제2유구치의 일차성 만기잔존이 동반된 제1대구치 수평매복의 맹출유도 : 증례보고
Eruption Guidance of Horizontally Impacted Permanent First Molar with Primary Retention of Primary Second Molars: Case Reports
Article information
Abstract
치아 맹출은 치조골을 통해 치낭의 위치로부터 구강 내의 최종적인 교합 위치까지 치아가 이동해가는 복잡한 발육 과정이다. 치아의 맹출 장애는 맹출 일련의 단계 중 어느 단계에서도 일어날 수 있으며, 하악 제2유구치의 일차성 만기잔존과 하악 제1대구치의 수평매복이 동시에 발생한 증례는 매우 드물다.
이번 연구의 목적은 제2유구치의 일차성 만기잔존이 동반된 하악 제1대구치의 수평매복의 두 증례에 대한 치료를 제시하는 것이다. 일차성 만기잔존으로 맹출 지연된 하악 제2유구치는 발치하였고, 수평매복된 하악 제1대구치는 교정적 견인을 시행하였다. 이후 계승 소구치의 맹출 공간을 위해 공간획득을 도모하였고 계승 소구치의 변위가 개선되었으며 제1대구치는 정상적인 맹출이 유도되었다.
Trans Abstract
Tooth eruption involves a complex developmental process of tooth migration from the dental follicular origin to the final occlusion position in the oral cavity via the alveolar process. Disturbance of tooth eruption can occur at any point in a series of eruption stages; however, horizontal impaction of the mandibular first molar and primary retention of the primary mandibular second molar are rarely observed simultaneously. This study describes the treatment for two cases of horizontally impacted first molar with primary retention of primary molar. The primary retention of the primary mandibular second molar was extracted, and orthodontic traction was applied to the horizontally impacted primary mandibular first molar. Subsequently, displacement of the premolar tooth bud was improved and space regaining for eruption was achieved, guiding to normal eruption of the first molar.
Ⅰ. Introduction
Tooth eruption occurs via a multifactorial developmental process of tooth migration from its origin in the dental follicle to the final occlusion position in the oral cavity via the alveolar process[1]; however, the underlying biological mechanism for tooth eruption remains unclear. The process progresses through pre-eruptive, pre-functional eruptive, and functional eruptive phases. Tooth eruption can be disturbed by systemic[2-4] and local factors[5]. Several syndromes and systemic diseases in various systemic factors can affect normal multiple teeth. In addition, local factors that cause eruption disturbances affecting one or more teeth include abnormal eruption paths, tooth anomalies, supernumerary teeth, odontoma, tooth bud displacement by a cyst and tumor, prolonged retention or premature exfoliation of primary teeth, ankylosis, loss of eruption space, gingival fibrosis, cleft palate, and idiopathic conditions with unknown causes.
Eruption disturbance can occur at any point in the series of eruption stages. Raghoebar et al .[6] classified eruption disturbances as impaction, primary retention, and secondary retention, depending on the cause. Impaction is the cessation of tooth eruption caused by a detectable physical barrier in the eruption path or abnormal directionality of the tooth. Secondary retention refers to the cessation of eruption of a tooth after emergence without a physical barrier in the eruption path and not due to an abnormal position.
Primary retention refers to the cessation of eruption before emergence without a physical barrier in the eruption path and not due to an abnormal position. The tooth shows a normal eruption path from a radiograph. Primary retention is likely caused by a disturbance in the dental follicle, which fails to initiate metabolic events responsible for bone resorption in the eruption path. In the case of a permanent tooth, if eruption is delayed for more than 2 years, primary retention is suspected[6].
Primary retention of a primary molar can lead to numerous problems, including tipping of adjacent teeth, decreased arch length, supra-eruption of the antagonists, tooth bud displacement, damaged occlusal function, cystic change, or infection[7-10]. Especially, primary retention of the second primary molar can seriously impact the development and eruption of the first permanent molar. Such issues can be addressed via regular periodic examination, early extraction inserting a space maintainer, space-regaining followed by surgical extraction and surgical exposure followed by orthodontic traction. Successful treatment depends on the patient’s age and treatment compliance, presence of a succedaneous permanent teeth and the condition of adjacent teeth[10].
First molar plays important roles for mastication in permanent dentition and the formation of vertical occlusion and development of the jaw after mixed dentition. Unlike other permanent teeth, the permanent molar tooth bud develops from the distal extension of the dental lamina without preceding primary teeth[11]. In this case of eruption disturbance of first molar, periodical examination, removal of physical factor and surgical exposure, orthodontic traction, surgical reposition, and tooth replantation can be attempted, and if eruption guidance is not possible, orthodontic or prosthetic treatment can be considered after extraction of first molar[6].
Several studies have described eruption disturbance of primary or permanent molars. However, few have reported horizontally impacted first molar with primary retention of a primary second molar. This study describes proper diagnosis and treatment for two cases of horizontally impacted mandibular first molar with primary retention of the primary mandibular second molar in patients referred to the Department of Pediatric Dentistry, College of Dentistry, Chosun University.
Ⅱ. Case reports
1. Case 1
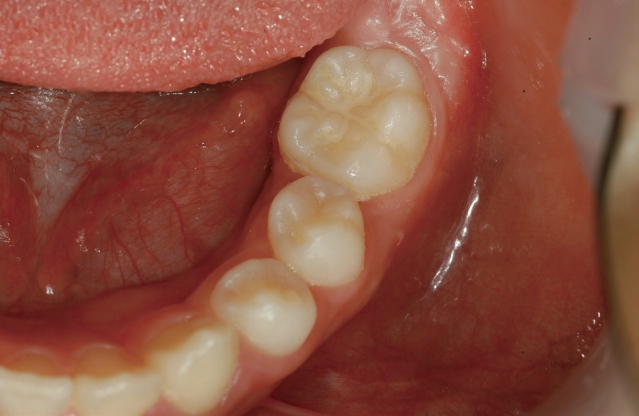
A 6-year-old girl with no eruption of the primary mandibular left second molar was referred to the Department of Pediatric Dentistry, College of Dentistry, Chosun University. Clinical findings indicated an unerupted primary mandibular left second molar (Fig. 1).
First visit. Primary second molar in the left mandible were not observed on an intraoral photograph.
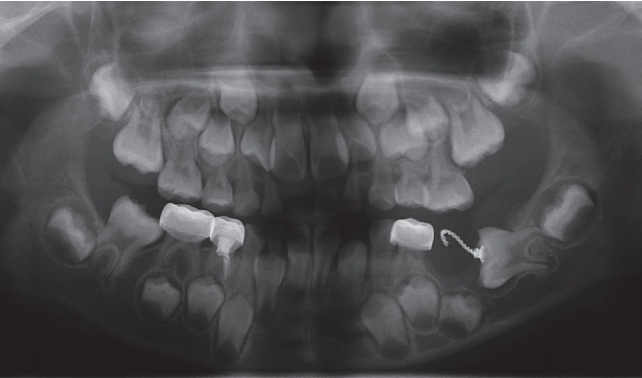
Panoramic radiograph revealed primary retention of the primary mandibular left second molar and showed lower displacement of the premolar tooth bud (Fig. 2). The mandibular left first molar was horizontally impacted, showing root development at Nolla stage 7(one-third of the root completed), and was locked with the primary mandibular left second molar. In addition, the mandibular right first molar was locked with the primary mandibular right second molar. The oral examination revealed no relevant familial or medical history. Computed tomography(CT) imaging showed loss of periodontal ligaments of the primary mandibular second molar, thus, being suspected of ankylosis (Fig. 3).
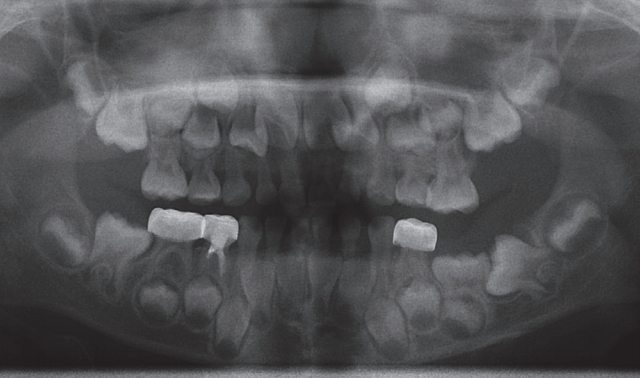
Panoramic radiograph showed horizontal impaction of the permanent mandibular left first molar with primary retention of the primary mandibular left second molar.
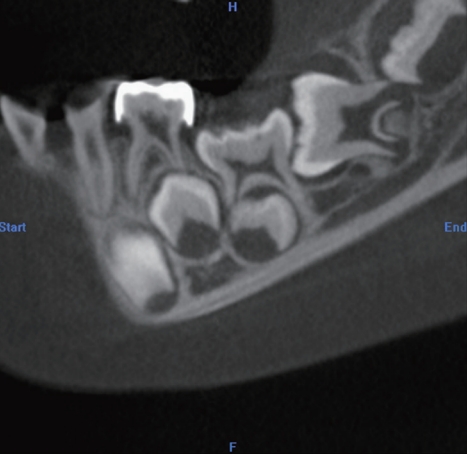
From CT imaging, loss of periodontal ligaments of the primary mandibular left second molar was observed, and the tooth bud of the mandibular left second premolar was displaced toward the lower side.
At initial examination, root development of the primary mandibular second molar was nearly complete and ankylosis was suspected. Also, as it was locked to the mandibular first molar, spontaneous eruption of the primary second molar seemed to be unlikely. Therefore, considering the patient’s compliance, we decided to extract the primary second molar under general anesthesia and perform orthodontic traction of the horizontally impacted first molar.
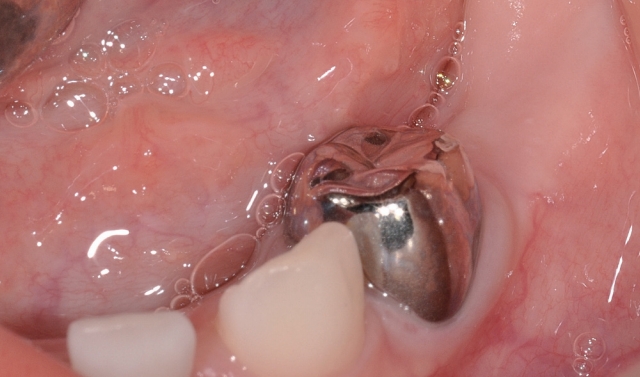
Under general anesthesia, to avoid damaging the premolar tooth bud, after flap elevation for the surgical approach, we extracted the ankylosed primary mandibular second molar in sections. After gingivectomy, orthodontic traction of the mandibular first molar was prepared by attaching a lingual button with ligature wire to the exposed occlusal surface (Fig. 4). Using a modified Nance holding arch and power chain, traction of the horizontally impacted first molar was initiated and maintained for 6 months (Fig. 5), leading to approximately 45° improvement in angle and root dilaceration of the first molar was observed. Next, using a modified Halterman appliance, we positioned a new anchor and enforced distalization of the improved mandibular left first molar and planned distal movement of locked mandibular right first molar. Mandibular right first molar was relocated into proper position after 3 months, and tilting of the left mandibular first molar was almost upright after 6 months. Subsequently, due to premature contact of the maxillary left first molar with the lingual button, we planned to position the mandibular left first molar completely upright and regain space for the premolar tooth bud using a removable space regainer with a distal screw, and then used it as a removable space retainer. Examination after 24 months revealed an upright mandibular left first molar even if dilacerated and regaining of eruption space for the mandibular left second premolar (Fig. 6A, 6B).
Panoramic radiograph showed extraction of the primary mandibular left second molar and lingual button attached to the permanent mandibular left first molar for orthodontic traction.

A modified Nance holding arch was applied for orthodontic traction of the horizontally impacted mandibular left first molar using intermaxillary force.
52 months follow up after orthodontic traction. (A) The permanent mandibular left first molar was distalized to its normal position, allowing eruption space for the mandibular left second premolar. (B) Panoramic radiograph showed improvement in the position of the mandibular left second premolar and upright mandibular left first molar even if dilacerated.
2. Case 2
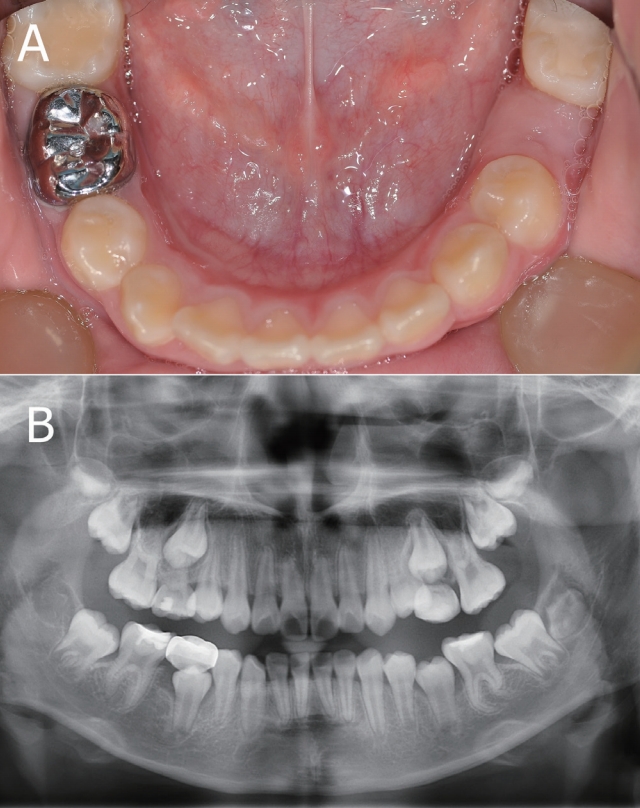
A 7-year-old girl with horizontally impacted mandibular left first molar was referred to the Department of Pediatric Dentistry, College of Dentistry, Chosun University. Clinical findings revealed early mixed dentition with non-eruption of the primary mandibular left second molar and permanent mandibular left first molar (Fig. 7).

First visit. Both primary second molar and permanent first molar in the left mandible were not observed on an intraoral photograph.
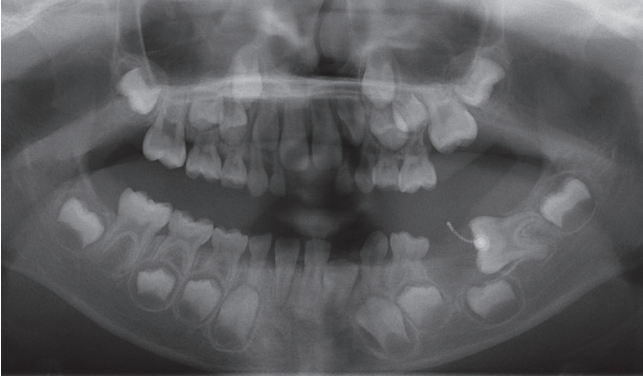
Panoramic radiograph showed primary retention of the primary mandibular left second molar and displacement of the second premolar tooth bud toward the lower and distal side. The mandibular left first molar was horizontally impacted, showing tooth development at Nolla stage 8(two-thirds of root completed) (Fig. 8). The oral examination revealed no relevant familial or medical history. CT imaging showed loss of periodontal ligaments of the primary mandibular second molar and the displacement of the second premolar tooth bud in a inferior, disto-lingual direction (Fig. 9). Therefore, the primary mandibular second molar was pseudo-diagnosed of ankylosis, and the horizontally impacted mandibular first molar was planned for orthodontic traction after surgical extraction of the primary second molar.

Panoramic radiograph showed horizontal impaction of the permanent mandibular left first molar with primary retention of the primary mandibular left second molar.

(A, B) From CT imaging, loss of periodontal ligaments of the primary mandibular left second molar was observed and the tooth bud of the mandibular left second premolar was displaced toward the lower, distal, and lingual side.
A flap was surgically elevated, and the ankylosed primary mandibular left second molar was extracted by cutting it into several pieces to avoid damaging the premolar tooth bud. A lingual button was attached to the occlusal surface of the exposed permanent mandibular first molar for orthodontic traction (Fig. 10, 11). A removable maxillary appliance was applied to promote traction of the permanent mandibular first molar, and a resin bite block was used to improve retention of the appliance and increase the action range of occlusion (Fig. 12). For 10 months with the appliance, the permanent mandibular first molar was distally upright and root dilaceration was observed. After that, a removable space regainer with a distal screw was applied to complete the upright movement of the mandibular first molar.

A lingual button was attached to the permanent mandibular left first molar for orthodontic traction.
Panoramic radiograph showed the extraction of the primary mandibular left second molar and lingual button attached to the permanent mandibular left first molar for orthodontic traction.

A removable maxillary appliance with a resin bite block was applied for orthodontic traction of the permanent mandibular left first molar.
After 6 months, the permanent mandibular left first molar was distalized to its normal position and used band and loop until the eruption of the second premolar (Fig. 13). After 18 months, displacement was improved with normal eruption. In addition, we observed complete uprightness of the first molar with normal eruption but clear dilaceration of the root (Fig. 14).

26 months follow up after orthodontic traction. 10 months after applying a space maintainer, From the panoramic radiograph, the mandibular left second premolar had improved position and the root dilaceration of mandibular left first molar was observed.
Ⅲ. Discussion
Eruption disturbance occurs rarely in primary dentition, with a prevalence rate of 0.01%[12,13]. Most cases with eruption disturbance in primary dentition occur in second primary molars[14,15]. Eruption disturbance is usually found in permanent dentition, occurring most frequently in the third molar, followed by the maxillary canine, mandibular premolar, and mandibular canine. Especially, the prevalence rate of mandibular first molar is 0.01%[16]. Patients rarely present with simultaneous primary retention of the primary second molar and horizontal impaction of the first molar, and formation of an ideal occlusion is difficult in such cases.
In both cases, unerupted primary mandibular left second molar was diagnosed as the primary retention. Radiographically, the primary second molar was normally oriented in its eruption path, but the crown was covered by mucosa with no definable obstacles, and eruption was at least 2 years behind schedule.
We chose to extract the primary second molar which showed primary retention due to ankylosis. The primary second molar was pseudo-diagnosed of ankylosis since a significant amount of periodontal ligament space was lost based on the CT scan. In fact, the tooth did not show any luxation after being surgically exposed, thus, the primary second molar was extracted by cutting it into several sections. Ankylosis can be clinically diagnosed by percussion and mobility test. Futhermore, the loss of normal periodontal space and root surface due to replacement by bone suggests the criteria for the diagnosis of ankylosis from radiographs[17]. Diagnosis of primary molar ankylosis is clinically significant, as it does not respond to orthodontic force[18]. However, diagnosis of an unerupted ankylosed tooth can be difficult since clinical diagnostic examinations cannot be used. An ankylosed primary molar is problematic for the eruption and development of permanent dentition, causing issues such as malocclusion from loss of arch length, tilting of the adjacent teeth, or extrusion of opposing teeth[13,19,20].
In the present cases, initial examination revealed that the succedaneous tooth buds were displaced due to primary retention of the primary second molar. Conventional treatment is the extraction of the primary tooth followed by application of a space maintainer for eruption of the succedaneous tooth bud[21]. If the eruption path of the succedaneous tooth bud does not improve, surgical exposure followed by orthodontic traction may be needed.
The cause of horizontally impacted mandibular first molars is unknown. Unlike other permanent teeth, normal molars develop from the distal extension of the dental lamina without eruption of preceding primary teeth, due to the lack of space for such tooth buds in the jaw, the tooth bud of mandibular first molar begins to tilt. As the jaw develops gradually, the tooth gradually tilts upright[22]. After eruption, the tilted first molar contacts the primary second molar and erupts until it reaches the occlusal plane through distal appearance[23]. However, several factors could cause horizontal impaction of the mandibular first molar such as lack of jaw growth, mesiodistal length of the primary second molar, delayed calcification of the first molar, and abnormal angulation of the erupting first molar[24-26]. The primary retention of the primary mandibular second molar was thought to be the greatest contributing factor in the present cases.
Eruption disturbance of permanent molars can result in decreased height of the lower face, imperfect development of the alveolar process, formation of a follicular cyst, pericoronal inflammation, tilting of adjacent teeth, root resorption of neighboring teeth, extrusion of antagonists, caries, and periodontal diseases[6,27-29].
Various factors should be considered in choosing the appropriate treatment for eruption guidance of the mandibular first molar, including appearances of delayed eruption, development of the tooth, and the patient’s age and compliance. Palma et al .[30] reported that as delayed eruption occurs at a young age, the age of the patient is a key factor in the prognosis for permanent molars. In addition, the root development stage is more important than the non-eruption depth. Kaban et al .[31] reported that treatment is less successful when the roots of the unerupted tooth are completely formed, and the presence of dilacerated roots is a determinant of poor prognosis. Meanwhile, successful treatment depends on the tooth axis of the impacted permanent tooth. For example, eruption guidance can be successfully established when the axis of the tooth is oriented within 45° of the normal angle, whereas eruption guidance is difficult when the tooth axis angulation exceeds 90° from the normal angle[32,33].
The mandibular first molars in our cases, though they were Nolla stage 7 and 8 in the tooth development stage Nolla[34] suggested, showed no emergence. Also, the tooth was oriented at approximately 90°, so we did not expect spontaneous tooth eruption. Overall, the tooth development stage and the axis angle and position of the eruption-delayed tooth can be considered to be important factors in determining orthodontic traction. Commonly, orthodontic traction for eruption guidance in pediatric cases is difficult due to compliance issues and limited anchorage. Thus, conservative methods are generally the first recommendation. Surgical exposure is commonly used in delayed eruption of the first molar[35]; however, to increase the possibility of successful treatment, we used orthodontic traction by intermaxillary force in our cases.
One of the most important factor to consider orthodontic traction for children is the cooperation of the patient and guardian. A modified Nance holding arch and power chain were used in the first case, and a removable appliance and elastic rubber band were used in the second case. A suitable type of the orthodontic appliances should be considered based on patient cooperation. For example, the child from case 1 showed poor cooperation, thus, a fixed appliance and power chain, which does not need regular replacement, were used.
Root dilaceration of the first molar was observed in both cases after treatment. When eruption occurs, the change in tooth axis following the position of the calcified root causes the root apex in the soft tissue to undergo root dilaceration[23]. Therefore, root dilaceration is unavoidable in the traction of a horizontally impacted first molar and thought to decrease with the last stages of root formation; however, the likelihood of orthodontic traction failure may increase.
To date, there is no standard treatment for cases of horizontally impacted first molar with primary retention of primary molar. However, delays in diagnosis and treatment can lead to increased complications with fewer options for conservative treatments. Therefore, pediatric dentists must practice prevention, early diagnosis, and treatment through periodic dental examination of primary and mixed dentition.
Ⅳ. Summary
It is critical to diagnose eruption disturbance early in mixed dentition. For eruption guidance of a delayed eruptive tooth, appropriate treatments should be done, considering the cause and appearance of delayed eruption, tooth development, and the age and compliance of patients. In these cases, delayed eruptive primary molar of primary retention was extracted and mandibular first molar of horizontal impaction was orthodontically tracted with intermaxillary force using fixed or removable appliances. Orthodontic traction of the mandibular first molar, root dilaceration was unavoidable; however, through early diagnosis and treatment, the displaced premolar tooth bud improved, and eruption guidance was successfully done for the normal occlusion of the first molar.