초록
동정맥 기형(Arteriovenous malformations, AVMs)은 동맥과 정맥이 직접적으로 연결되어 모세혈관과 연결되지 않은 희귀한 선천성 기형 중 하나이다. AVM은 유아기 후반이나 소아기까지는 임상적으로 나타나지 않을 수 있다. 특히 안면 AVM은 생명을 위협하는 치과적 응급 상황을 일으킬 수 있다.
전신병력이 없는 만 5세 여아가 하악 좌측 제2유구치의 후방 치은 주위의 자발적인 잇몸 출혈로 내원하였다. 감별진단 및 치료를 위해 전신마취 하에 대퇴정맥 접근을 통한 혈관조영술이 시행되었다. 동맥색전술 만으로도 혈류량이 효과적으로 감소되었다. 5개월 동안의 경과관찰에서 재발되지 않았다.
본 연구는 성장기 환자에서 이환된 혈관의 색전술이 외과적 절제술보다 더 효과적이고 안전한 방법이 될 수 있다고 보고하는 바이다.
Abstract
Arteriovenous malformations (AVMs) are rare congenital anomalies characterized by direct communication between arteries and veins that bypass the capillary bed. AVMs may not manifest clinically until late infancy or childhood. In particular, facial AVMs can cause urgent life-threatening dental events. A 5-year-old girl without a medical history visited the hospital because of spontaneous gingival bleeding around the posterior gingival area of the lower left 2nd primary molar.
Angiography through the femoral approach under general anesthesia was performed for differential diagnosis and therapeutic option. The blood flow was effectively reduced after arterial embolization alone, and there was no evidence of recurrence at the 5-month follow-up.
The present study reports that embolization of the affected vessels can be a more effective and safe method than surgical resection for the treatment of AVM during the growth period.
Keywords: Arteriovenous malformations, Angiography, Embolization, Spontaneous gingival bleeding
Ⅰ. Introduction
Arteriovenous malformations (AVMs) are rare congenital anomalies characterized by direct communication between arteries and veins that bypass the capillary bed[
1-
3]. AVM shows no signs until late infancy or childhood[
4]. Trauma, infection, or hormonal changes seem to contribute to their expansion[
1,
4,
5]. The most common clinical manifestations of AVM are bleeding, pain, and tissue destruction[
1,
2,
5].
AVM is a very rare disease, and its prevalence is difficult to estimate. In particular, extracranial AVMs in the head and neck are even more difficult to detect[
4-
7]. However, head and neck AVM (facial AVM) can cause urgent life-threatening dental events[
4-
6]. Therefore, dentists must have knowledge about the clinical symptoms of AVM in order not to cause an iatrogenic accident or a potential emergency situation[
4,
6,
7].
A wide variety of clinical signs and symptoms can be observed in facial AVMs. Patients may present with tooth mobility, facial asymmetry, ulceration, and bleeding[
1,
2,
5,
6]. Shöbinger[
8] classified the stages of AVM according to the clinical symptoms (
Table 1).
The main treatment options include embolization, surgical resection and combination therapy[
2,
9]. Surgical resection can cause massive bleeding; furthermore, children during the growth period may show impaired growth, which can cause facial asymmetry or dysfunction. Therefore, embolization of anomalous vessels is a safe and effective treatment option for children with AVM[
4,
10,
11].
Herein, we report the case of a 5-year-old girl with an AVM of the gingival area that was successfully treated with transfemoral venous embolization.
Ⅱ. Case Report
A 23-month-old girl without any medical history visited the Department of Pediatric Dentistry, Kyung Hee University Dental Hospital at Gangdong with swelling and bleeding in the gums involving the lower left posterior region. The left mandibular 2nd primary molar was not erupted. An incision was made to rule out an eruption cyst. Immediately after the injection needle was inserted for local anesthesia, pulsating bleeding occurred. Bleeding was difficult to control with buccellation or electrocautery. Under general anesthesia, the lesion was removed, and a biopsy specimen was obtained. Biopsy revealed a pyogenic granuloma. The bleeding was controlled, and the patient was uneventfully discharged from the hospital.
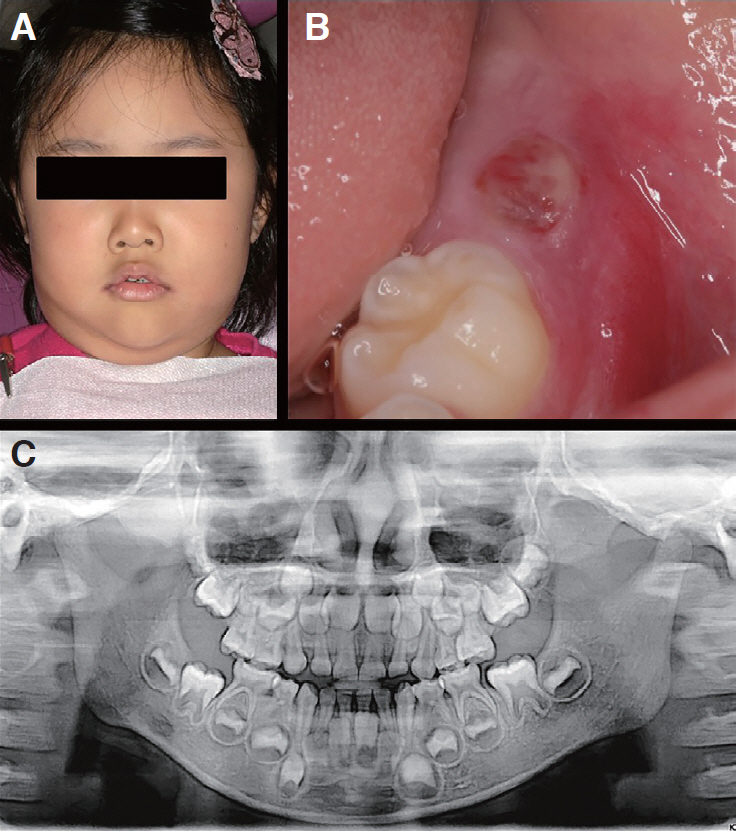
At the age of 5 years, the patient visited a regional hospital due to spontaneous gingival bleeding in the posterior gingival area of the lower left 2nd primary molar and was referred to our clinic. The left mandibular 1st molar was not erupted. Her parents reported gingival bleeding in the left mandibular posterior area for 10 days. Intraoral examination revealed arterial bleeding. On physical examination facial asymmetry with the left facial swelling was observed (
Fig. 1A). Panoramic and periapical radiography revealed no specific signs. After hemostasis, the lesion showed gingival redness, ulceration, and hypervascularization (
Fig. 1). Doppler ultrasound showed high-pitched sounds on the gingiva and buccal mucosa.
The patient was referred to a radiologist for differential diagnosis. Interventional angiography using a femoral approach was planned as a diagnostic and therapeutic option. The angiography was performed under general anesthesia. Angiography showed a high-flow vascular malformation with branches emerging from the facial and internal maxillary arteries, which appeared to drain into the facial vein early (
Fig. 2). At that time, branches of the facial and internal maxillary arteries were embolized with gelform, polyvinyl alcohol (PVA) particles, and glue/lipodol mixture infusion. Postoperative imaging revealed controlled lesions with the ablation of all branches. The blood flow was continued, but was reduced by 75 - 80% (
Fig. 2). After treatment with steroids and prophylactic antibiotics for 2 days, the patient was discharged following full recovery.
Follow-up studies included physical examination, panoramic radiography, and periapical radiography (
Fig. 3). There was no evidence of recurrence at the 5-month follow-up. Facial asymmetry was relieved and the permanent mandibular left 1st molar was erupted correctly.
Ⅲ. Discussion
AVM is rare congenital anomaly, especially within the maxillofacial area, which predominantly occurs in childhood. Bony involvement occurs in approximately 22% of cases, with the maxilla-mandibular bone being the most frequently involved[
5]. It can be fatal when an AVM occurs in the mandible, as routine dental treatment such as tooth extraction or simple incision can cause unexpected uncontrollable massive bleeding[
4,
6,
7].
Facial AVM can be suspected if clinical signs, including facial asymmetry, pain, swelling, redness, tooth mobility, or gingival bleeding, occur in patients without underlying disease[
1,
2,
5,
6]. Radiography demonstrated the bony involvement of facial AVM as lytic, multilocular or well-circumscribed lesions with a “soap bubble” or “honeycomb” appearance. In the mandible, lytic lesions are often radiographically similar to benign tumors[
2,
4].
AVMs are usually diagnosed by physical examination and imaging studies[
2,
6]. Selective angiography can be used for differential diagnosis[
4,
6]. For angiography, contrast media are injected into the vascular system, and blood flow is radiographically monitored by inserting a catheter into the vessels around the lesion. It can help select feeding vessels and perform embolization of the vessels[
4]. Therefore, surgical approaches to the affected area without embolization should be avoided, because this can cause uncontrollable bleeding when an incision is made in the affected area[
4,
6].
Contrast media mainly used for angiography are iodine agents and mostly water-soluble. They are discharged out of the body through the kidneys by glomerular filtration. There are side effects related to contrast agents such as allergic reactions or decreased renal function after angiography. Only rarely is renal damage from contrast media permanent. The incidence of allergic reactions have been observed in 2 - 10%. Allergic reactions range from hives and itching to facial and laryngeal edema, bronchospasm. Most reactions are minor and no treatment is required. Patients with a history of allergic reactions may benefit from steroid and antihistamine medication[
12].
The risk of infection after angiography is low, but antibiotics can be considered in the event of infection where the catheter was inserted. Antibiotics prophylaxis is not essential in angiography with careful technique[
13,
14].
Treatment methods for AVM include sclerotherapy, surgical ligation, radical resection, and embolization[
4,
6]. Vascular embolization with surgical resection is widely used as a standard treatment method[
2,
5,
6,
9]. However, surgical resection can result in massive bleeding and severe facial deformities, especially in growing children[
4,
10]. Recently, vascular embolization has been shown to be effective in treating facial AVM[
7,
9-
11]. Selective angiography is used to detect the arteries of the lesions, and embolizing materials can be placed in the suspected arteries. Materials that have been used for embolization include PVA particles, gel foam, metal coils, silicone fluid, isobutyl-2-cyanoacrylate, and collagen[
2,
4,
9]. Furthermore, it is possible to confirm the effect of the materials used to embolize the blood vessels of the lesions by angiography[
4].
Embolization may result in transient pain in the area of the embolized vessel and a mild febrile response for 24 to 48 hours. Other possible complications of embolization for AVMs include occlusion of a critical artery, erroneous embolization to a nonparticipating artery, and transvenous migration of the embolizing materials to the pulmonary vasculature[
15]. It is important to super select vessels. Embolization of a proximal vessel can open up the collateral vessels and cause recurrence or even further growth[
16].
Facial AVMs have a high risk of recurrence. They recur most frequently within the 1st year after treatment[
1,
17,
18]. Liu et al.[
17] reported a recurrence rate of AVM after treatment with embolization alone was 85.6% within 1 year. Despite the high likelihood of reexpansion, embolization can effectively palliate an arteriovenous malformation by reducing its size, slowing its expansion, and alleviating pain and bleeding.
Therefore, regular checkups are highly recommended for patients with AVM. In our case, blood flow was effectively reduced after arterial embolization alone. Since the patient was a 5-year-old girl in the growth period, further surgical resection was not performed. Even though the symptoms disappear, patients should be carefully followed up on a yearly basis to prevent possible relapse of the lesions.
Pediatric dentists should consider the possibility of AVM during mixed dentition. If AVM is suspected, a multidisciplinary team approach including radiologists and oral surgeons is mandatory. Embolization of the affected vessels can be a more effective and safe method than surgical resection during the growth period. AVMs have a high risk of re-expansion and recurrence. Therefore, yearly follow-up is important in detecting the potential recurrence of lesions.
Ⅳ. Summary
Facial AVM is a rare congenital anomaly with clinical signs including facial asymmetry, pain, swelling, redness, tooth mobility, and gingival bleeding. Selective angiography allowed the detection of specific arteries contributing to the lesions and the visualization of the placement of the embolizing materials. Angiography also allowed visualization of the effect of embolizing materials on blood flow to the area.
In this case, the AVM was located in the soft tissues. Facial asymmetry and spontaneous gingival bleeding were observed, but there were no bony changes or life-threatening bleeding. Spontaneous bleeding was thought to be affected by eruption of the 1st molar. The five-month follow-up showed no signs of recurrence and normal eruption of the 1st molar was observed. Although all signs are currently positive for effective treatment, this child should be monitored on a yearly basis for potential recurrence of a vascular malformation. When AVM is suspected, pediatric dentists should consider a multidisciplinary team approach, including radiologists and oral surgeons.














 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



