Assessment of Risk Factors for Dental Developmental Disorders in Pediatric Cancer Survivors
Article information
Abstract
This study was to examine the developmental dental abnormalities in childhood cancer survivors. Risk factors were assessed for 125 children with radiographic data through a retrospective analysis of medical records and panoramic images. 68.0% of childhood cancer survivors exhibited at least one dental abnormality. The types of abnormalities varied depending on the age at cancer diagnosis and treatment intensity, ranging from microdontia (43.2%), to abnormal root development (39.2%) and tooth agenesis (33.6%). Logistic regression analysis demonstrated that a young age at diagnosis (under 3 years), the use of heavy metal agents, a history of hematopoietic stem cell transplantation (HSCT), and combination treatment of chemotherapy, radiation therapy, and HSCT were associated with a significantly higher risk for overall dental abnormalities. The increased risk ratios were 6.00, 3.06, 3.22, and 7.87, respectively (p < 0.05). The results of this study will predict dental abnormality in permanent dentition according to the diagnosis age and treatment method of childhood cancer.
Introduction
Improved treatment methods and early diagnosis have led to a continuous increase in the survival rates of cancer patients [1]. However, there are still evident late side effects that emerge during or after cancer treatment, and identifying these side effects is clinically important. While cancer treatment is effective, it also negatively impacts the normal structures surrounding the tumor. These treat-ment methods can cause long-term and potentially fatal consequences due to their association with delayed toxicity [2].
Chemotherapy and radiotherapy treatments for childhood cancer survivors (CCS) aim to only damage cancer cells while minimizing harm to normal tissues, but their lack of specificity can interfere with dental and facial development, leading to irreversible developmental defects such as tooth agenesis, microdontia, and abnormal root development [3,4]. Additionally, cancer treatments often induce side effects such as reduced appetite, vomiting, and diarrhea in cancer patients. As a result, their nutritional status can decline, potentially impacting tooth development. Furthermore, due to the suppressed immune system, oral infections and inflammation can also affect tooth development. A study comparing dental abnormalities between children who received cancer treatments and their siblings showed that the group that received cancer treatments showed significantly more evidence of tooth agenesis, microdontia, enamel hypoplasia, thin roots, and root constriction [5].
The potential side effects on teeth that result from cancer treatments can vary depending on factors such as age, radiation dosage, the radiation field size, specific chemotherapy drugs used, and whether hematopoietic stem cell transplantation (HSCT) was performed. These factors can influence the severity and type of dental complications that may arise [6]. While dental abnormalities occurring in CCS may not directly threaten life, the complications of cancer treatment can significantly impair the quality of life. Therefore, it is essential for pediatric dentists to be familiar with the side effects of cancer treatment when children with cancer visit the dental clinic. They should have a good understanding of these effects and be able to effectively communicate them to both parents and children. Providing comprehensive explanations about the potential oral complications related to cancer treatment can help parents and children understand the importance of oral health care during and after cancer treatment. It also allows them to actively participate in preventive measures and seek appropriate dental management to minimize the impact of these side effects.
In 2019, Lee et al. assessed dental developmental abnormalities based on a diagnostic age criterion of 6 years [7]. In 2022, Kim et al. investigated dental abnormalities in patients who underwent HSCT [8]. This study analyzes and confirms dental abnormalities in patients, considering not only the impact of HSCT but also various risk factors such as gender, surgery, radiation, chemotherapeutic agents, treatment modality, and treatment duration. The study uses 3 and 6 years of age at diagnosis as reference points for the analysis.
The aim of the study was to assess the occurrence of dental complications after the completion of cancer treatments and to analyze the types and prevalence of developmental dental abnormalities in CCS resulting from cancer treatment outcomes.
Materials and Methods
1. Study population
In this study, we investigated the patients who met the following inclusion criteria: 1) patients who visited the long-term follow-up clinic of the pediatric hematology and oncology department at Yonsei University Hospital’ s Childhood Cancer Center from January 1, 2018, to May 31, 2023; and 2) patients who visited the pediatric dentistry clinic and had panoramic radiographs taken. Initially, a total of 233 patients were identified; however, 108 patients were excluded due to the following exclusion criteria: 1) lack of panoramic radiographs taken one year after completion of cancer treatment; 2) loss of followup; and 3) patients undergoing cancer treatment or experiencing a relapse. As a result, 125 CCS were included in the study. These CCS were followed up for at least 1 year after completing their cancer therapy.
1) Demographics and evaluated risk factors
A retrospective analysis was conducted using medical records and panoramic images to evaluate the study subjects. The complete medical records of all patients were obtained from the pediatric hematology and oncology department. Key variables, including gender, cancer type, age at cancer diagnosis, age at completion of treatment, treatment duration, treatment modality, type and number of administered drugs, dose and site of radiation, HSCT, and surgery intervention status, were recorded. Patients were divided into three groups based on age at cancer diagnosis: the youngest group (≤ 3 years old), the middle group (3 - 6 years old), and the oldest group (≥ 6 years old). The radiation dosage used for cancer treatment was calculated based on the total radiation dose administered during treatment. The class of chemotherapeutic agents was defined by the mechanisms of action for each agent. The total number of chemotherapeutic agent classes used for each CCS was recorded to estimate the toxicity of chemotherapy; “multiple classes” was defined as ≥ 4 classes.
2) Diagnosis of dental developmental disturbances
Dental abnormalities were assessed by a single pediatric resident through panoramic radiographic images. Panoramic images were taken before and after treatment. To assess the intra-rater reliability, observations for all panoramic images were conducted three times at three-week intervals. Intra-rater reliability was evaluated using the kappa coefficient value and showed a fairly high level of reliability (intraclass correlation coefficient = 0.92). The following signs of dental developmental disorders were observed and examined: tooth agenesis, tooth size, and root morphology.
(1) Tooth agenesis
Tooth agenesis was defined as the congenital missing of a permanent tooth or tooth germ. The third molars were excluded. Regarding tooth agenesis, a tooth was not considered missing before a certain age: first premolar, < 5 years; second premolar, < 6 years; and second molar, < 7 years.
(2) Tooth size
For tooth size, if there was a difference of more than twice the standard deviation from the average tooth size or a significant deviation from the expected tooth size based on normal, it was classified as a microdontia [9-12].
(3) Root morphology
The adjacent teeth and their roots were used as a reference. The roots were classified into two categories based on their deviation from normal root morphology: when the root tapering exceeded normal convergence and the relative ratio between root and crown was 0.8 - 1.6 and greater than 50% normal root length, we called it a shortened tapered V-shaped root. We called it a short and blunt U-shaped root when it exhibited a relative ratio between root and crown under 0.8 and less than 50% of normal root length. The longest root was used for evaluation in the case of multiple roots. In this study, we refer to the combination of V-shaped roots and U-shaped roots as abnormal root development (Fig. 1).
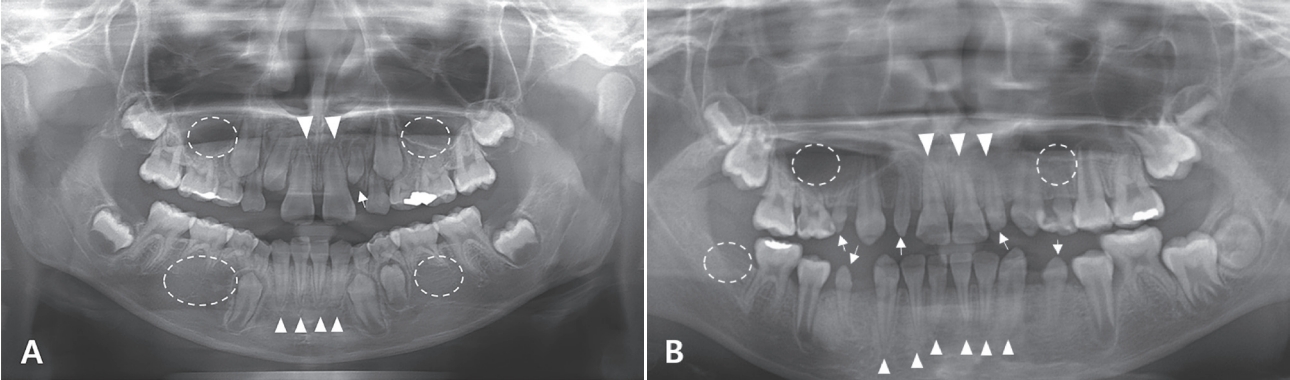
Examples of dental anomalies observed in the panoramic view are depicted in (A) and (B). These anomalies include tooth agenesis in permanent teeth (asterisk), microdontia (arrowhead), and root malformation (triangle).
For teeth with ongoing development with an unclear final morphology, missing teeth that are not categorized in the agenesis group at a young age, teeth that had already undergone extraction at a young age, and teeth that did not have an accurate appearance in the panoramic view, they were not classified into any category.
2. Statistical analysis
Characteristics of CCS according to the diagnostic age and the number of teeth were analyzed using the Kruskal-Wallis test. Diagnosis, treatment modalities, prevalence, and incidence, as well as the association between the number of teeth and characteristics, were evaluated using exact chi-square tests. Logistic regression models were used to assess the association between the risk factors and severely abnormal disturbances. A 95% confidence level was used. All statistical analyses were performed using the SPSS program (Version 26.0, SPSS, Chicago, IL, USA).
1) Ethical statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Board of Yonsei University Dental Hospital (approval No.: 2 - 2023 - 0003). The requirement for informed consent was waived.
Results
1. Population demography
Among the 125 CCS, 69 were boys and 56 were girls. The median age at cancer diagnosis and completion of treatment was 2.92 ± 3.39 and 5.42 ± 3.42 years, respectively. The median age at evaluation and radiation was 10.67 ± 4.58 and 3.38 ± 2.91 years, respectively. The median treatment duration was 1.33 ± 1.89 years. The median number of chemotherapy classes received was 4, and the total number of chemotherapeutic agents administered was 7. For CCS who received radiation therapy, the median radiation dose was 40.80 Gy.
The most prevalent childhood cancer observed was acute lymphoblastic leukemia (28.8%). The next most common category was others (18.4%), which included neuroblastoma, Langerhans cell histiocytosis, hepatoblastoma, and others. Following that, the occurrence of cancer was observed in the following order: lymphoma, brain tumor, sarcoma, acute myeloid leukemia, retinoblastoma, and abdominal Wilms tumors.
100% of the survivors received chemotherapy treatment. Out of the survivors, 52 survivors (41.6%) received chemotherapy alone, while 35 survivors (28.0%) underwent HSCT in addition to chemotherapy. Additionally, 19 survivors were treated with radiation therapy (RT), and another 19 survivors received both RT and HSCT concurrently (Table 1).
2. Dental abnormalities
Panoramic radiographs of 42 patients (33.6%) showed no dental abnormalities; the remaining 83 patients (66.4%) showed at least one abnormality. The most common combination of abnormalities observed overall was ‘tooth agenesis + microdontia + abnormal root development’ (17.6%). In the youngest age group, ‘tooth agenesis + microdontia + abnormal root development’ (27.69%) was the most prevalent. In the middle group, ‘abnormal root development only’ was the most common (33.33%). ‘Normal dental development’ was the most prevalent in the oldest group, followed by ‘abnormal root development only’ (13.33%, Table 2).
The prevalence of tooth agenesis, microdontia, abnormal root development, and oligodontia showed significant differences depending on age. In particular, tooth agenesis and microdontia were more prevalent in the youngest group, while abnormal root development was most commonly observed in the middle group. Oligodontia, on the other hand, was only observed in children diagnosed in the youngest group (Table 3).
Similar to the prevalence, the number of affected teeth for tooth agenesis and microdontia was significantly higher in the youngest group (p < 0.0001). For abnormal root development, it was observed to have a higher impact in the middle group, with an average of 8.83 affected teeth, surpassing the overall group average (p < 0.0001, Table 4).
It can be observed that the lower second premolars were the most commonly affected teeth by tooth agenesis (25.84%). Microdontia was predominantly found in the upper second molars (17.28%), followed by the lower second molars (16.46%). Abnormal root development was commonly observed in the lower anterior teeth, for the lower central incisor (14.03%) and the lower lateral incisor (13.63%), respectively (Fig. 2).
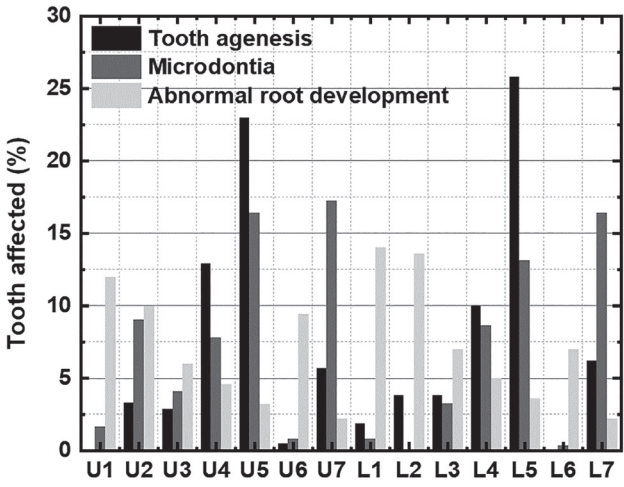
Distribution of teeth affected by tooth agenesis, microdontia, and abnormal root development. The lower second premolars were the most commonly affected teeth by tooth agenesis, accounting for 25.84%. Microdontia was predominantly observed in the upper second molars, representing 17.28%. Abnormal root development was predominantly found in the lower central incisors, accounting for 14.03%.
Brain tumor showed significant differences in abnormal root development, and treatment duration showed significant differences in microdontia. Using multiple classes of chemotherapeutic agents, HSCT, surgery showed significant differences in tooth agenesis and abnormal root development. Finally, differences in age of diagnosis, using heavy metal agents, and treatment modality showed significant differences in tooth agenesis, microdontia, and abnormal root development (Table 5).

The association between the number of teeth affected by dental abnormalities and their characteristics
In the regression analysis, the youngest group showed odds ratios (OR) of 6.30 and 25.56 for tooth agenesis and microdontia, respectively, compared to the oldest group. The middle group exhibited an OR of 5.23 for abnormal root development. Additionally, the use of heavy metals showed higher ORs of 4.24, 2.23, 3.80 for all three categories: tooth agenesis, microdontia, and abnormal root development. Having multiple classes and undergoing HSCT or surgery were identified as severe risk factors for tooth agenesis and abnormal root development. Furthermore, treatment involving chemotherapy and RT combined with HSCT showed ORs of 7.22, 5.11, and 54.64 for tooth agenesis, microdontia, and abnormal root development, respectively, compared to treatment with HSCT alone (Table 6).
Discussion
We investigated significant risk factors for dental developmental abnormalities in CCS across various age groups, and we found that childhood cancer treatments often lead to developmental abnormalities in permanent teeth. In our study, at least 68.0% of the CCS exhibited at least one dental abnormality. The types of abnormalities varied depending on the age at cancer diagnosis and treatment intensity, ranging from microdontia (43.2%), early termination of root formation resulting in abnormal root development (39.2%), and tooth agenesis (33.6%). Minicucci et al. showed that of 76 children who received cancer treatment, had resulted that 82.9% showed at least one dental abnormality, including tooth agenesis, microdontia, and arrested root development [2]. Kim showed that 55.8% of CCS exhibited at least one dental anomaly [13]. Kaste et al. showed a lower percentage of 39.0% was also observed to have dental abnormalities, and these differences in incidence rates could be attributed to variations in demographic factors, clinical diagnoses, and treatment approaches among the study population [14]. The prevalence of dental abnormalities in permanent teeth in the general population varies from 1.9% to 26.5% [15-17]. Dental anomalies are common even in healthy individuals, and in Korea, the prevalence ranges from 5.7% to 6.6% [18,19]. These figures certainly suggest that children who have experienced cancer therapy have higher tooth formation disorders than those who have not.
In the present study, a young age at cancer diagnosis was identified as a significant risk factor for tooth agenesis and microdontia, while middle age at cancer diagnosis was found to be an important risk factor for root malformation. This finding suggests that dental development can be influenced at any point before the completion of tooth development. In this study, the age divisions of 3 years and 6 years were chosen based on standard reference points for dental development. Calcifications of the first premolars begin between 1.5 - 2 years of age, while the second premolars and second molars start between 2 - 2.5 years and 2.5 - 3 years, respectively [19]. Other permanent teeth begin mineralization within the first year after birth, but the first premolars, second premolars, and second molars start their initial calcification after two years of age. If tooth development is disrupted due to cancer treatment during this critical period, abnormal growth of teeth can occur, leading to conditions such as tooth agenesis or microdontia. Between the ages of 3 and 6, the roots of teeth that initially developed during earlier stages continue to grow, while the crowns of teeth that develop later progress. Therefore, anticancer treatments conducted during this period have a high potential to induce growth abnormalities in both the crown and root of the teeth [20].
When comparing the prevalence of tooth agenesis and microdontia between children under 3 years old and those aged 3 to 6 years old, this study clearly demonstrates a decrease in the occurrence of tooth agenesis and microdontia with increasing age at diagnosis while showing an increasing trend in abnormal root development. A previous study has shown that children who received cancer treatment before age 6 or around 6 at a high risk of dental growth abnormalities due to local or systemic effects that halt the growth of ameloblasts and odontoblasts [20]. On the other hand, other studies have reported that the prevalence of dental growth abnormalities is consistent regardless of the age of cancer diagnosis [21,22]. The differences in these findings may be attributed to variations in treatment protocols and the inclusion of small groups limited to a single diagnosis. Additionally, differences in results could also arise from variations in the timing of tooth formation. Furthermore, the diversity in the timing of tooth formation could be another contributing factor.
Anticancer drugs can also affect the development of permanent teeth. The occurrence of dental abnormalities as a result of cancer treatment is associated with the timing of treatment, the type of medication, dosage, and duration [23]. Disruption of odontogenesis has been reported following the administration of various anticancer agents, including anthracyclines, cyclophosphamide, vincristine, and actinomycin [24]. Furthermore, in other previous studies, through animal experiments, it has been found that the alkylating agent cyclophosphamide is toxic to normal dentinogenesis. This toxicity is attributed to the binding of cyclophosphamide to DNA in the S-phase of mitosis, leading to early apoptosis. The dental effect of cyclophosphamide-induced cell death predominates in primitive mesenchymal cells and preodontoblasts of the pulp [14]. Some chemotherapeutic agents, such as vinblastine and vincristine, can impact mature secretory odontoblasts and ameloblasts. Metalbased agents such as cisplatin and carboplatin can also hinder normal dental development [20]. In previous studies, it has been observed that children exposed to cisplatin exhibited similar toxicities to those induced by other drugs, but specifically caused minor reductions in epithelial and dental pulp stem cells [19,20]. The main side effect of these drugs is that, while they are intended to target and inhibit the division and replication processes of cancer cells, they can also affect normal cells. The dental disturbances that occur after receiving anticancer treatment vary depending on the developmental stage of the affected teeth at the time of treatment. Animal experiments have shown that younger animals are more susceptible to dental effects [2]. Furthermore, it has been reported that the root can be affected even after crown development, leading to root resorption, partial calcification of the pulp chamber, or enamel hypoplasia [25]. In this study, a significant difference in the use of using heavy metal agents is related to tooth agenesis, microdontia and abnormal root development. Also, using multiple class (≥ 4 classes) has a significant difference in tooth agenesis and abnormal root development.
Radiation therapy is often associated with developmental disorders in the body, but the minimum dose of radiation that impairs tooth development remains uncertain [26]. Children who received combined radiation therapy of the head and neck with chemotherapy exhibited more severe dental developmental disorders than children who received chemotherapy alone [27,28]. In previous studies, out of 10 patients who received wholebody radiation therapy combined with chemotherapy, 9 patients exhibited severe dental root abnormalities. In contrast, patients who received chemotherapy alone did not show severe abnormalities [29]. Also, there have been reports of the impact of 4 Gy of radiation therapy on tooth development [3]. Another study indicated that radiation doses of 10 Gy can affect mature ameloblasts, leading to the cessation of tooth development [30]. In this study, when divided based on the median dose of 40 Gy, no significant difference was observed in dental abnormalities.
According to HSCT, patients who underwent HSCT demonstrated a statistically higher prevalence of abnormal root development than groups who only got the chemotherapy. This suggests that HSCT may impact the occurrence and severity of dental anomalies. In this study, when we combine RT and HSCT with chemotherapy, there are significant differences in dental abnormalities.
The most common dental developmental abnormality observed in this research was microdontia (43.2%). The prevalence of microdontia in pediatric cancer patients ranges from 4% to 78% [2,31,32]. In this study, the maxillary second molar was the most affected tooth by microdontia, followed by the maxillary second premolar and mandibular second molar. Another study indicated that the maxillary first premolar was the most commonly affected, followed by the maxillary second molar [2].
The next most common dental abnormality was root abnormality (39.2%), and the most common root abnormality observed was V-shaped roots. Altered odontoblastic activity, as a consequence of the abnormal secretory function of microtubules and complete changes in interand intracellular relationships, can lead to the development of short, thin, and blunt roots [19]. These variations may be attributed to the differences in the age of cancer diagnosis.
Tooth agenesis was observed in 33.6% of the cases. The most affected tooth was the lower second premolar, followed by the upper second premolar. This was the same order as in the case of children who received chemotherapy in other studies [5]. Also, Jeong et al. reported that the frequency of tooth agenesis in ordinary children was 3.6% [33].
Overall, among the 125 CCS, excluding the 41 patients without any dental abnormalities, the most frequently observed dental abnormalities were a combination of tooth agenesis, microdontia, and abnormal root development. Another study stated that patients with agenesis teeth were, in general, were more likely to present with smaller teeth, particularly in the posterior regions, which might suggest a correlation between the occurrence of microdontia and tooth agenesis [6]. This suggests that dental abnormalities can manifest not only as single anomalies but also in combination, highlighting the importance for pediatric dentists to carefully examine and consider these multiple abnormalities.
Overall, among the 125 CCS, excluding the 41 patients without any dental abnormalities, the most frequently observed dental abnormalities were a combination of tooth agenesis, microdontia, and abnormal root development. Another study stated that patients with agenesis teeth were, in general, were more likely to present with smaller teeth, particularly in the posterior regions, which might suggest a correlation between the occurrence of microdontia and tooth agenesis [6]. This suggests that dental abnormalities can manifest not only as single anomalies but also in combination, highlighting the importance for pediatric dentists to carefully examine and consider these multiple abnormalities.
This study also has certain limitations. Firstly, it relied solely on retrospective assessment through radiographic images, which limited the availability of clinical data. Consequently, it was not possible to assess specific measurements related to dental anomalies such as enamel hypoplasia, caries detection, or the extent of caries. Furthermore, since each patient may have undergone different types and durations of cancer treatment, it was challenging to fully understand the dental effects specifically attributed to each anticancer therapy. Lastly, this study exclusively examined dental developmental abnormalities within CCS. A direct comparison was not made with healthy individuals who did not undergo cancer treatment. The prevalence of dental developmental disorders in healthy subjects was established through reference to prior research. Therefore, future studies encompassing a comparison with healthy children would enhance the comprehensiveness of the analysis.
Finally, before treating CCS, it is the pediatric dentist’ s duty to gather accurate and detailed information about the patient’s medical history. This includes closely examining the treatment duration, treatment process, and timing, and understanding the various dental abnormalities that may manifest in the patient. In cases where dental anomalies are present, careful maintenance and appropriate restorative treatments should be considered. If the patients start cancer treatment at a young age, explaining to the parents the potential for tooth agenesis, microdontia, and root abnormalities in permanent teeth is essential. Additionally, it is crucial to provide the necessary explanations regarding permanent dentition. If the patient still retains the primary dentition and exhibits tooth agenesis in the permanent dentition, restorative management or orthodontic treatment of the primary dentition are crucial. In cases involving microdontia, evaluating the size and condition of the teeth is imperative to determine the necessity of orthodontic or prosthetic treatment [34]. Removable prosthetic management is presently the preferred approach for tooth agenesis [35]. Lastly, if abnormalities are detected in the roots, regular clinical and radiographic evaluations are indispensable, and if the patient complains of tooth pain or experiences the occurrence of fistula, pulp treatment may be necessary [36]. Overall, treatment plans involving conservative management and considerations such as space maintenance will be essential.
Conclusion
68.0% of childhood cancer survivors exhibited at least one dental abnormality. The types of abnormalities varied depending on the age at cancer diagnosis and treatment intensity, ranging from microdontia (43.2%) to abnormal root development (39.2%) and tooth agenesis (33.6%). Young age (under 6), the use of heavy metal agents, a history of HSCT, and the combined treatment of RT and HSCT are important risk factors for overall dental abnormalities. The importance of this study lies in the fact that pediatric dentists should be aware of dental anomalies among childhood cancer survivors and that it provides information that can assist pediatric dentists in early detection, prevention, and timely intervention.
Acknowledgements
This research was funded by the Yonsei University College of Dentistry Fund (6-2023-0014).
Notes
Conflict of Interest
The authors have no potential conflicts of interest to disclose.
Funding information
This research was funded by the Yonsei University College of Dentistry Fund (6-2023-0014).





