소아용 크라운 수복을 위한 3D 프린팅 레진과 레진 시멘트 간의 접착 강도 평가
In Vitro Study on the Bond Strength Between 3D-Printed Resin and Resin Cement for Pediatric Crown Restoration
Article information
Abstract
3D 프린터로 출력된 레진 크라운은 유치의 심미 수복을 위한 크라운으로 사용될 수 있으며, 접착에는 주로 레진 시멘트가 사용된다. 본 연구의 목적은 크라운 제작용 3D 프린팅 레진의 접착 능력을 평가하고, 이를 다른 레진 간접 수복용 재료들과 비교하는 것이었다. 3D 프린팅 레진인 Graphy (GP)와 NextDent (NXT), 레진 간접 수복용 재료인 MAZIC Duro (MZ)와 VIPI Block (VIPI)의 전단결합강도가 본 연구에서 비교되었다. GP, NXT, MZ, VIPI군의 평균 전단결합강도는 각각 23.29 ± 3.88, 26.14 ± 4.67, 25.41 ± 4.03, 18.79 ± 4.26 MPa였다. VIPI군을 제외한 GP, NXT, MZ군의 평균 전단결합강도 값에는 유의미한 차이가 없었다. 본 연구 결과 3D 프린팅 레진은 레진 시멘트와 임상적으로 허용 가능한 수준의 접착 강도를 나타냈으며, 이에 따라 유치 수복을 위한 크라운 재료로서 적합한 조건을 갖추고 있음을 확인하였다.
Trans Abstract
A 3D-printed resin crown is a novel option for esthetic crown restoration for primary teeth, which are typically bonded with resin cement. The purpose of this study was to evaluate the bonding ability of a 3D printing resin and compare it with other indirect resin materials for crown fabrication. The shear bond strengths of two 3D printing resin materials, Graphy (GP) and NextDent (NXT), and two indirect resin materials, VIPI Block (VIPI) and MAZIC Duro (MZ), were compared in the study. For all materials, the shear bond strength at the interface between the surface of the resin material and resin cement was measured. The mean shear bond strength values of GP, NXT, MZ, and VIPI were 23.29 ± 3.88, 26.14 ± 4.67, 25.41 ± 4.03, and 18.79 ± 4.26 MPa, respectively. There was no significant difference among the SBSs of GP, NXT and MZ except for VIPI. The result of this study indicates that the 3D printing resin meets the essential requirement for clinical use by showing clinically adequate bond strength.
Introduction
Nowadays, esthetic demands are increasing in pediatric dentistry [1]. Parents do not downplay the esthetic value of primary teeth for the reason that they will fall out soon. When restoration is required for a decayed tooth, they hope it recovers its original shape and color [2]. 3D resin crowns can be a good choice for pediatric dentists planning an esthetic crown restoration. The most widely used pediatric crown so far is the stainless steel crown, but it has caused dissatisfaction for some parents due to its metallic appearance [2]. The zirconia crown is a more esthetic option, but still has disadvantages such as wear on the opposite teeth and high costs[3]. Accordingly, a 3D resin crown is emerging as a new option in the context of ongoing efforts to develop an ideal esthetic crown. The 3D-printed resin crowns surpass other prefabricated crowns for children, such as stainless steel and zirconia crowns, in that they can be fabricated in both standardized and customized form for each tooth.
The production of dental crowns with 3D-printed resin, in particular, has numerous advantages over conventional crown production methods. Previously, prostheses designed with computer-aided design (CAD) software were mainly manufactured through subtractive computer-aided manufacturing (CAM) methods [4,5], which tended to waste materials and milling tools. Also, milling with bars is a suboptimal method of contouring [6], whereas 3D printing-based additive methods save materials and simplify the shaping of complex structures such as the internal surface of the crown [7]. However, since there is little research on this new technology, the 3D printing resin materials should be assessed from various aspects.
It should be emphasized that the 3D-printed resin crown is a subcategory of pre-cured resins, or, in other words, indirect resin restoration (IRR). IRR was introduced to overcome the shortcomings of direct resin restoration by avoiding the negative effects of polymerization shrinkage that occurs during curing. Besides, mechanical properties were improved in IRR by increasing the degree of conversion [8-10]. However, the high degree of conversion has been accompanied by decreased bonding ability [8,9]. Advances in dental materials have led to the development of diverse resin-based materials and bonding systems with improved mechanical and chemical properties, including 3D printing resins [10]. Although the properties of 3D printing resins are actively being investigated, there have been only a few studies evaluating their bond strength [11,12].
This study aimed to evaluate the bonding ability of 3D-printed resin for pediatric crown restoration. The cementation of indirect restorations involves two interfaces: the interface between the tooth surface and the cement and the interface between the surface of the restoration and the cement [13,14]. In this study, we evaluated the shear bond strength (SBS) between the surface of the restoration and the cement. To evaluate the bonding ability of 3D printing resins, we compared the SBS values among 3D printing resins and indirect resin restoration materials for crown fabrication. This study’s null hypothesis was that different types of indirect resin materials have no effect on SBS.
Materials and Methods
1. Specimen fabrication
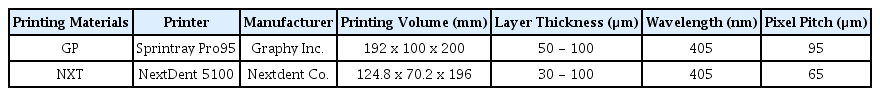
A total of 60 specimens were prepared with 4 types of resin materials: two 3D printing resins, Graphy TC-80DP (GP; Graphy Inc., Seoul, Republic of Korea), and Nextdent C&B MFH (NXT; NextDent, Soesterberg, The Netherlands); a nano-hybrid ceramic, MAZIC Duro (MZ; Vericom, Chuncheon, Republic of Korea); and an organically modified polymethylmethacrylate (PMMA) ceramic, VIPI Block Trilux (VIPI; VIPI Indústria, Pirassununga, SP, Brazil). The components and manufacturers of each material used in the study are summarized in Table 1. GP and NXT discs (thickness, 2.0 mm; diameter, 8.0 mm) were printed using each company’s digital light processing (DLP) printers according to the layer thickness recommended by manufacturers (Table 2). After printing was complete, discs were washed for 5 minutes in an ultrasonic washing machine (Twin Tornado, Medifive, Seoul, Republic of Korea) with resin cleaner (Twin 3D Cleaner, Medifive) to remove excessive resin monomers. The post-curing process for GP specimens was conducted for 30 × 30 minutes in a post-curing unit (The CureM U102H, Graphy Inc.), and the NXT specimens were post-cured for 30 minutes using a post-curing machine (LC-3DPrint box, NextDent, 3D systems, Rock Hill, SC, USA). The VIPI specimens were milled, and the MZ specimens were cut into 2.0 mm-thick discs. The specimens were embedded in cylinders of self-polymerizing resin (Trayplast NF, Vertex Dental B.V., Zeist, The Netherlands), and their faces were polished flat with a 600-grit abrasive paper under running water.
2. Luting of specimens with resin cement and storage
Prior to luting of specimens, air abrasion was performed with 50 µm aluminum oxide (Al2O3) particles from a distance of 10.0 mm, with a pressure of 2 bar, using an airborne-particle abrasion device (Cobra, Renfert GmbH, Hilzinge, Germany) for 10 seconds. The specimens were rinsed with running water and air-dried with oil-free compressed air. Afterwards, the Scotchbond Universal adhesive (3M ESPE, Seefeld, Germany) was applied to all disc surfaces and dried without light curing according to the manufacturer’s instructions. The Rely X Ultimate resin cement (3M ESPE, St. Paul, MN, USA) was delivered in an automix syringe containing base paste and catalyst paste. It was injected into a cylindrical hole (width, 2.38 mm; height, 2.50 mm) of a teflon mold placed over each disc and light-cured with an LED light curing unit, BeLite S (B&L Biotech, Ansan, Republic of Korea), for 20 seconds. BeLite S emits energy over a wavelength range of 430 - 490 nm with a single peak at 460 nm. Among several curing modes in BeLite S, the general composite filling mode (Norm mode, 800 mW/cm2) was used. The tip diameter of BeLite was 8.8 mm. To simulate oral conditions, all samples were placed in distilled water in an incubator at 37℃ for 24 hours.
3. Evaluation of the SBS between the resin cement and the specimen
After incubation, the SBS between each specimen and the resin cement was measured using a shear bond tester (Bisco Inc., Schaumburg, IL, USA) with a crosshead speed of 1 mm min-1. For each specimen, the force at bond failure was obtained in Newtons (N). The SBS was calculated in megapascals (MPa) as follows: SBS = force/surface area of adhesion.
The fractured surfaces were visually analyzed to determine the mode of failure for each specimen. Adhesive failure was defined as resin cement completely separated from the surface of the composite; cohesive failure was defined as a completely fractured resin disc or cement; and mixed failure was defined as both adhesive and cohesive failures observed.
4. Evaluation with scanning electron microscopy
Representative failed specimens from each resin were observed under a scanning electron microscope (SEM; JEOL-7800F, JEOL, Tokyo, Japan), which features a deeper depth of field and higher resolution than a light microscope. Each specimen was mounted with a carbon adhesive, coated with gold palladium, and photographed at 50× magnification for SEM imaging.
5. Statistics
Differences among groups were evaluated with a Kruskal-Wallis test followed by a Bonferroni correction for multiple comparisons. All statistical tests were performed in SPSS version 23.0 (IBM Corp., Armonk, NY, USA) with the cutoff for significance set at α = 0.05 for a Kruskal-Wallis test, and α = 0.0125 for a Bonferroni correction.
Results
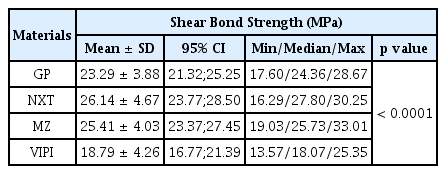
The mean SBS values of GP, NXT, MZ, and VIPI were 23.29 ± 3.88, 26.14 ± 4.67, 25.41 ± 4.03, and 18.79 ± 4.26 MPa, respectively. SBS values differed significantly between resins (p < 0.0001; Table 3) and were significantly lower in the VIPI group than in the NXT and MZ groups. However, there were no significant differences between the GP, NXT, and MZ groups (Table 4). The boxplots showing the SBSs of each material are presented in Fig. 1.
Boxplots showing the shear bond strength (MPa) of different resin materials. The lower and upper borders of each box indicate the 25th and 75th percentiles of SBS in each group, respectively; the line inside the box denotes the median; the dot inside the box denotes the mean; and the lower and upper whiskers represent the minimum and maximum values within 1.5 times the inter-quartile range (IQR). IQR: inter-quartile range; GP: Graphy TC-80DP; NXT: Nextdent C&B MFH; MZ: MAZIC Duro; VIPI: VIPI Block Trilux.
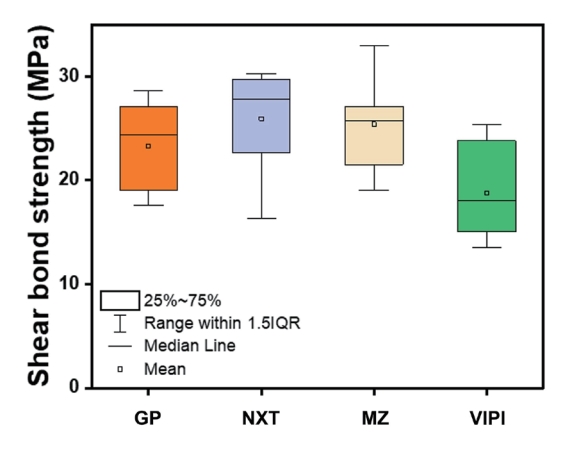
All specimens except those in the VIPI group showed cohesive failures. 20% of specimens in the VIPI group showed adhesive failures, and 80% showed mixed failures (Fig. 2). Representative SEM images of the failure modes of each resin group are shown in Fig. 3. As shown on the SEM images, All GP, NXT, and MZ specimens with cohesive failures were fractured inside the specimen, with a characteristic larger fractured area than bonding area. The VIPI specimens with adhesive failures showed a flat surface with a constant texture. Although most of the VIPI specimens showed mixed failures, most of the changes that occurred inside the specimens were cohesive crack lines. The VIPI specimens with mixed failure and cohesive fracture inside the cement showed an irregular surface with a partially flat area (Fig. 3).
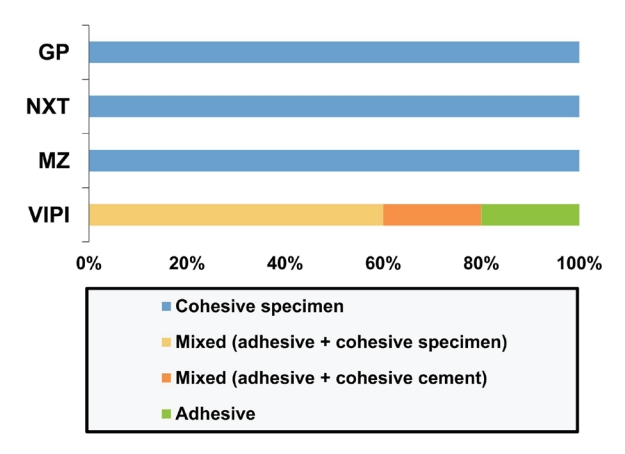
Comparison of failure modes among different groups of resin materials. GP: Graphy TC-80DP; NXT: Nextdent C&B MFH; MZ: MAZIC Duro; VIPI: VIPI Block Trilux.
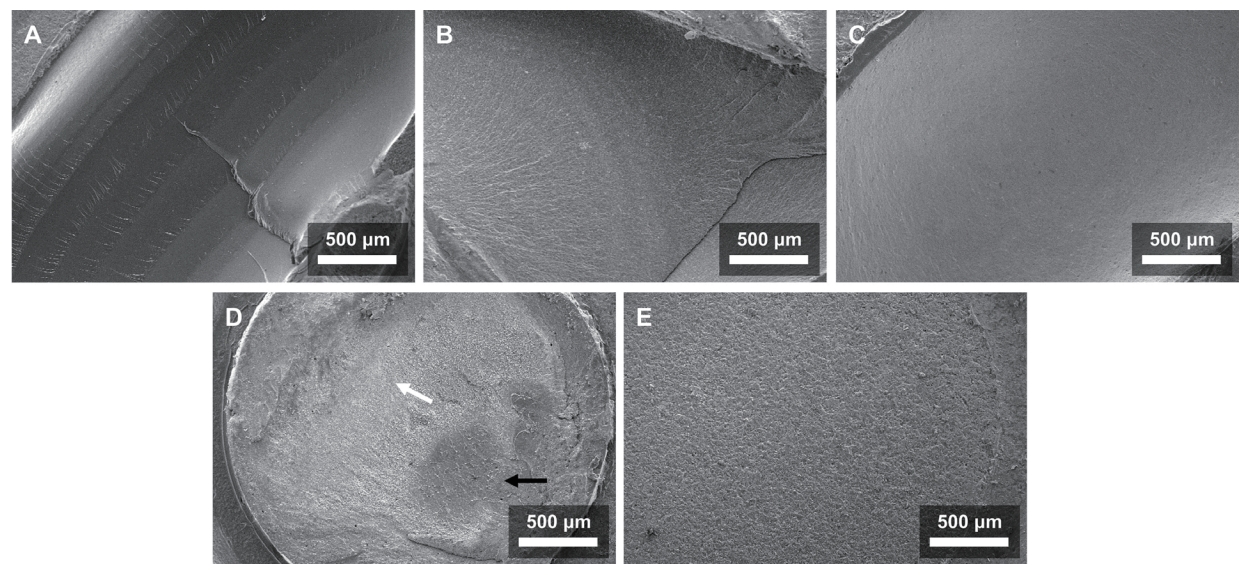
Scanning electron microscopy images of resin samples (×50). (A) GP with cohesive failure inside the specimen, (B) NXT with cohesive failure inside the specimen, (C) MZ with cohesive failure inside the specimen, (D) VIPI with mixed failure, including cohesive failure inside the cement (white arrow) and adhesive failure (black arrow), (E) VIPI with adhesive failure.
Discussion
A 3D-printed resin crown is a novel pediatric crown that features esthetic benefits and manufacturing advantages. However, since 3D printed restoration is a type of IRR, it is essential to evaluate not only the mechanical properties but also the bonding ability of the material. The bond strength between pediatric zirconia crowns and resin cement was estimated in several articles; it was 18.79 MPa in the study of Lee et al. [15] and 16.4 MPa in the study of Ishii et al. [16]. In this study, we measured the SBS between 3D-printed resin and resin cement to confirm that it has clinically acceptable bonding ability, and compared the SBS values among different IRR materials.
IRRs with a high degree of conversion have a limited number of freely accessible C=C double bonds left, which are required for the formation of new covalent bonds with the resin cement. This can be detrimental to the bonding between the surface of the restoration and the resin cement [8,17-20]. Although there are other bonds, such as Van der Waals bonds, hydrogen bonds, and ionic bonds, they contribute to chemical bonding only to a small extent. As such, adhesion between the IRR and resin cement likely involves mechanical bonding [14,17,21,22]. The monomers in bonding materials polymerize within micro-grooves on the surface, leading to mechanical interlocking [17,22]. To improve the bond strength of IRRs, sandblasting is recommended, which is the most definitive pretreatment method to increase the surface roughness of the IRR [13,20,23]. In addition, using a bonding agent that is compatible with the resin cement is important for successful bonding [13,20]. Accordingly, all specimens were sandblasted with Al2O3, and Rely X Ultimate cement and Scotchbond Universal adhesive were used for luting in this study. Since chemically active components, such as 10-methacryloyloxydecyl dihydrogen phosphate (MDP) and silane, were included in the Scotchbond Universal adhesive, it also aided in the formation of chemical bonds with fillers and the ceramic components of the restorative materials [24,25].
The mean SBS value of GP, NXT, MZ, and VIPI was 23.29 MPa, 26.14 MPa, 25.14 MPa, and 18.79 MPa, respectively. The mean SBSs of 3D printing resin (GP and NXT) in the present study were comparable to the mean microtensile bond strength of 23.20 MPa reported by Pfeffer S. et al. who tested the microtensile bond strength between a 3D-printed resin specimen and a dual-cure resin [11]. At present, there is no official recommendation on the range of bond strength for crown restorations. Moreover, the bond strength required for luting IRRs has not been investigated in longitudinal clinical studies. Nevertheless, Matsumura et al. regarded 10 - 20 MPa as the minimum bond strength required for crown prostheses [26]. Other studies have argued that for composite repair, an SBS of 18 - 25 MPa is clinically acceptable for occlusal function survival [27]. Considering these recommendations and referring to the bond strength between zirconia crowns and resin cement measured in previous studies, despite the lack of official requirements, we could draw a conclusion that the mean SBS values of all resin materials in this study were all within the clinically acceptable range.
Except for the VIPI group, which had mixed and adhesive failures, all groups experienced cohesive failure. Cohesive failures may indicate that the exhibited stress exceeded the tensile strength of the specimen before the real bond strength was challenged. As a result, these failures are mostly associated with higher MPa values, as in the present study [28]. However, the fact that most of the cohesive failures occurred inside the resin specimen can mean that the mechanical strength of the resin materials may not be sufficient. Hence, further evaluation of the mechanical properties of the resin-based indirect materials, including 3D printing resin, is required. CAD/CAM PMMA resins such as the VIPI Block exhibit good mechanical properties, but their wettability and bond strength are known to be lower than those of traditional PMMA materials [29,30]. It can be inferred that the VIPI group had loose mechanical interlocking between the resin and resin cement, which caused more frequent mixed and adhesive failures and a lower SBS value than other groups.
This study has some limitations. First, we used a single luting protocol for different resin materials with different bonding processes. Therefore, our comparison of the bonding capacities of these materials may have been imprecise. Second, we did not assess long-term changes in bond strength, even though the bond strength between the polymer and cement can change over time. Third, we did not quantitatively assess the surface properties of resins (such as the surface energy, roughness, and wettability), which will provide more information related to the bonding ability.
Future studies should evaluate the long-term changes in bond strength to determine the long-term survival of dental restorations, and the surface properties of resin specimens.
Conclusion
To summarize, we reject the null hypothesis that different types of indirect resin materials have no affect the SBS at the 5% significance level. However, there was no significant difference in mean SBS values among 3D printing resin groups (GP and NXT) and a nano-hybrid ceramic group (MZ), except for a PMMA group (VIPI), which showed the lowest value. Furthermore, despite the comparably low SBS value of the VIPI group, the SBS values of all materials evaluated in the study were verified to be above the clinically acceptable thresholds. Hence, we can draw a conclusion that 3D printing resin shows adequate adhesion with resin cement and it meets the essential requirement of bonding ability for clinical use.
Notes
Conflict of Interest
The authors have no potential conflicts of interest to disclose.
Funding information
Study was supported by the Korea Medical Device Development Fund grant funded by the Korea government (the Ministry of Science and ICT) (Project Number: 1711138576, KMDF_PR_20200901_0260).
Acknowledgements
Study was supported by the Korea Medical Device Development Fund grant funded by the Korea government (the Ministry of Science and ICT) (Project Number: 1711138576, KMDF_PR_20200901_0260).