berti SA, Santos JAR, Souza PHC, et al. : Micromarsupializa├¦├Żo: relato de dois casos cl├Łnicos. Rev Port Estomatol Cir Maxilofac, 47:151-155, 2006.
14. Knapp MJ : Oral disease in 181,338 consecutive oral examinations.
J Am Dent Assoc, 83:1288-1293, 1971.


15. Gallagher GJ : Biology and pathology of the oral mucosa. Dermatology in General Medicine. 4th ed. McGraw Hill Pub, New York, 1355-1416, 1993.
16. Shulman JD : Prevalence of oral mucosal lesions in children and youths in the USA.
Int J Paediatr Dent, 15:89-97, 2005.


17. Barlow SM, Rath EM : Maximum voluntary closing forces in the upper and lower lips of humans.
J Speech Lang Hear Res, 28:373-376, 1985.

18. Sumi M, Yamada T, Nakamura T,
et al. : MR imaging of labial glands.
Am J Neuroradiol, 28:1552-1556, 2007.



19. Choi YJ, Byun JS, Jung JK,
et al. : Identification of predictive variables for the recurrence of oral mucocele.
Med Oral Patol Oral Cir Bucal, 24:231-235, 2019.

20. L├│pez-Jornet P : Labial mucocele: a study of eighteen cases. Int J Dent Sci, 3:1-5, 2006.
21. Racey GL, Wallace WR, Marguard JV, et al. : Comparison of a polyglycolic-polylactic acid suture to black silk and plain catgut in human oral tissues. J Oral Surg, 36:766-770, 1965.
22. Selvig KA, Biagiotti GR, Wikesj├Č UM, et al. : Oral tissue reactions to suture materials. Int J Periodontics Restorative Dent, 18:475-487, 1998.
23. Sandrini FAL, SantŌĆÖana-Filho M, Rados PV : Ranula management: suggested modifications in the micro-marsupialization technique.
J Oral Maxillofac Surg, 65:1436-1438, 2007.


24. Giraddi GB, Saifi AM : Micro-marsupialization versus surgical excision for the treatment of mucoceles.
Ann Maxillofac Surg, 6:204-209, 2016.



25. Sagari SK, Vamsi KC, Saawarn S,
et al. : Micro-marsupialization: a minimally invasive technique for mucocele in children and adolescents.
J Indian Soc Pedod Prev Dent, 30:188-191, 2012.


26. Lee YS, Choi BJ, Son HK, et al. : Non-surgical treatment with tying of mucocele. J Korean Acad Pediatr Dent, 29:413-417, 2002.
27. Goyal S, Sharma , S , Diwaker P : Diagnostic role and limitations of FNAC in oral and jaw swellings.
Diagn Pathol, 43:810-818, 2015.














 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



