저한성 외배엽 이형성증을 가진 소아 환자에서 의치 유지력 향상을 위한 보철 치료 전략: 두 가지 증례 보고
Prosthetic Treatment Strategies for Improving Denture Retention in Pediatric Patients with Hypohidrotic Ectodermal Dysplasia: a Report of Two Cases
Article information
Abstract
이 논문은 저한성 외배엽 이형성증(Hypohidrotic Ectodermal Dysplasia, HED)으로 인한 부분무치증을 가진 소아 환자에게 의치의 유지력 증가 방법에 관한 두 가지 증례를 보고한다. 두 환자 모두 다수의 치아 결손 및 원추형의 견치와 치조골 위축, 골격적 III급 경향이 나타났다. 첫 번째 증례에서는, 변형된 형태의 Conical-Crown Retained Denture (CCRD)를 이용해 견치를 피개하였다. 이 방법은 치아를 삭제하거나 코핑 없이 진행되었다. 두 번째 증례에서는, 심한 치조제 흡수와 함께 하악 좌측 견치가 원심으로 경사지어 맹출한 상황에서, 하이브리드 세라믹 크라운을 사용하여 견치를 수복한 후, 흡착성 원리를 이용한 클라스프 유지 가철식 의치로 변경하였다. 두 환자는 현재 보철물 유지 관리 및 성장양상을 평가하기 위해 주기적으로 치료를 받고 있다. 이 증례는 HED로 인하여 의치의 유지력이 부족한 소아 환자에게 적용된 창의적인 보철 치료 방법을 제시하였다.
Trans Abstract
This report presents two cases concerning strategies for improving denture retention in pediatric patients with oligodontia caused by hypohidrotic ectodermal dysplasia (HED). Both patients presented with multiple missing teeth, conical canines, alveolar bone atrophy, and a skeletal Class III tendency. In the first case, a modified form of conical-crown-retained denture was used to cover the canines. This approach was carried out without tooth extraction or coping. In the second case of severe alveolar bone resorption and a distally tilted lower left canine, the tooth was restored with a hybrid ceramic crown. It was subsequently converted into a clasp-retained removable partial denture, utilizing a suction mechanism. Both patients are currently receiving regular check-ups for the maintenance of their prosthetic appliances and the evaluation of their growth patterns. This study presents innovative prosthetic treatment methods for pediatric patients with HED who have inadequate denture retention.
Introduction
Ectodermal dysplasia (ED) is a hereditary disorder that causes dysplasia in two or more tissues derived from the ectoderm, including skin, hair, nails, teeth, and sweat glands. It has 170 different syndromic types and can be categorized into two main types, hypohidrotic and hidrotic, based on whether or not there are sweating disorders [1]. Hypohidrotic ectodermal dysplasia (HED) is expressed in men, and its characteristic facial features include a protruding forehead, a small saddle nose, depressed cheeks, an underdeveloped zygoma, and hyperpigmentation of the skin around the eyes and mouth. The skin is wrinkled and dry due to dyshidrosis [2]. The primary oral characteristics include anodontia or oligodontia, cone-shaped dental abnormalities, enamel hypoplasia, decreased height of the alveolar ridge, vertical dimension loss, and a high palate [3,4]. Anodontia or oligodontia can lead to masticatory dysfunction, nutritional imbalance, and articulation disorders. Malocclusion can also result in dissatisfaction with one’s appearance [5].
Therefore, prosthetic treatment for pediatric HED patients should focus on alveolar ridge preservation, early habit corrections for mastication, swallowing, and pronunciation, and aesthetic enhancement [6]. Utilizing removable complete or partial dentures and fixed prostheses is common in the prosthetic treatment of HED [7]. Early prosthesis use not only mitigates side effects like alveolar ridge resorption, vertical dimension loss, and skeletal class III malocclusion but also enhances functional aspects like mastication, language development, and patient self-esteem. It is generally known that dentures can be worn at around 3 years of age [8-10]. Mastication, esthetics, and pronunciation are corrected through long-term, regular dental visits, and a final restoration is performed using implants or dentures when the bone growth is complete [11].
Pediatric patients with HED have reduced tissue support due to an anatomically small mandible and an atrophied alveolar ridge, as well as reduced denture retention owing to the loss of support resulting from oligodontia [12]. Additionally, given the significant changes in maxilla and mandible growth that cause discomfort and frequent denture replacement in pediatric patients, their prosthetic treatment necessitates a multidisciplinary approach.
This report presents two cases of pediatric HED patients with oligodontia, an atrophied alveolar ridge, and conical central incisors and canines. Prosthetic methods improving denture retention were applied, yielding satisfactory results and increased dental retention observed at regular checkups.
Case Reports
1. Case 1
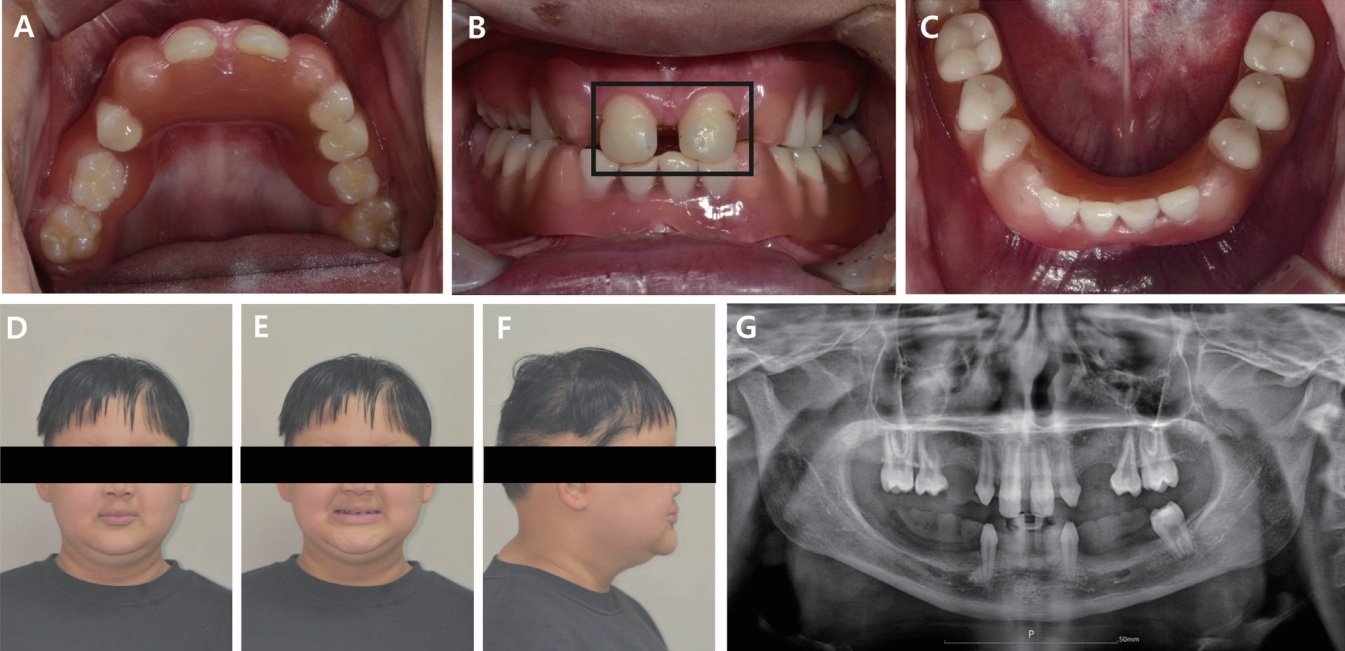
A 5-year-old boy with HED visited the clinic, representing multiple dental anomalies as the chief complaint. Based on family history, there were no relatives who had the same symptoms as the patient. Intraoral and panoramic radiographic examination showed only eight erupted primary teeth (upper primary 2nd molars, upper primary canines, upper primary central incisors, and lower primary canines) and five unerupted permanent teeth in the bone (upper 1st molars, upper central incisors, and lower left 1st molar). The upper primary central incisors and primary canines were conical, the lower primary canines were conical, and the upper primary 2nd molars showed abnormal crown morphology. Developmental disturbances of the mandible and edentulous ridge due to the loss of 51, 52, 54, 55, 61, 62, 64, and 65 teeth were observed (Fig. 1A - 1D). The patient’s clinical examination was consistent with the physiognomic features of ED, with protruding mentum and lips, sparse and thin hair, a flat mandibular plane, and reduced lower anterior face height (Fig. 1E - 1G). The lateral cephalogram revealed skeletal class III malocclusion (Fig. 1H) [13]. Prior to treatment planning, the patient and caregivers were informed of matters regarding this report’s publication and confidentiality, and signed written consent was obtained.

5-year-old pediatric patient with hypohidrotic ectodermal dysplasia. (A) Maxillary occlusal view, (B) Frontal view, (C) Mandibular occlusal view, (D) Panoramic radiograph, (E - G) Extraoral photograph, (H) lateral cephalometric radiograph and analysis.
A flexible denture was fabricated using Valplast® (Valplast, New York, USA) and was installed orally to recover masticatory function and vertical dimension as the first treatment after the initial meeting (Fig. 2). However, the patient returned 2 days later, complaining of instability and frequent displacement of the mandibular denture. Considering the patient’s request to correct severe lower alveolar ridge resorption and denture retention, refabrication of the mandibular denture was planned. In consultation with the department of prosthetics, the conical lower primary canines were utilized to enable better retention of the alveolar ridge, and restoration using a modified form of a conical-crown-retained denture CCRD) without tooth extraction or coping was planned.

Intraoral view after flexible denture delivery. (A) Maxillary occlusal view, (B) Frontal view, (C) Mandibular occlusal view.
First, a preliminary impression was obtained using irreversible hydrocolloid (Alginoplast®, Cavex Holland BV, Haarlem, The Netherlands) on the day of the visit, and a wax rim and recording base of the jaw relationship were produced based on this impression. At the next visit, the vertical dimension and centric relation were obtained using the wax rim (Fig. 3A - 3C), and the maxillomandibular impression was made using polyvinylsiloxane (Honigum Mono, Light body, DMG, Hamburg, Germany). Occlusion was measured with the contact points of the canines as the reference. The articulator was elevated based on the formed rim and bite (Fig. 3D), and the flexible dentures were fabricated using the conventional method. The coverage used lower primary canines as abutments for retention enhancement, and two pontics were placed at the 24, 25-tooth area to enhance occlusal force (Fig. 4A). Two weeks later, the pediatric patient initiated using the maxillary and mandibular dentures, and the occlusion and inner surfaces were adjusted (Fig. 4). Regular follow-ups were performed every 3 months.
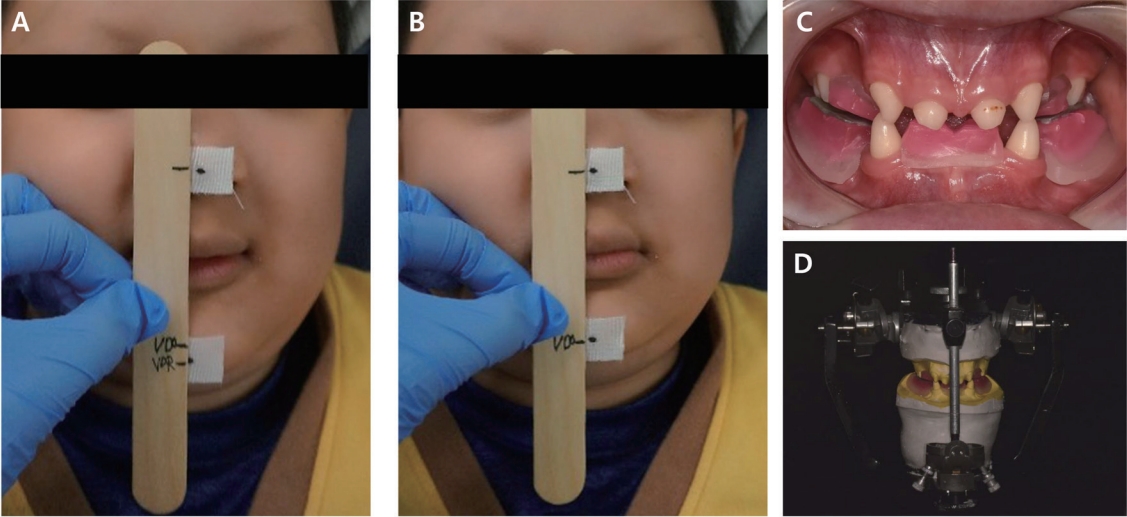
Vertical dimension of occlusion. (A) Vertical dimension at rest, (B) Vertical dimension of occlusion, (C) Wax rim, (D) Elevation of the articulator.

Photograph after upper and lower denture delivery. (A) Maxillary occlusal view showing #24, 25 pontic, (B) Frontal view, (C) Mandibular occlusal view.
After 3 years, the maxillary denture was planned for refabrication owing to the completion of the eruption of permanent teeth (upper 1st molars, upper central incisors, lower left 1st molar) with falling out upper primary central incisors and decreased maxillary denture retention. As the mandibular denture showed good retention, an identical denture, with lower primary canines as abutments, was fabricated. The erupted conical upper central incisors were restored using composite resin (Composite Z350/A2 Restorative; 3M ESPE, Minnesota, USA) to improve the shape of the crowns (Fig. 5B). The mandibular denture was fabricated using the conventional method, and the occlusion of the denture was adjusted to the resin-restored upper central incisors to prevent crossbite (Fig. 5). The patient currently undergoes regular checkups every 3 months, and the dentures have been observed and adjusted for a year.
2. Case 2
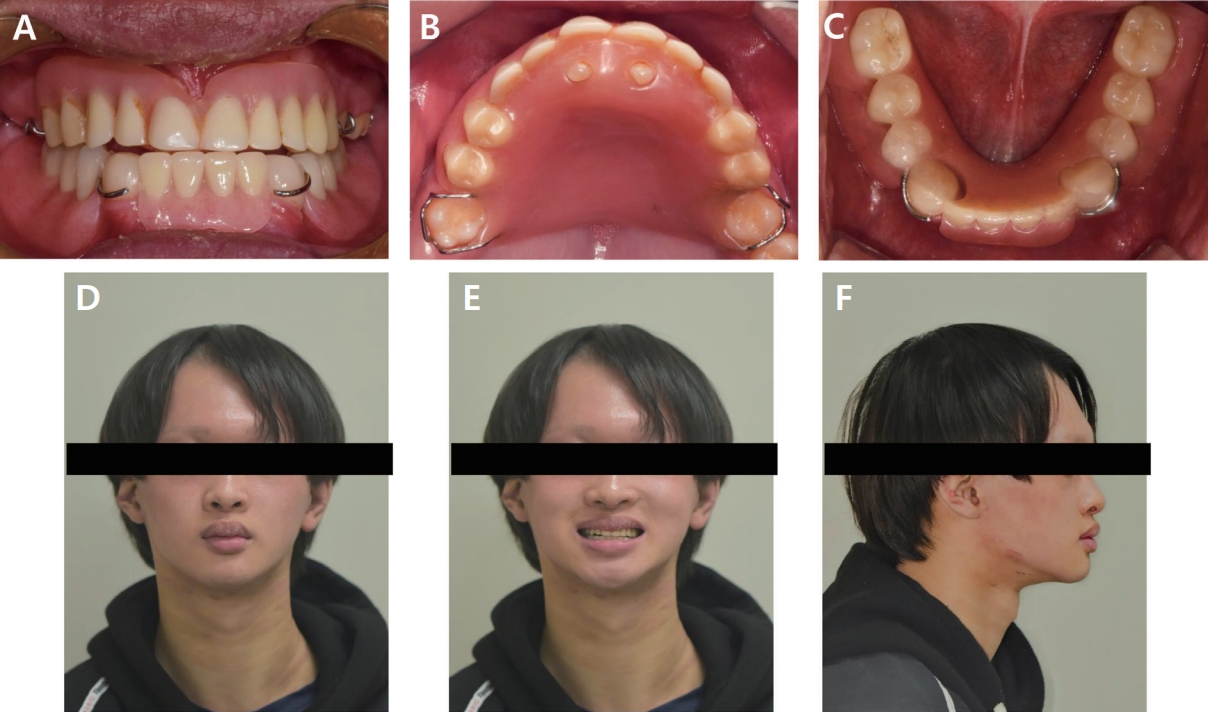
A 12-year-old boy visited the clinic with complaints of discomfort in his maxillary and mandibular dentures since the eruption of permanent teeth. Based on family history, there were no relatives who had the same symptoms as the patient. Clinical examination of the patient was consistent with the physiognomic features of HED, including pale eyebrows, hyperpigmented and dry skin around the eyes, protruded lips, a flat mandibular plane, and reduced lower anterior facial height. Intraoral examination and radiographic image showed that only seven permanent teeth (upper central incisors, upper 1st molars, upper left 2nd molar, and lower canines) were present; the upper central incisors and lower canines were conical; the lower left canine was distally tilted; and the upper 1st molars and left 2nd molar showed abnormal crown morphology. Deficient development of the mandibular and edentulous alveolar ridge due to the V-shaped maxillary arch and the loss of 31, 32, 34, 35, 36, 37, 41, 42, 44, 45, 46, and 47 teeth resulting from the atrophy of the maxillary alveolar ridge in the area with missing teeth were observed (Fig. 6A - 6D). was observed (Fig. 6A - 6D). The lateral cephalogram revealed skeletal class III malocclusion (Fig. 6E) [13]. Prior to treatment planning, the patient and caregivers were informed regarding this report’s publication and confidentiality, and signed written consent was obtained.

12-year-old pediatric patient with hypohidrotic ectodermal dysplasia. (A) Maxillary occlusal view, (B) Frontal view, (C) Mandibular occlusal view, (D) Panoramic radiograph taken while wearing an upper denture, (E) lateral cephalometric radiograph and analysis.
The fabrication of a removable partial denture was planned to improve the patient’s esthetic appearance and masticatory abilities. Due to the skeletal class III mandibular prognathism, there was a possibility of anterior crossbite and a concave facial profile when using conventional maxillary and mandibular dentures. To prevent these, holes for the upper central incisors were made on the palatal surface of the maxillary denture using their conical appearance. Additionally, the upper central and lateral incisor pontics were placed more buccally than the upper central incisors to promote normal occlusion of the anterior teeth and improve the facial profile. The mandibular denture could not be retained with clasps due to the severe undercut of the lower left canine; therefore, a denture that maintained the clasp of the lower right canine but covered the lower left canine was fabricated and applied (Fig. 7).

Photograph after upper and lower denture delivery. (A) Maxillary occlusal view, (B) Frontal view, (C) Mandibular occlusal view.
Three years later, the patient returned to the clinic, indicating that the tilting of the lower left canine (Fig. 8) had made the mandibular denture uncomfortable and lifted its posterior part. The patient desired a denture that was economical, aesthetically pleasing, and demonstrated good retention. Accordingly, a denture using a suction mechanism in the tissue and forming abutments with crown restoration on the remaining mandibular teeth was planned. The crowns were restored using hybrid ceramic blocks (MAZIC Duro, Vericom, Anyang, Korea) for the removal of the undercut on the left mandibular canine and esthetic purposes (Fig. 9A - 9B). Subsequently, the vertical dimension and centric relation were obtained using a wax rim (Fig. 9C - 9E), and the patient underwent functional motion training before getting impressions for denture fabrication. The patient was instructed to move the lips and buccal mucosa, pronounce /u/ and /i/, move the tongue left and right while opening the mouth, and press the inside of the tray with the tongue while closing the mouth, and was instructed to perform these actions when the impression was being taken. Based on the acquired impression, a lower denture with a clasp under the height of the contour of the lower canine crown was created and applied to the patient (Fig. 10). Both the patient and the guardian were satisfied with the esthetics and fit of the denture, and regular checkups every 3 months are currently scheduled.
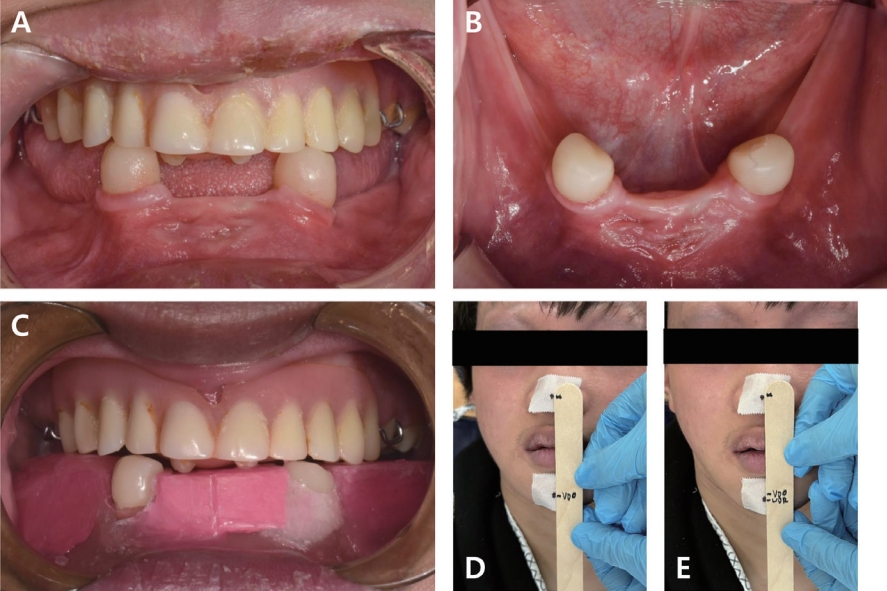
Crown restoration and the vertical dimension of occlusion.
(A) Frontal view, (B) Maxillary occlusal view, (C) Wax rim, (D) Vertical dimension of occlusion, (E) Vertical dimension at rest.
Discussion
In pediatric HED patients with oligodontia, it is advantageous to plan the use of removable overdentures, which utilize the remaining teeth as abutments until bone growth is complete [14]. A study has shown that overdentures for pediatric patients enable vertical dimension increase and ideal occlusion, improving facial form and stimulating alveolar ridges [15]. Moreover, overdentures offer improved stability, retention, and support compared to conventional complete dentures, especially for patients facing challenges with implant restoration due to health conditions or financial constraints [16-21]. And they enhance esthetic satisfaction, notably for patients with oligodontia or other developmental disorders [14]. However, despite these advantages, many dentists hesitate to use overdentures. Concerns include denture thinning due to abutment covering, abutment breakage, functional loss, and the need for frequent replacements of the denture due to alveolar ridge resorption in the posterior edentulous mandible according to age [22-24]. In the reported case 1, the final upper and lower removable dentures were converted to overdentures. In case 2, due to the distal tilt of the permanent mandibular left canine, the initial lower removable denture was also converted to an overdenture.
For case 1, a modified form of CCRD without tooth extraction or coping was planned to use the conical lower primary canines. Conical crowns obtain retention through friction force caused by the wedge effect when a CCRD is inserted and gain an indirect fixation effect from CCRD when there are only a few remaining teeth that are unfavorably positioned [25]. Igarashi reported the results of a 10-year evaluation of 152 patients wearing CCRD, showing good prognoses in Kennedy Classes I, II, and III arches [26]. Conical teeth typically reduce the stability of removable dentures; however, they can be utilized using the aforementioned method to increase denture retention as an abutment of the overdenture. In case 1, As the mandibular overdenture provided excellent maintenance and patient satisfaction, an overdenture was similarly fabricated for the maxilla, designed to cover the maxillary primary canines. The maxillary and mandibular dentures remained in good condition after 1 and 4 years, respectively.
In case 2, a denture was designed to cover the mandibular left permanent canine that had distally erupted. During the 3-year follow-up, the permanent canine did not interfere with the wearing of the overdenture. However, the fit was reduced as the tooth erupted and the distal undercut increased. The pediatric patient requested an affordable and aesthetically pleasing treatment prior to implant restoration. Therefore, the plan included the fabrication of a partial denture with clasp retention following tooth preparation and crown restoration using a hybrid ceramic block (MAZIC Duro, Vericom, Anyang, Korea). MAZIC Duro®, one of the hybrid ceramic blocks, is a nanohybrid ceramic composed of 80% nano ceramic filters (zirconia and silicate) and a 20% resin matrix. It has the advantages of ceramic strength, discoloration resistance, esthetics, and the flexibility and processability of resin matrix [27]. These features allow the product to be used for single crowns as well. It is also economically advantageous because the product’s manufacturing cost is cheaper than conventional zirconia ceramics. In case 2, all undercuts of the lower canines were removed to form the path of insertion, yet the original shape was maintained through minimal crown preparation.
Additionally, to compensate for the severe mandibular alveolar ridge resorption, a suction mechanism was used to enhance retention. The concept of suction refers to denture compression of the alveolar mucous membrane, causing saliva production and generating a negative pressure between the denture and alveolar mucosa, ultimately creating denture retention [28]. Such suction force is effectively exerted when marginal sealing blocks the air inflow. During the precision impression stage, the motion of pronouncing /u/ and /i/ is utilized to create a labiobuccal impression that includes the movement of the buccal frenum. Furthermore, an impression of the oral floor can be made, reflecting the movement of the mylohyoid muscle by utilizing the tongue’s motion of pushing out the lingual tray on the anterior teeth area. Finally, buccal mucosa can move inward through the deglutition movement in the retromolar pad area to form a blockage, and the contraction of this muscle can form a marginal zone in the infralabial area [29]. In the reported case, to reduce patient discomfort from the lifting of the mandibular denture’s posterior part, a suction mechanism was incorporated. This mandibular denture has been maintained well to date, 6 months after its initial use.
A treatment approach for skeletal class III malocclusion is to restore normal arch relationships through orthodontic or surgical procedures [30]. However, if such a treatment is not possible, the functional and esthetic aspects must be restored, while maintaining the current arch relationship in the patient. To this end, prosthetic methods that consider vertical arch movement and reduce anterior crossbite are used [30]. In esthetic terms, the elevation of the vertical dimension of occlusion is required when obtaining the impression in consideration of improvements in the reversed occlusion of the anterior teeth region [31]. In the presented cases, the vertical dimensions were measured to resolve the skeletal class III malocclusion due to HED using a prosthetic method. In particular, to address the severe mandibular prognathism in case 2, the central and lateral incisor pontics were placed more buccally than the natural teeth to enhance the arch’s vertical function and resolve the anterior crossbite. Holes for the conical upper central incisors were made on the palatal area of the denture to establish additional retention.
Recently, fixed treatment methods for the anterior teeth of the mandible have been introduced, providing alternatives to the traditional removable dentures. Ou-Yang et al. used Fixed Partial Dentures (FPDs) to restore multiple missing teeth in 3-year-old ED twins, improving their speech and masticatory function [32]. However, these appliances are required to be removed for monthly cleaning and biannual relining. In another study, Alcan et al. successfully placed anterior mandibular endosseous implants in a 4-year-old patient with HED [33]. Sfeir et al. introduced mini-implant placement. For a 6-yearold anhidrotic ectodermal dysplasia (AED) patient, two mini-implants were placed in the mandibular anterior region to secure removable dentures, and for a 10-yearold ED patient, mini-implants were placed in the maxilla and mandible to replace missing anterior teeth with fixed prostheses [34]. As the mandibular intercanine width stops growing early, dental implants and FPDs in the anterior mandible don’t hinder children’s jaw development [1]. The National Foundation for Ectodermal Dysplasias advises dental implants for children over seven in the anterior mandible [35]. Despite their growing popularity, both FPDs and implants pose potential challenges in pediatric patients, including possible growth hindrance and the need for continuous adjustments. Especially in growing patients, the placement of dental implants carries potential risks such as cessation of growth, implant submersion, or ankylosis [1]. Cronin et al. suggested that implant placement should be planned after the age of 18 for boys and 15 for girls [36].
Pediatric patients with HED exhibit reduced vertical dimensions and abnormal mandibular positions due to growth, which can lead to misfit dentures over time. Therefore, periodic follow-ups are required, and if necessary, a multidisciplinary approach involving pediatric dentistry and prosthetics departments is recommended [37]. Additionally, since hybrid ceramic crowns have a lower strength than conventional zirconia ceramics, their use as a denture abutment must be observed in the long term. Vergo has recommended that the prostheses for growing pediatric patients be relined and rebased every 2 - 4 years and replaced every 4 - 6 years [38]. Both patients will undergo regular checkups every 3 months to assess their growth patterns. Prosthesis adjustment and replacement will be performed accordingly when necessary, and the timing of the implant placement will also be evaluated.
Summary
This report presented two cases to explore methods for enhancing denture retention in pediatric patients with HED. The introduced approach is expected to aid in the prosthetic treatment of pediatric patients with reduced denture retention due to HED, which could contribute to their improved quality of life. However, periodic maintenance of prostheses and evaluation of growth patterns are crucial for securely applying this method to pediatric patients with HED.
Notes
Conflict of Interest
The authors have no potential conflicts of interest to disclose.