Managing Short Root Anomalies in Pediatric Cancer Survivors: Utilizing Resin Wire Splints and Miniscrews for Skeletal Anchorage
Article information
Trans Abstract
Patients with pediatric cancer often undergo multiple therapies, such as chemotherapy, radiation therapy, and stem cell transplantation. These treatments, while essential, can result in dental developmental issues, including hypodontia, microdontia, short roots, and delayed dental development. This report presents two cases of pediatric patients diagnosed with neuroblastoma who exhibited severe tooth mobility due to short roots as a complication of cancer treatment. Moreover, we investigated the conservative management of the patients’ conditions using resin wire splints and orthodontic miniscrews for skeletal anchorage along with long-term follow-ups to evaluate their prognosis.
Introduction
Childhood cancer is a leading cause of pediatric mortality, and the incidence has steadily increased since 1975 [1]. Pediatric malignant tumors primarily occur during the first year of life, with a second peak observed between ages 2 and 3. These tumors include various conditions, such as acute leukemias, malignant lymphomas, encephalomas, neuroblastomas, kidney tumors, and malignant bone cancers. Neuroblastomas and Wilms tumors are more prevalent before the age of 5 years, whereas brain tumors and malignant lymphomas are more common after this age [2]. Neuroblastoma-a malignant tumor of the sympathetic nervous system and the most common extracranial solid tumor in children-originates from embryonic neural crest cells. Recent advancements in treatment strategies for neuroblastoma have resulted in a 5-year survival rate of 82% in children aged < 15 years [3]. Treatment strategies for this malignancy include chemotherapy, radiation therapy (RT), hematopoietic stem cell transplantation (HSCT), and immunotherapy [4]. Meanwhile, dental developmental disturbances caused by these treatments include microdontia, short roots, root shunting, delayed or arrested dental development, enamel hypoplasia, abnormal crown size, and multiple tooth agenesis [5-7]. A previous study reported that the incidence of hypodontia and microdontia was higher in cancer survivors who received anticancer treatment before the age of 4 years [8].
Short root anomalies were typically addressed by extraction, particularly when tooth preservation was challenging because of severe mobility. In such cases, the rehabilitation of oral function was achieved using prosthetic devices such as flexible or implant-supported dentures [9,10]. However, tooth preservation is crucial for pediatric patients receiving anticancer treatment at an early age because alveolar bone resorption can occur after extraction.
This report presents two cases of pediatric patients who were diagnosed with neuroblastoma and exhibited severe tooth mobility due to short roots as a complication of cancer treatment. Moreover, herein, we discuss the conservative management of patients using resin wire splints and orthodontic miniscrews along with long-term follow-ups to evaluate their prognosis.
Case Reports
Each patient provided informed consent prior to participation in and publication of this case report.
1. Case 1
A girl aged 2 years and 10 months was referred to the Department of Pediatric Dentistry, Chonnam National University Hospital, with the complaint of multiple dental caries. Her medical and dental history is presented in Table 1. She was diagnosed with Stage IV neuroblastoma at 15 months of age, which later metastasized to the brain. Further, she received chemotherapy with etoposoide, adriamycin, and cyclophosphamide. Subsequently, a craniotomy and surgical removal of the abdominal tumor were performed. In addition, abdominal RT (total dose, 2,160 cGy) was administered over 2 months at the age of 2 years and 4 months. Further, chemotherapy with thiotepa, melphalan, and total body irradiation (TBI) (total dose, 3,891 cGy) were administered, followed by autologous peripheral blood stem cell transplantation (PBSCT). Then, the patient received immunosuppressant, antifungal, and antiviral agents.
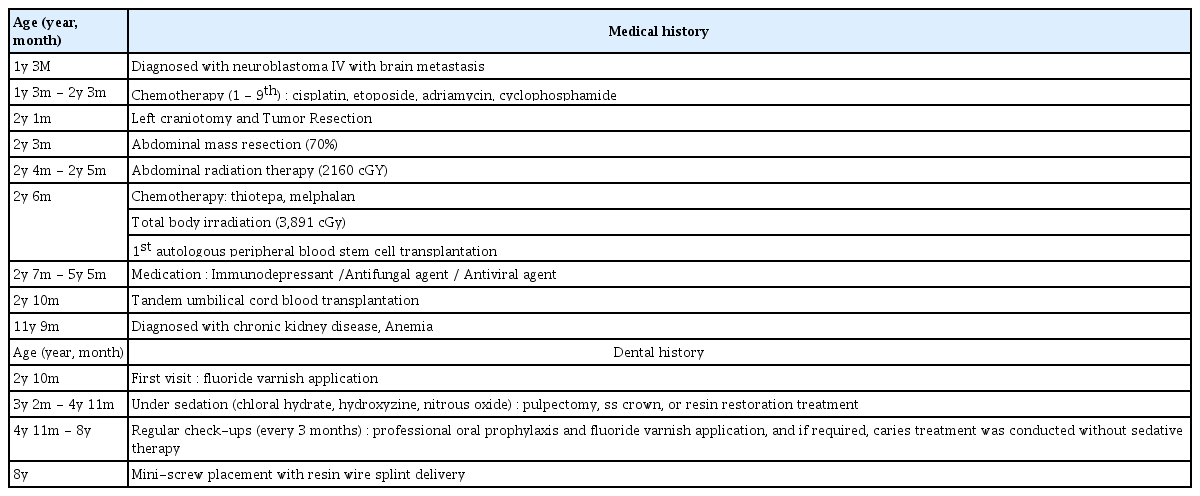
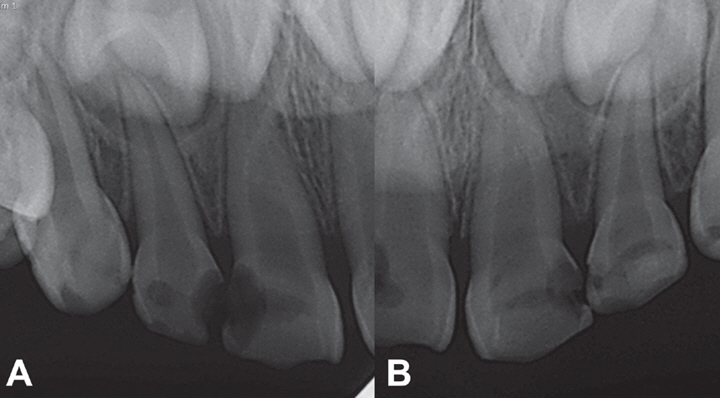
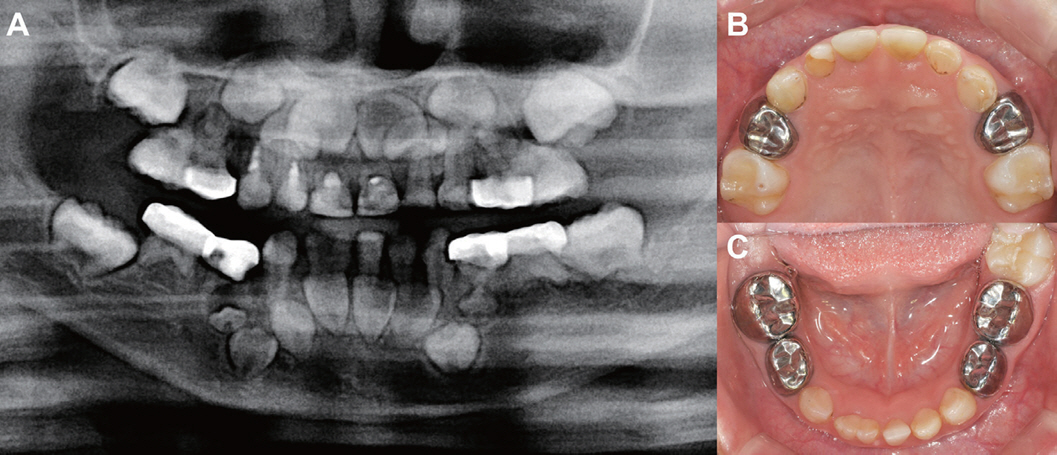
Periapical images taken at the initial visit revealed decalcification changes in the upper primary anterior teeth (Fig. 1). Given that the anticancer treatment was ongoing, fluoride varnish was applied to the teeth to continue the conservative treatment. After 8 months, tandem umbilical cord blood transplantation (UCBT) was performed. Subsequently, after 4 months, with an improved overall health condition, the patient was referred to the pediatric dentistry department for caries treatment. At the time of the visit, the patient was receiving cis-retinoic acid for differentiation therapy, and after consultation with a pediatrician, due to her poor compliance rated as Grade 2 by the Frankl behavioral classification, sedative treatment was planned. The patient received oral administration of 1,000 mg chloral hydrate (Pocral®, Hanlim, Korea) and 21 mg hydroxyzine (Dudrizine®, Sama, Korea), and the concentration of N2O was maintained at 40% during the treatment. The treatment involved Pulp therapy, and restorations were performed under local anesthesia using 2% lidocaine with 1:100,000 epinephrine. Two rounds of treatments were performed under sedation, following which fluoride application and dental examinations were decided to be performed at 3-month intervals. Moreover, restorations were performed as needed during each visit; further, patient cooperation with dental care increased, allowing the treatment to be completed within 1 year and 9 months without sedation (Fig. 2). Fig. 2A revealed the suspected defect of the second premolars, microdontia of the first premolars, and short root of all permanent teeth. Regular check-ups were scheduled every 3 months to manage the eruption of permanent teeth and oral hygiene, which included fluoride application and oral prophylaxis. During routine check-up at the age of 8 years (i.e., in the mixed dentition stage), the patient reported discomfort due to pronounced mobility (Grade 2 by the Grace and Smales mobility index) of her lower permanent incisors. Panoramic radiographs revealed that all permanent teeth had short roots; moreover, there was agenesis of all second premolars and all second molars, as well as microdontia of all first premolars and the upper right second molar (Fig. 3A). At that time, the length of the root of the maxillary anterior teeth was short; however, because the teeth were still erupting, we decided to evaluate the need for tooth stabilization after eruption. The final prosthetic plan was to extract the severely mobile tooth, followed by implant placement, which was scheduled after reaching adulthood (i.e., at the age of 15 years) once growth was completed.
Periapical view at the age of 15 months in case 1. (A, B) Multiple caries were observed in the upper primary anterior teeth.
Panoramic view and intraoral image at the age of 4 years and 11 months in case 1. (A) After endodontic treatment and restoration of multiple teeth, small-sized first premolars were observed, but multiple tooth germ agenesis was suspected, (B) Image after caries treatment in the maxillary teeth, (C) Image after teeth caries treatment in the mandibular teeth (fusion of the right lower central and lateral incisor).
Panoramic radiographs in case 1. (A) Before screw implantation, tooth anomalies including tooth agenesis of the four second premolars, three second molars without right upper second molars, microdontia of the right maxillary second molars and four first premolars (white arrowhead), and short roots in all permanent teeth were observed in all teeth (age, 7 years), (B) Image after 3 months (age, 7 years and 3 months), (C) Image after 5 years (age, 13 years), (D) Image after 8 years (age, 16 years).
Throughout this period, efforts were made to conservatively preserve the teeth as much as possible to maintain the alveolar bone. Accordingly, we decided to place a resin wire splint (RWS) and provide additional skeletal anchorage using miniscrew implantation.
Local anesthesia using 2% lidocaine with 1:100,000 epinephrine was administered. A miniscrew, 1.6 mm in diameter and 7.0 mm in length (Ortholution, Seoul, Korea), was inserted into the attached gingiva between the lower left central and lateral incisors (Fig. 4B). The four lower incisors were then splinted using a 0.017 × 0.025-inch titanium molybdenum alloy (TMA) wire along with the miniscrew and RWS (Fig. 3B). Further, after fixation, the mobility of the lower permanent incisors improved to ≤ Grade 1. To assess alveolar bone resorption and prognosis, the crown-to-root (C/R) ratio was measured using periapical radiographs taken before the procedure (Fig. 5). At the time of screw placement, four lower anterior teeth exhibited an average C/R ratio of 3.3, indicating short roots and severe mobility.
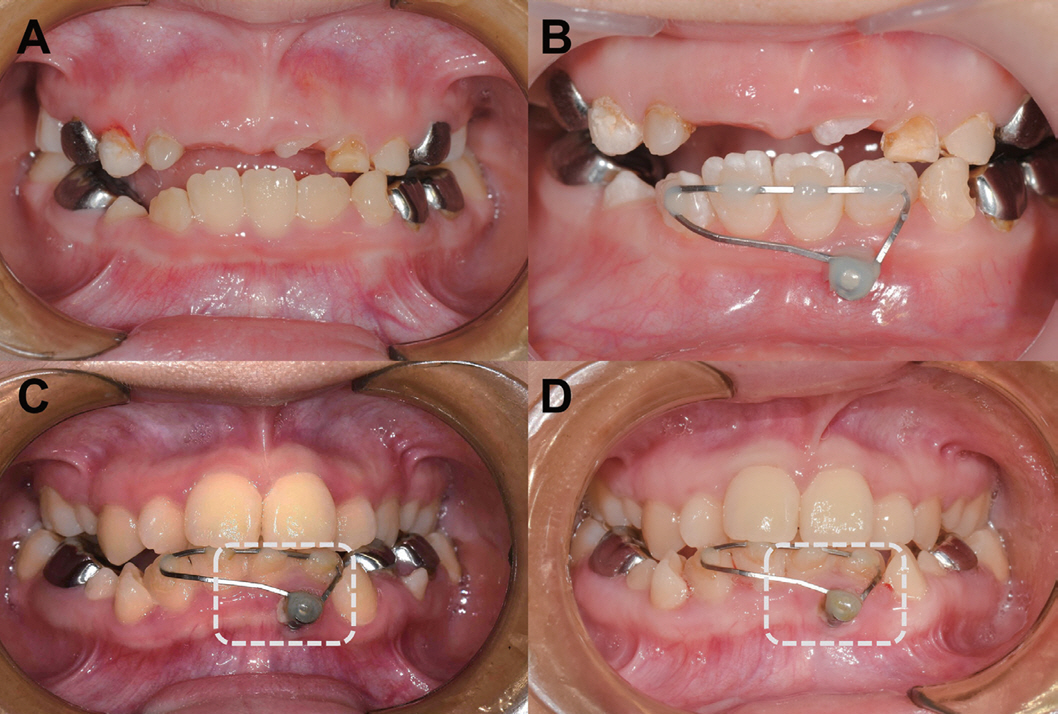
Intraoral photographs of case 1. (A) Image before screw implantation (age, 7 years), (B) Image after 3 months (age, 7 years and 3 months), (C) Image after 5 years (age, 13 years), (D) Image after 8 years (age, 16 years). Gingival tissue overgrowth was observed in the dotted box.
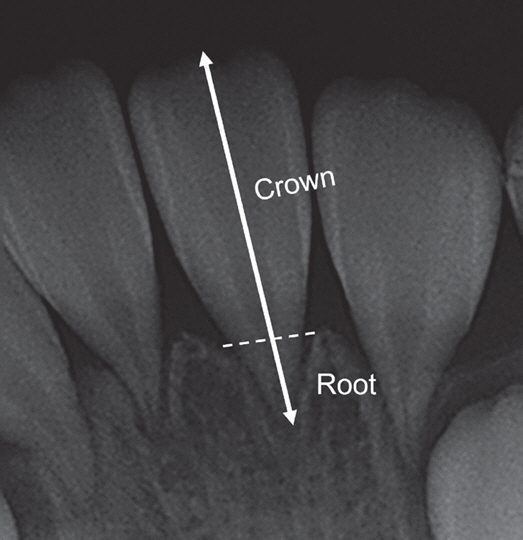
The method of measurement of crown-to-root ratio in both patients. The crown and root lengths were measured using the alveolar bone height (dotted line) as a reference.
Regular check-ups were conducted every 3 months to maintain oral hygiene and manage inflammation around the miniscrew. Moreover, professional oral hygiene care was provided, including fluoride application, oral prophylaxis, and infections related to the screw were assessed.
Panoramic radiographs and intraoral photos were taken during follow-up examinations at 3 months, 5 years, and 8 years after the procedure (Fig. 3, 4). During the regular check-up at 8 years, a periapical view was captured, and the C/R ratio was found to be 3.0, demonstrating stability without increased mobility. However, from the 5-year follow-up onwards, there was excessive growth of the surrounding gingiva (Fig. 4C, 4D). Therefore, consideration was given to exposing the screw head a bit more in the future to facilitate oral hygiene maintenance.
2. Case 2
A boy aged 2 years and 10 months was referred to the Department of Pediatric Dentistry at Chonnam National University Dental Hospital with the complaint of multiple dental caries. Clinical examination revealed carious lesions on all primary molars.
Table 2 presents the medical and dental history of the patient. The patient was diagnosed with Stage IV neuroblastoma, which metastasized to the bone at the age of 22 months. Subsequently, the patient underwent nine cycles of chemotherapy. At the age of 2 years and 5 months, surgery was performed for abdominal tumor removal, followed by an autologous peripheral blood stem cell transplantation.
We planned to proceed with restoration under the sedative treatment due to the patient’s poor compliance rated as Grade 2 by the Frankl behavioral classification. However, because the second PBSCT was scheduled after 1 month, we planned to complete the dental caries treatment within 2 weeks. After consultation with a pediatrician, 940 mg of chloral hydrate (Pocral®, Hanlim, Korea) and 18 mg of hydroxyzine (Dudrizine®, Sama, Korea) were administered orally, and the N2O concentration was maintained at 40% during treatment. The treatment involved stainless steel (SS) crown and resin restorations, which were performed under local anesthesia using 2% lidocaine with 1:100,000 epinephrine. After one month, he underwent a second PBSCT. Moreover, he received a total body radiation dose of 1,500 cGy during his cancer treatment. After receiving anticancer treatment, intravenous immunoglobulin (IVIG) and interleukin-2 were administered to supplement the weakened immune system. After completing the anticancer treatment and recovering his overall health, the patient revisited the dental clinic after 2 years and 8 months with the chief complaint of multiple dental caries. The radiograph revealed multiple caries with the suspected defect of the second premolars, and the first premolars exhibited microdontia (Fig. 6).

Periapical view of case 2 at the age of 5 years and 6 months. (A-E) Multiple caries, small-sized first premolars, and suspected defects in the second premolars were observed.
Five cycles of N2O sedation were administered, and then endodontic and restoration treatments were performed. The patient was scheduled to undergo regular check-ups every 3 months for oral hygiene maintenance and fluoride application by a specialized dental hygienist. He was diagnosed with Stage IV chronic kidney disease at the age of 3 years and 5 months. This led to the diagnosis of a growth delay at the age of 6 years. At that time, both the height and weight of the patient were below 3%, prompting the initiation of growth hormone therapy.
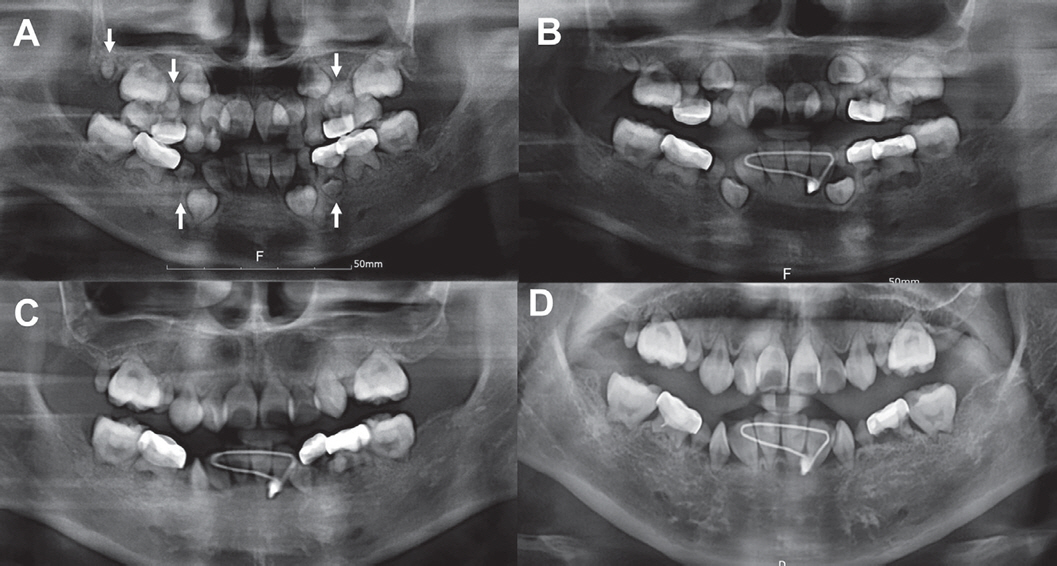
At 8 years and 9 months of age, during a routine checkup, the patient was found to have transitioned to the mixed dentition stage. All permanent teeth exhibited short root development, and lower anterior teeth showed mobility, agenesis of all second premolars and molars, maxillary right first premolar, short roots in all permanent teeth, and 3 microdontia of the first premolar without upper right (Fig. 7A).

Panoramic radiographs of case 2. (A) Before screw implantation, tooth anomalies including tooth agenesis of the four second premolars, the four second molars, and the left maxillary first premolar, microdontia of the three first premolars without the left maxillary first premolar (white arrow), and short roots in all permanent teeth were observed (age, 8 years and 9 months), (B) Image after 3 years (age, 12 years and 1 month).
The C/R ratio was measured using the periapical radiograph images taken before and 3 years after the procedure. Three lower anterior teeth without the right lower lateral incisor had an average C/R ratio of 4.0, indicating very short roots, and exhibited Grade 2 mobility. Notably, the right lower lateral incisor was in the process of eruption (Fig. 8A). To improve the stability of the lower anterior teeth, a plan was made to deliver a RWS using a miniscrew. Moreover, local anesthesia with 2% lidocaine with 1:100,000 epinephrine was administered to the vestibular area between the lower central incisors. Further, a miniscrew, 1.6 mm in diameter and 7.0 mm in length (Ortholution, Seoul, Korea), was inserted. Three lower incisors were splinted using a 0.017 × 0.025-inch TMA wire along with the miniscrew and RWS (Fig. 7B, 8B). Moreover, to facilitate eruption, the lower right lateral incisor was not initially included in the splint, but later, it was considered for inclusion in the appliance. After splinting, tooth mobility was reduced to ≤ Grade 1. After 3 years of follow-up, there was no increase in mobility, indicating stability, with a C/R ratio of 4.2 on the periapical view. Further, regular check-ups were conducted every 3 months to maintain oral hygiene and manage inflammation around the miniscrews, and professional oral hygiene care was provided, including fluoride application, and infections related to the screws were monitored.

Intraoral photographs of case 2. (A) Image before screw implantation (age, 8 years and 9 months), (B) Image after operation, (C) Image after 3 months (age, 9 years and 3 months). The dotted line indicates a mucogingival junction.
In case 2, the goal was to extract teeth with severe mobility after the age of 19 and place implants. Further, considering the eruption of maxillary incisors, discussions were planned for assessing the stability of mobility at a later stage.
Discussion
Neuroblastoma is one of the most common malignant tumors in children and originates from primitive nervous system cells, with an average age at diagnosis of 17 months [11,12]. The first phase of tooth development begins around the 6th week of gestation, whereas tooth root development continues until approximately 3 years of age. Permanent dental crowns form over a period of approximately 12 years. Meanwhile, the development of the roots of all teeth, except the third molars, begins at approximately 3 - 4 years of age and continues until the age of 16 years [13]. The diagnosis of neuroblastoma often coincides with critical dental development phases. Moreover, common neuroblastoma treatments, such as RT, chemotherapy, and HSCT, can markedly impact dental development [6]. RT with high-dose radiation exposure during early tooth development stages, including the tooth germ phase, can lead to incomplete tooth formation [5]. In subsequent growth stages, even lower radiation doses can cause dental abnormalities, including microdontia, short roots, enamel hypoplasia, delayed tooth development, and root resorption [14]. Chemotherapy acts via various mechanisms, such as inhibition of cell division or destruction of DNA or RNA in cells. These treatments can lead to dental abnormalities such as delayed tooth development, dental agenesis, microdontia, supernumerary teeth, and short roots [15]. HSCT involves administering healthy hematopoietic stem cells to patients with dysfunctional or depleted bone marrow. In general, the younger the patient at the time of HSCT, the higher the chance of agenesis or microdontia [5,16].
The two cases presented in this report were diagnosed with Stage IV neuroblastoma before the age of 3 years, and they received TBI doses of 3,891 and 1,500 cGy, respectively. Moreover, chemotherapy was administered, and HSCT was provided as part of the treatment before the age of 4 years. Regarding long-term complications, both cases 1 and 2 exhibited dental abnormalities, including the absence of seven or nine teeth, microdontia in five or three teeth, and short roots in all permanent teeth.
In a previous study, dental anomalies, including short root teeth, were observed in a 12-year-old boy who had undergone anticancer treatment for neuroblastoma. Teeth with mobility were extracted, and implant-supported overdentures were fabricated [9]. However, when placing implants in growing children, the implant may submerge compared with the vertical growth of the adjacent alveolar bone, which could pose challenges to occlusion and hygiene management [17]. Craniofacial growth is completed at ages 13 - 15 for females and 17 - 25 for males [18]. Therefore, in these cases, the final prosthetic plan involved extracting mobile teeth and proceeding with implant placement after this age.
Various methods have been introduced to stabilize teeth with severe mobility. First, a removable splint made from polycarboxylate and polyacrylic can be used, primarily within a short period (4 - 8 weeks) for traumatized teeth [19]. Another method is the use of a fixed periodontal splint. Various types of splints are available, such as light-cured resin or materials like wire, fiber, and titanium [20]. The most commonly used splint among these types is RWS. For enhanced flexibility, it is generally recommended to use orthodontic wires with a thickness of < 0.018 inch, such as twistflex wire, or those with a thickness of 0.4 - 0.5-mm, allowing physiological movement while preventing complications such as ankylosis [21]. However, in the present report, rectangular 0.017 × 0.025-inch wire was used, because the length of the root is very short, necessitating a more rigid fixation. Additionally, while SS wire is commonly used for rigidity, it can lead to increased production of free radicals and potential cytotoxicity, making it less suitable for long-term use in cancer survivors [22]. In contrast, TMA materials, characterized by an inert TiO2-based film on their wire surface, were chosen due to their excellent biocompatibility [23,24].
However, one of the limitations of this technique is that RWS is primarily intended for short-term stabilization of mobile teeth, especially in pediatric cases, but long-term use, particularly in growing children with erupting teeth, may disrupt the physiological eruption process when the device is attached to erupting teeth. Similarly, in case 2, the teeth were not connected to RWS to allow for the eruption of the lower right lateral incisors. In the future, once a complete eruption occurs, the possibility of modifying the RWS design will be considered, taking into account the assessment of mobility. Additionally, orthodontic miniscrews were chosen in both cases due to the short length of the adjacent tooth root, requiring extra anchorage.
Miniscrews offer several advantages, including costeffectiveness, easy placement and removal, small and versatile size for various anatomical regions, excellent stress distribution to the surrounding bone tissues, resistance to orthodontic forces, and minimal surgical trauma [25-27]. However, when treating pediatric cancer survivors, it is essential to be mindful of the potential adverse effects and risks of complications associated with miniscrew placement. Miniscrews are made from the same materials as implants and are sometimes referred to as mini-implants. There are important considerations when determining implant placement for patients with a history of cancer. The first consideration is to delay surgical procedures if the patient’s platelet count is ≤ 100,000/mm3. Furthermore, a history of radiation exposure ≥ 66 Gy to the head and neck may pose a risk of radiationinduced osteonecrosis after implant placement [28]. Although there is a shortage of research on the long-term use of miniscrews, it remains critical to select suitable patients for miniscrew placement based on their medical history and condition. The two patients had completed anticancer treatments, including chemotherapy and RT, before 3 and 4 years, respectively, and were not receiving any medications at the time of miniscrew implantation.
Several factors should be considered when implanting a miniscrew. The first is the implantation site. When the implantation site is in close contact with the root, it can lead to loss of tooth vitality, root fractures, and loss of dental sensation. Also, placing miniscrews in the nonkeratinized tissue may exert pressure on the surrounding tissues, potentially causing tissue overgrowth [29]. In case 2, due to the short length of the attached gingiva, the miniscrew was positioned in the alveolar mucosa to prevent it from getting too close to the tooth root. Should there be an excessive growth of soft tissue, the plan involves removing the excess tissue and, in the future, relocating the miniscrew based on the expansion of the attached gingiva as the alveolar bone growth.
The second consideration is the miniscrew diameter. To minimize minor bone damage, it’s advisable to use a 1.5- or 1.6-mm-diameter miniscrew, with a preference for the latter in these cases [30,31]. If the diameter is too small, there is a risk of screw loosening or detachment [32]. However, in both cases, miniscrews were employed for tooth maintenance rather than applying orthodontic forces, thus minimizing related risks.
Even after implantation, thorough oral hygiene management and inflammation control are crucial, with the removal of the screw being considered in patients with suspected infections. If there is local irritation, it is common to use 0.2% chlorhexidine to manage local inflammation. However, it is essential to exercise caution when dealing with patients who have inadequate oral hygiene management. In particular, because a wire is connected around the miniscrew neck, there is a risk of tissue damage and plaque deposition [33]. To prevent this, exposing the miniscrew head as much as possible can be beneficial [34]. For case 1, although the miniscrew was initially placed in the attached gingiva, over a five-year observation period, excessive tissue growth in the surrounding area was noted. Therefore, consideration should be given to exposing the miniscrew head a bit more to facilitate oral hygiene maintenance.
In both cases, despite C/R ratios significantly lower than the normal 0.5 [25], follow-up exams at 8 and 3 years, respectively, showed miniscrews effectively reduced tooth mobility. This report suggests that the utilization of miniscrews and RWS may offer benefits not only to pediatric cancer survivors but also to those with short dental roots by enabling the preservation of teeth.
Summary
This case report presented two cases of pediatric patients with short tooth roots as complications of multimodal therapies for malignant tumors. The mobile lower permanent incisors were stabilized using RWS with miniscrews at the ages of 8 years and 8 years 9 months, respectively, and extensive long-term follow-up was conducted. This approach of preserving the teeth and reducing mobility instead of extracting them was found to have favorable results for both patients and their caregivers. Moreover, both cases exhibited favorable long-term outcomes. Therefore, this approach represents a viable treatment option for lower permanent incisors that are severely mobile because of dental root developmental abnormalities.
Notes
Conflict of Interest
The authors have no potential conflicts of interest to disclose.