Introduction
Eruption is defined as the movement of a tooth from its developmental position to its functional position within the oral cavity, to form the occlusal plane [
1]. The eruption process may be disturbed due to several reasons; however, the 3 main causes are ectopic location of tooth germ, obstructions in the eruption path, and defects in the follicle or periodontal ligament [
1]. Displacement of unerupted tooth is uncommon and occur exclusively in the mandible. This type of eruption disturbance commonly involves either the mandibular second premolar (MnP2) or the mandibular canine (MnC) [
2]. An ectopically positioned tooth germ during eruption can cause impaction, while increasing the risk of root resorption, eruption disturbance, and cystic changes in adjacent teeth [
1,
3-
5]. As the mandibular first molar erupts much earlier than the MnP2, the distally displaced tooth germ of the MnP2 can obstruct the eruption path of the mandibular first molar and delay its eruption [
6].
To correct the position of an ectopically located tooth germ, intentional extraction of primary predecessors, surgical exposure, and surgical repositioning are considered [
1]. Many case reports have described the spontaneous eruption of an ectopically located permanent teeth following a combination of simple extraction of the primary predecessor and subsequent use of space maintainers [
1,
7,
8]. However, Fux-noy [
9] reported that the premature loss of mandibular primary second molar could lead to distal migration and ectopic eruption of the first premolar despite placement of a space maintainer. In such case, the space MnP2 eruption may be lost, resulting in its impaction. This implies that when the preceding primary second molar is intentionally extracted to improve the position of an ectopically positioned MnP2, the first premolar may incline distally during eruption, causing additional space management issues.
The present case report describes the treatment of 2 cases of distally displaced MnP2s and consequent impaction of mandibular first molars. These premolars erupted spontaneously following sequential extraction preceded by hemisection of the primary second molar.
Discussion
Delayed eruption of the mandibular first molars due to the ectopically placed MnP2 tooth germ, similar to that described in the present cases, is even rarer. The etiology of ectopic position of the tooth germ is unclear, but a hereditary origin can sometimes be established [
1]. The MnP2 shows great variation in its developmental pattern [
6] and can sometimes follow an incorrect eruption pathway. Eruption of premolars generally starts around the age of 10 years when root formation is initiated, while eruption of the mandibular first molar starts around the age of 6 years [
10]. If the tooth germ of MnP2 is distally displaced during the eruption of the first molar, its eruption path of the first molar gets obstructed, delaying to its eruption. Eruption failure of permanent molars may result in complications, such as posterior open bite, extrusion of antagonistic teeth, resorption and inclination of adjacent teeth, and formation of cyst [
11]. Any eruption disturbance of the first molars should be detected at an early stage, and eruption guidance should be performed as soon as possible.
The degree of root development is an important consideration when choosing a treatment strategy [
1,
8]. An immature root is beneficial for spontaneous eruption. Spontaneous eruption can be expected if the immature root has developed less than 2/3 of the total root length; however, if the root has developed more than 2/3 of the total root length or if there is no improvement in the spontaneous eruption path after removal of preceding primary tooth, active interventions such as surgical exposure or orthodontic traction are required [
1,
12,
13]. Spontaneous eruption could be expected because the root development was less than 2/3 of the expected total root length in both cases 1 and 2.
When a primary second molar is extracted prematurely, inclination of the adjacent teeth towards the extraction space and distal inclination of erupting mandibular first premolar are expected [
9,
14]. If this distal inclination of the mandibular first premolars occurs during the eruption guidance of MnP2s, it will lead to lack of space for spontaneous eruption, resulting in tooth impaction. Hemisection and sequential extraction of the preceding primary second molar were performed to retain the mesial root of the tooth in this case report. Extraction of the distal root provides space for the mesial migration of the displaced MnP2, and the retained mesial root prevents the distal inclination of the mandibular first premolar. Because the purpose of hemisection of mandibular primary second molars is to prevent distal inclination of the mandibular first premolars, it should be limited to patients with early mixed dentition in whom the first premolar has not been replaced. In both cases 1 and 2, the replacement of the mandibular first premolars did not occur; hence, eruption guidance by hemisection could be attempted.
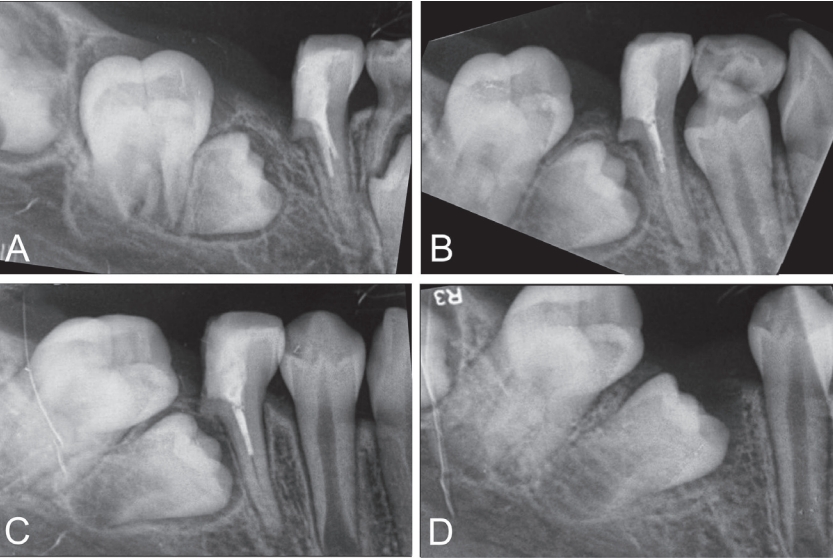
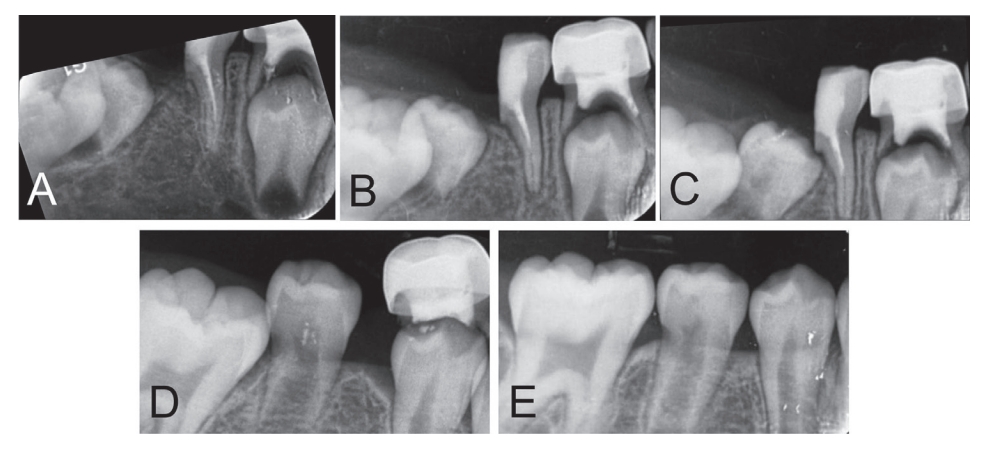
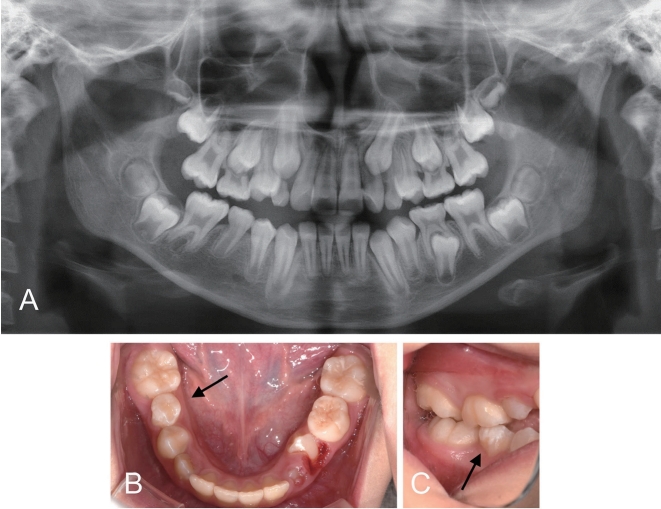
The mandibular first molars also showed mesial movement during the mesial shift of the MnP2s. This mesial movement of mandibular first molar would result in decreased arch perimeter. In case 1, the mandibular first molar erupted earlier than MnP2. A removable space maintainer was placed to prevent loss of space for eruption of the MnP2 and decrease in mandibular arch perimeter. In both cases 1 and 2, the distal displacement of mandibular first molars due to distally displaced MnP2s was observed(
Fig. 1, 4), thus, some extent of mesial shift of mandibular first molars could be allowed. However, if a significant reduction in the arch perimeter by excessive mesial shift of the first molar is expected, a distal shoe type space maintainer may be used.
Many clinicians have reported successful spontaneous eruption of ectopically positioned tooth germs, especially when the axial tilt of the premolar is less than 45┬░ [
6,
15]. If the axial tilt approaches 90┬░, active treatment options like surgical replantation, orthodontic traction, or extraction of the tooth may be necessary [
1,
16]. In case 1, although the axial tilt of the MnP2 approached 90┬░ in the mesiodistal direction, improvement of the axial tilt and spontaneous eruption was observed after hemisection and sequential extraction of the preceding primary tooth. This may have been because the intervention for eruption guidance of the angulated and displaced MnP2 started early at an appropriate time when the root development of the MnP2 was initiated.
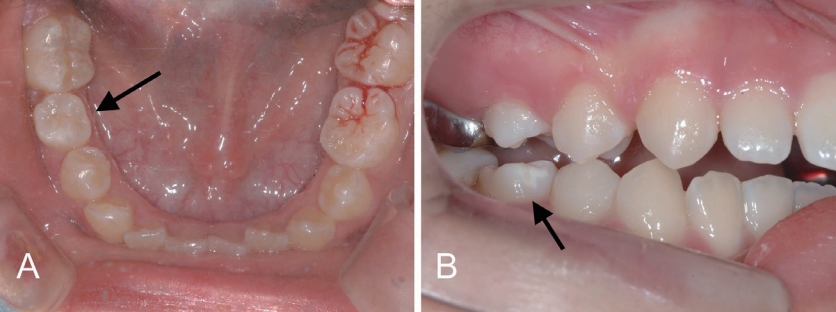
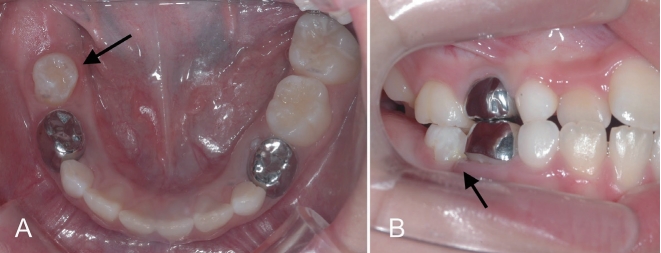
After completing eruption of the MnP2s, the teeth showed signs of enamel hypoplasia in both cases 1 and 2 (
Fig. 3B, 7C). The ectopic position of the MnP2s caused the tooth germ of the MnP2s and the mandibular first molars to be in close proximity, acting as physical obstructions to each other during tooth development. Further research is needed to clarify the causal relationship between the ectopic position of the tooth germ and enamel hypoplasia.
This study has a limitation: although eruption guidance of the two MnP2s was achieved, both teeth were rotated (
Fig. 3A, 6A). The need for further orthodontic treatment was inevitable in both cases. Despite this limitation, the strength of this case report is that it addresses the unfavorable distal inclination of the mandibular first premolars during eruption guidance of distally displaced MnP2s. Hemisection can help spontaneous eruption of distally displaced MnP2 as a less invasive treatment strategy to avoid surgical exposure or orthodontic traction.











 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



