Erythrosine과 LED를 이용한 광역동 치료 후 Streptococcus mutans 바이오필름의 회복
Recovery of Streptococcus Mutans Biofilm after Photodynamic Therapy with Erythrosine and LED Light Source
Article information
Abstract
이 연구의 목적은 erythrosine 매개 광역동 치료 (Photodynamic therapy, PDT)가 Streptococcus mutans 바이오필름 회복에 미치는 영향을 Colony Forming Unit (CFU) 측정과 공초점 레이저 주사 현미경의 관찰을 통해 평가하는 것이었다.
PDT에서 광감각제로 erythrosine을 사용하였다. S. mutans ATCC 25175 바이오필름에 LED 광원을 통해 광역동 치료를 시행하였다. 클로르헥시딘 (Chlorhexidine, CHX) 처리한 군을 양성대조군으로 설정하였다. 각 군에 따른 처리 후 바이오필름의 회복을 위해 배양하였다. 세균 생존율을 처리 직후, 재배양 후 3시간 간격으로 24시간까지 CFU 계수를 통해 측정하였다.
항균 처리 직후 PDT, CHX에서 모두 음성대조군과 비교 시 S. mutans CFU 수가 유의하게 감소하였다. 재배양 12시간 후 PDT는 음성 대조군과 비교 시 CFU 수 감소에 관하여 통계적인 유의성을 띄지 않았지만 CHX는 24시간 동안 통계적으로 낮은 CFU 수를 보였다.
Erythrosine을 이용한 광역동 치료는 S. mutans 바이오필름 형성을 효과적으로 억제하지만 클로르헥시딘보다 바이오필름의 회복이 빠르게 나타났다. 이 연구는 치아 우식 예방을 위한 광역동 치료의 임상적 효과에 관한 통찰력을 제공한다.
Trans Abstract
The aim of this study was to evaluate the effects of erythrosine-mediated photodynamic therapy (PDT) on Streptococcus mutans biofilm recovery by counting its colony-forming units (CFUs) and via confocal laser scanning microscopy analysis at different time points following PDT.
In PDT, photosensitizer was an erythrosine. S. mutans ATCC25175 biofilms were irradiated using an LED curing light. Chlorhexidine (CHX) was used as positive control. After each antimicrobial treatment, samples were cultured to allow biofilm recovery. Viability was measured by calculating the CFU counts after treatment and after every 3 hours for up to 24 hours.
Immediately after treatment, the PDT and CHX groups showed equally significant decreases in S. mutans CFU counts compared to the negative control. After 12 hours of reculture, the PDT group showed no significant difference in the decrease in CFU count compared to the negative control, whereas the CHX group showed significantly lower CFU counts throughout the 24-hour period.
Erythrosine-mediated PDT can effectively inhibit S. mutans biofilm formation. However, biofilm recovery occurred earlier in the CHX group after PDT. This study provides insights into the clinical effectiveness of PDT in preventing dental caries.
Ⅰ. Introduction
Dental caries indicates the tooth erosion due to acids produced by microorganisms in oral biofilms[1]. Biofilms are defined as structured microbial communities bound to a surface and encased in an extracellular matrix[2]. The life cycle of oral biofilms includes attachment (interaction between bacteria and tooth surface), maturation (formation of a viable three-dimensional microbial structure), and dispersion (release from the biofilm and readily colonize other surfaces)[3].
Streptococcus mutans is a representative microbial strain closely associated with early childhood caries (ECC)[4], as it substantially contributes notably to the pathogenesis of dental caries owing to its adhesive ability, acid production, and acid resistance in the oral cavity[5]. To control the growth of the causal microorganisms of dental caries, interventions such as plaque removal or use of an antimicrobial agent should be considered[6]. However, it is difficult to achieve a satisfactory state of plaque control using mechanical plaque removal as it can damage the oral tissue. Additionally, antimicrobial agents may cause side effects, such as destruction of normal microflora or production of resistant strains[7]. Photodynamic therapy (PDT) has been suggested as an alternative treatment for dental caries. PDT involves a photosensitizer and light source that generate reactive oxygen species (ROS) to destroy the microbial DNA and cell membrane, causing apoptosis of microbial cells[8].
The photosensitizers commonly used for PDT are methylene blue, toluidine blue O, erythrosine, and eosin. Among these, erythrosine can be used as a photosensitizer in dentistry because it has been approved for use in the mouth as a plaque disclosing agent and shows no toxicity[9]. Erythrosine is a xanthene dye characterized by absorption of light at wavelengths ranging 500 - 550 nm[10]. The conventional dental LED curing light has an emission wavelength of 385 - 515 nm. The combination of erythrosine and a dental curing unit can be used for PDT effectively.
Regardless of the antimicrobial method, the complete eradication of bacteria is difficult. Although previous studies have investigated the antimicrobial effects of erythrosine-mediated PDT on S. mutans biofilms, no study has reported biofilm recovery following PDT.
Thus, the aim of this study was to identify the pattern of post-PDT biofilm recovery on S. mutans biofilms in vitro and the possibility of clinical use for preventing dental caries.
Ⅱ. Materials and Methods
1. Bacterial culture and culture conditions
Streptococcus mutans ATCC25175 standard strain was cultured in Brain Heart Infusion (BHI) broth (Becton, Dickinson and Company, Sparks, MD, USA) in an incubator at 37°C under 5% CO2 for 18 hours.
Turbidity of the bacterial culture solution was measured using a spectrophotometer (X-ma 1200v, Human Corporation, Seoul, South Korea), and the suspension was diluted to yield a cell density of 1 × 107 CFU/mL.
2. Biofilm formation
A hydroxyapatite (HA) disk (1.27 cm in diameter, Biosurface Technologies Corporation, Bozeman, MT, USA) was sealed with a silicon impression material on all sides, except the one subjected to treatment, and sterilized with EO gas. Next, the HA disc was placed in a 12-well cell culture plate, followed by the addition of 1,980 μL of BHI broth and inoculation of 20 μL of S. mutans culture solution (diluted to 1 × 107 CFU/mL), to yield a final cell density of 1 × 105 CFU/mL. Next, biofilm formation was allowed to proceed in an incubator at 37°C under 5% CO2 for 24 hours.
3. Photosensitizer and light source
Erythrosine (Sigma-Aldrich, St Louis, MO, USA) was used as the photosensitizer, and the concentration of erythrosine was set as 40 μM, according to previous studies[11]. Erythrosine (molecular weight, 879.86 g/mol) powder was mixed with phosphate-buffered saline (PBS), followed by filter sterilization, to prepare a 1 mM erythrosine stock solution. And it was stored in the dark at -20℃. The working solution required for the experiment was prepared via PBS dilution to obtain 40 μ M erythrosine. Valo (LED) curing light (Ultradent Products Inc, South Jordan, UT, USA) was used as the light source. The irradiation distance was 10 mm, and in the measurement using a radiometer, the output was 1,200 mW/cm3. In this study, 18 J/cm2 of energy was irradiated for PDT. By applying the formula, 1 W = 1 J/s, 1 J = 1 W × 1 s, the LED irradiation time was calculated, which was set to 15 seconds for the curing unit.
4. Biofilm treatment
Each HA disk was gently washed twice with 2 mL PBS to remove loosely attached bacteria. Three groups were formed in accordance with the treatment method. Group I was the negative control, treated solely with PBS. Group II underwent PDT treatment. For PDT, cells were treated with 40 μM erythrosine for 3 minutes, followed by irradiation at an energy density of 18 J/cm2 [11,12]. Group III was a positive control, treated with 0.12% chlorhexidine (CHX) (Hexamedine, Bukwang Pharmaceutical, Seoul, South Korea). After application of CHX, each specimen was washed twice with 2 mL PBS to remove remaining CHX.
5. Biofilm reformation
After biofilm treatment for each group, the respective HA disks were transferred to a fresh 12-well cell culture plate with 2 mL of BHI broth for reculture. Biofilm reformation for each group was observed for up to 24 hours.
6. CFU counting
Following biofilm treatment for each group, the respective wells were treated with ultrasound (VC 100, Sonics & Materials Inc., Danbury, CT, USA) twice (for 10 seconds each) to produce the bacterial suspension. Then, 50 μL of the suspension in each well was diluted and spread onto blood agar plates (Hanil-KOMED, Seongnam, Korea), followed by culturing in an incubator at 37°C under 5% CO2 for 72 hours. The CFUs were counted, and the means of duplicate counting were obtained. Next, the disks cultured in BHI broth were taken out, washed with PBS at 3-hour intervals, and the CFUs were counted for up to 24 hours, as described above.
7. Confocal laser scanning microscopy (CLSM)
To assess cell viability, the disks in which biofilm had formed were visualized using CLSM. CLSM was performed immediately after the treatment(0 hour) and after 12 and 24 hours, to determine bacterial cell survival after each antimicrobial treatment. Samples were stained with the LIVE/DEAD BacLight Bacterial Viability Kit Solution (Molecular Probes, Inc., Eugene, OR, USA) in the dark for 20 minutes. The LEICA TCS SP8 system (Leica Microsystem, Wetzlar, Germany) was used for observation.
8. Statistical analysis
SPSS 22 (SPSS Inc, Chicago, IL, USA) was used for the statistical analyses of log CFU/mL. The normality of the experimental results was examined using the Shapiro-Wilks test. The Kruskal-Wallis test was performed for each group to validate the statistical significance, followed by Bonferroni post-hoc analysis to determine the statistical significance of multiple comparisons (p < 0.05).
Ⅲ. Results
1. CFU counting
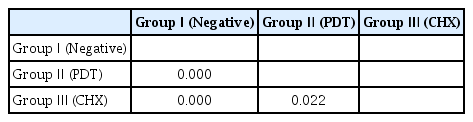
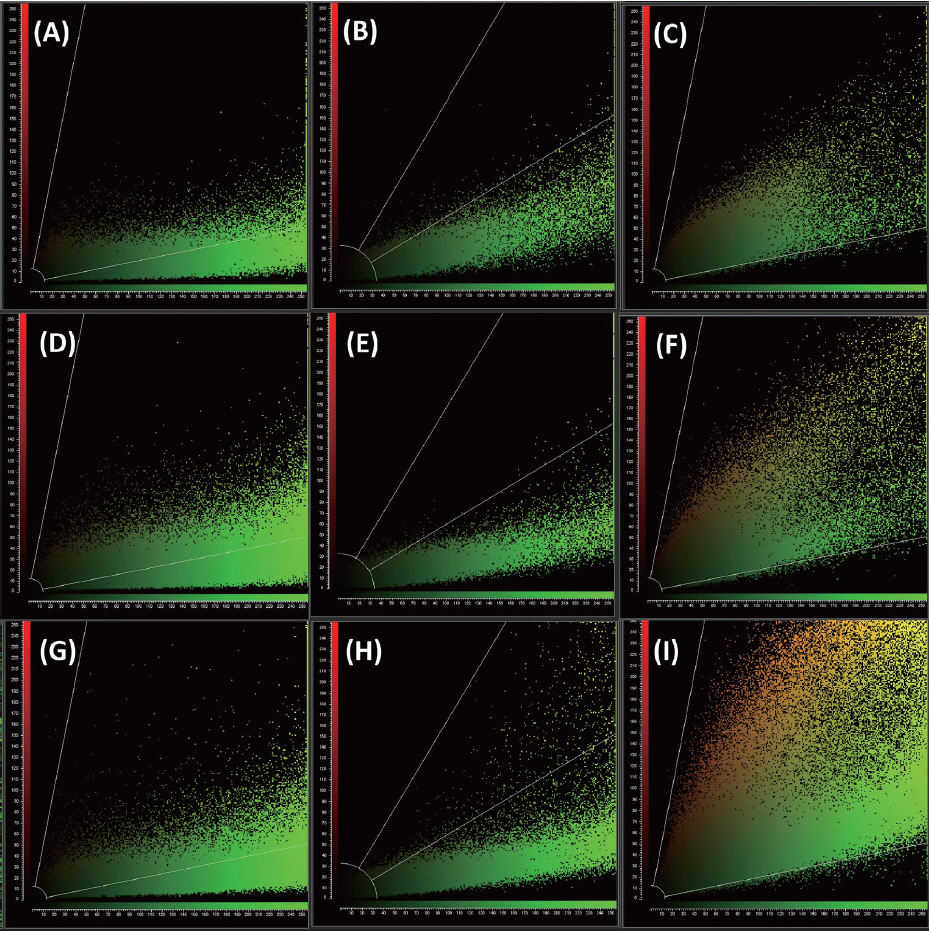
The time-based CFU counts are presented in Table 1 and Fig. 1. The CFUs in Groups II (PDT) and III (CHX) decreased significantly compared to those in Group I (negative control) (Table 2).
Mean and standard deviation of Streptococcus mutans bacterial counts at different time points. Kruskal-Wallis test and Bonferroni’s post-hoc test (a, b, c: p < 0.05)
a: Comparison with negative control; b: Comparison with PDT; c: Comparison with CHX
A time-dependent increase in CFU number was observed for Groups II and III after the addition of the medium for reculture (Fig. 1). After 12 hours of reculture, Group III showed significantly low CFU counts compared to those in Groups I and II (Table 3). However, Group II showed a steep increase in CFU counts after reculture. After 12 hours of reculture, the CFU counts of Group II were no longer significantly different from those of Group I, suggesting biofilm recovery upon PDT. After 24 hours of reculture, only Group III showed significantly low CFU counts compared to the other groups (Table 4).
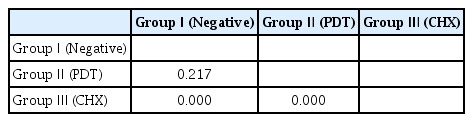
2. CLSM analysis
Specimen was evaluated to visualize cell viability via CLSM. The viable cells emitted green fluorescence, and dead cells, red fluorescence. The results of the colocalization analysis of green and red fluorescent colors were visualized as a scatter plot, a type of pixel distribution diagram, using Pearson’s correlation analysis (Fig. 2). Group I showed substantial amount of green fluorescence distributed along the X-axis compared to other groups, indicating relatively higher live bacterial abundance (Fig. 2 A, D, G). Group III showed substantially enhanced red fluorescence compared to other groups (Fig. 2 C, F, I).
Ⅳ. Discussion
Studies have reported the use of erythrosine as a photosensitizer in PDT to exert antimicrobial effects against S. mutans cells in suspensions or biofilms[9,11-15]. After antimicrobial treatment, residual bacteria induce the recovery of biofilm growth and CFU counts, indicating the possibility of reinfection. In this study, the biofilm recovery after PDT on biofilms formed by S. mutans, a major bacterial species causing dental caries, was compared, and evaluated against that when CHX is used.
In this study, 18 J/cm2 of energy was used for irradiation with an appropriate light source. A previous study has determined the optimal treatment parameters to ensure maximal preventive effect of erythrosine-mediated PDT on dental caries[14]. The ideal conditions include an irradiation time exceeding 30 seconds and energy output of 600 mW/cm2 from the halogen. Additional light irradiation longer than 30 seconds did not enhance or exhibit a significant difference in the antimicrobial effect. Kim et al.[11] reported that if the same total amount energy of 18,000 mW/cm2 was used, the photodynamic effect would remain unaltered regardless of the types of light sources used. The light source used in this study has a characteristic of high output, which would facilitate the shortening of the light curing time for PDT to 15 seconds. Considering the characteristics of the treatment in pediatric dentistry, using high output light-curing unit can be reasonably advantageous because it is time-efficient, thereby resulting in a shortened chair time.
The CFU counts immediately after treatment were significantly lower in Group II (PDT) than in Group I (negative control), thus verifying the antimicrobial ability of erythrosinemediated PDT on S. mutans. This is consistent with the results of previous studies[9,11-15]. The American Society of Microbiology defines antimicrobial activity as a ≥3 log CFU/mL reduction from the starting inoculum[16]. Groups II and III showed a decrease of ≥3.0 log CFU/mL immediately upon treatment, thereby confirming the antimicrobial activities of PDT and CHX.
In this study, the CFU counts were significantly lower in Group III than in Groups I and II throughout the 24-hour reculture period. This trend was also observed in the CLSM analysis results. Group III had distinctly more red fluorescent areas than the other groups for 24 hours, indicating that the proportion of dead cells was dominant in Group III. The results of this study corroborate those of previous studies that demonstrated the substantivity of CHX. When adhered to the tissue, it exhibits antimicrobial effects for up to 12 hours[17,18].
After the initiation of biofilm reculture following PDT, an increase in CFU counts was observed for Group II. However, the differences in CFU counts against the negative control were no longer significant after 12 hours. This indicated that biofilm recovery mostly occurred after 12 hours.
The repeated use of CHX should be avoided as its long-term use can cause side effects, such as tooth and oral cavity discoloration, increase in supra-gingival plaque formation, temporary loss of taste, burning sensation, and mouth dryness[19]. A previous study reported the risk of resistance toward CHX on bacteria in oral biofilms[20]. As an alternative to CHX, the use of a plaque-disclosing agent as a photosensitizer in PDT may induce selective apoptosis in plaques that cause dental caries without harming the host because the agent selectively adheres to the plaque[6,21-23]. An additional advantage of PDT is the absence of resistant strains, a common side effect associated with the use of antimicrobial agents[23]. It is unlikely that bacteria would develop resistance to the cytotoxic action of ROS. Therefore, the use of PDT would not lead to further developments in resistance[24], which suggests the potential for repeated use of PDT within short intervals. Thus, the relatively faster biofilm recovery by PDT than by CHX is likely to be complemented by applying PDT in shorter, more frequent intervals. Park et al.[13] reported that PDT has a significant antimicrobial effect on S. mutans biofilm when the whitening LED used in homes was used as the light source. This further supports the potential and more frequent use of PDT with commercially available whitening home devices.
Due to frequent exposure to light source, PDT would cause thermal damage of oral tissue. Temperature range of healthy normal dental pulp is stated as 34 - 35°C[25]. There is a consensus that the use of LED curing light can result in a pulp chamber temperature rise to values higher than the threshold temperature increase of 5.5°C, considered harmful for the pulp[26]. Further studies would be needed to determine relationship between application of light source in PDT and potential thermal damage of pulp tissue.
Several studies have reported the antimicrobial effects of erythrosine-mediated PDT on cariogenic bacteria immediately after intervention. Nevertheless, no study has investigated its antimicrobial effects on S. mutans post-treatment in terms of biofilm recovery. This study is significant, because it evaluated the pattern of biofilm recovery after subjecting S. mutans to PDT in set time intervals via quantitative method using CFU counting and qualitative method using CLSM for analysis.
However, the present study has a few limitations. It was performed to identify the antimicrobial effect on mono-species biofilm formed in vitro by S. mutans . Biofilms in the actual oral cavity comprise a community of multiple bacterial species that cause dental caries. Multi-species cariogenic biofilms have greater thickness than mono-species biofilms, and due to the structural complexity and bacterial interaction, their resistance to antimicrobial treatment is high[27]. Further studies should be conducted to develop a protocol that is clinically feasible for use against multispecies biofilms, while evaluating the effects of PDT in clinical conditions. And recovery of multispecies biofilms following PDT should also be conducted.
Although PDT cannot replace the currently used antimicrobial agents and dental treatment, it is a promising non-invasive adjunctive therapy for management of oral infection[28]. PDT’s effective antimicrobial effect in combination with a photosensitizer and LED light source indicates its potential usefulness in daily dental care.
Ⅴ. Conclusions
The in vitro treatment of S. mutans biofilms with erythrosine-mediated PDT led to a significant decrease in CFU counts immediately after treatment; this significant decrease disappeared after 12 hours of reculture. Erythrosine-mediated PDT could effectively inhibit the growth of S. mutans biofilms. However, biofilm recovery ensued mostly after 12 hours. Taken together, this study provides insights into long-lasting clinical effectiveness of PDT to prevent dental caries.