 |
 |
| J Korean Acad Pediatr Dent > Volume 45(4); 2018 > Article |
|
초록
이 연구의 목적은 Calcium silicate를 기반으로 한 2종의 치수복조재 (Biodentine, RetroMTA)와 임상에서 사용되는 여러 가지 상아질접착제 간의 전단결합강도를 비교 평가하는 것이다.
중심구를 가진 아크릴 레진 블록 80개를 제작하고 2그룹으로 나누어 Biodentine (BD)과 RetroMTA (RMTA)를 중심구 안에 채운 후, 무작위로 10개씩 4개의 하위군을 나누어 재료 상방에 4가지 상아질 접착제인 Clearfill SE (CSE), AQ bond plus (AQ), All bond universal (ABU) 자가부식, ABU 일괄부식을 도포한 뒤 그 위에 복합레진을 적용하였다. Universal testing machine을 이용해 전단결합 강도를 측정하였다. 통계분석은 Kruskal-Wallis를 사용하였고 Mann-Whitney의 사후검정을 하였다.
연구결과, BD - ABU 자가부식군이 가장 높은 전단결합강도를, RMTA - AQ 군이 가장 낮은 전단결합강도를 보였다. ABU 일괄부식과 ABU 자가부식군, ABU 일괄부식과 CSE 간의 유의미한 차이는 보이지 않았다. 또한 같은 상아질접착제 적용 시, BD가 RMTA보다 높은 전단결합강도를 보였다. 또한, BD와 RMTA 그룹 군에서 ABU 자가부식군 도포 후, 레진 적용했을 때 향상된 전단결합강도를 보였다.
Abstract
The aim of this study was to measure the shear bond strength (SBS) of different adhesive systems to calcium silicatebased materials (Biodentine and RetroMTA). Eighty cylindrical acrylic blocks, with a hole (5.0 mm diameter, 2.0 mm height) in each, were prepared. The holes were filled with Biodentine (BD) and RetroMTA (RMTA), and the specimens were divided into 2 groups. Each group was classified into 4 subgroups: Clearfil™ SE (CSE) ; AQ bond (AQ) ; All bond universal Self-etch (ABU-SE) ; and All bond universal Total-etch (ABU-TE). After the application of different adhesive systems, composite resin (Z350) was applied over BD and RMTA. The SBS was measured using a universal testing machine, and the data were compared using the Kruskal-Wallis test and the Mann-Whitney test. The highest and lowest values of SBS were observed for BD-ABU-SE and RMTA-AQ, respectively. No significant differences were found in the SBS between ABU-TE and ABU-SE and between ABU-TE and CSE to BD and RMTA. According to the data, BD showed a higher SBS than did RMTA when BD and RMTA are compared in the same adhesive agents. Further, among all groups, composite resin with ABU-SE showed better bond strength to BD and RMTA.
Mineral trioxide aggregate (MTA) was introduced in the field of dentistry by Mahmoud Torabinejad. Over the last decade, MTA has rapidly gained great popularity, especially in pediatric and endodontic dentistry.
MTA forms a uniform and thick dentinal bridge faster than does calcium hydroxide, and it can be used safely when placed adjacent to the pulp and periodontal tissues. It also has lower solubility, better sealing ability, and facilities the control of bleeding and provides a strong barrier against bacterial leakage[1,2]. Therefore, MTA is considered to be one of the best materials for use in various endodontic treatment[3].
Despite its unique combination of favorable properties, MTA has a major disadvantage, that is, a long setting time[4], which is a limitation for use in children who show uncooperative behavior during treatment. In addition, MTA is difficult to manipulate and may cause discoloration of teeth[5].
Recently, new calcium silicate-based cements, including Biodentine (BD, Septodent, Saint-Maur-des-Fosses Cedex, France) and RetroMTA (RMTA, BioMTA, Seoul, Korea), have been introduced to overcome the limitations of MTA.
BD is a two-component material : the powder consists of tricalcium silicate as the major component, calcium carbonate as a filler, and zirconium oxide as a radiopacifier ; the liquid consists of distilled water, calcium chloride, and a water-soluble polymer. Calcium chloride functions as a setting accelerator for faster setting of the material. The water-soluble polymer acts as a water-reducing agent for increasing the material strength[6]. The advantage of BD over MTA is its short setting time (12 minutes), high viscosity, ease of manipulation[7]. BD also shows improved antibacterial properties, greater biocompatibility, and remineralization properties than previously developed MTA, as well as a low cytotoxic effect[8].
RMTA is a ZrO2-containing calcium aluminate cement that contains hydraulic calcium zirconia complex as a contrast media. When compared to MTA, the advantage of RMTA is its fast setting time (initial setting time of 150 seconds). The fast setting time may be attributed to the zirconium complex, which has been reported to modify the chemical reactions involved in setting and change physical properties[9]. In addition, RMTA does not cause tooth discoloration and would be suitable for use in the moist environment of the oral cavity.
In addition to favorable physical properties, biocompatibility, and bioactivity, the bond strength between restorative and calcium silicate-based materials is an important factor determining the quality of the filling and success of the restoration. Bonding of composite resin to a calcium silicate-based material creates an adhesive bond that can distribute stress evenly over the adhesion site. Currently, dentin adhesives tend to simplify the application step, shorten clinical application time, and reduce technique sensitivity[10]. Short treatment times and simple treatment procedures are very important for children who are not cooperative during treatment.
Self-etch (SE) adhesive systems reduce technique sensitivity because they do not require washing and drying during application. Further, SE adhesive systems can simplify multi-step etch-and-rinse procedures and minimize contamination with saliva by reducing the number of steps, especially in children who are uncooperative[11]. Recently, a new type of SE adhesive called “universal” has been introduced into the market. It can be used with either the etch-and-rinse or SE modes, enabling dentists to choose the most appropriate application mode for the prepared cavity.
The purpose of this study was to evaluate the shear bond strength of a resin composite to BD and RMTA, which have relatively fast setting times among calcium silicate-based cements, with four different adhesive systems of each generation.
Four commercial adhesive systems were tested in this study: 2-step SE adhesive system, Clearfil™ SE bond (Kuraray Medical, Osaka, Japan) ; 1-step SE adhesive system, AQ bond Plus (Sun Medical, Shiga, Japan) ; 1-step SE adhesive system, Allbond universal SE (Bisco Inc., Schaumburg, IL, USA) ; 1-step SE adhesive system, and All-bond universal total etch (TE) ; TE adhesive system. The application procedures for the adhesive materials were conducted according to the manufacturer’s instructions and are described in Table 1.
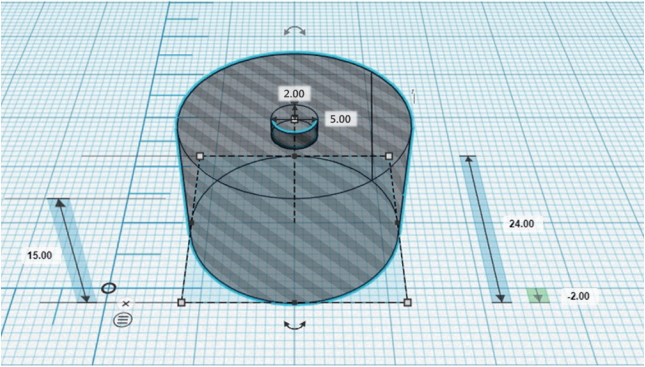
A total of 80 acrylic blocks containing a central hole with a 5.0 mm diameter and 2.0 mm height were designed using 3D printer (Pinter Pro, Bucheon, Korea) for constant specimens production (Fig. 1). BD and RMTA were mixed according to the manufacturer’s instructions. In 40 of the samples, the holes were filled with BD, and in the other 40 samples, the holes were filled with RMTA. After filling BD and RMTA, mylar strip was used to make a uniform surface. Each of the BD specimens was stored at 37℃ in 100% humidity for 12 minutes for setting; RMTA specimens were stored at 37℃ in 100% humidity for 10 minutes for the same purpose.
After setting, the BD and RMTA samples were randomly divided into 4 subgroups of 10 specimens each : Clearfil™ SE bond (CSE) ; AQ bond plus (AQ) ; All bond universal SE (ABU-SE) ; and All bond universal TE (ABU-TE). In all groups, the corresponding adhesive system was applied over BD and RMTA samples, according to the manufacturer’s instructions. A composite resin (Filtek Z350, 3M ESPE, St. Paul, MN, USA) was applied to a cylindrical plastic tube with an internal diameter of 2.0 mm and a height of 3.0 mm. The resin composite was cured with a light-emitting diode (LED) light cure (DemiTM Plus, Kerr, USA) with an intensity of 1200 mV/cm2 for 20 seconds. After the polymerization, the plastic tube was removed carefully, and the specimens were stored at 37℃ in 100% humidity for 24 hours. All the samples were prepared and tested by a single investigator.
For shear bond strength testing, the specimens were secured in a universal testing machine (Instron 3367, Instron Co., Norwood, MA, USA). A knife-edge blade was moved toward the BD and RMTA base/adhesive interface with a crosshead speed of 0.5 mm/min (Fig. 2). The shear force at failure was recorded in Newtons (N), and the shear bond strength was translated to megapascals by dividing the peak load values by the restorative material base area (3.14 mm2).
Fractured surfaces were examined under a stereomicroscope (Nikon SMZ1500, Tokyo, Japan) at a magnification of ×25. The fracture surfaces were categorized as follows: (1) adhesive fracture, failure at the BD/RMTA-restorative interface, (2) cohesive fracture, failure exclusively within the restorative material/base material, and (3) mixed fracture, 2 modes of failure occurring simultaneously. The samples were randomly divided based on the adhesive agents used into the ABU-SE and ABU-TE groups. Prior to scanning electron microscope (SEM) examinations, the specimens were air dried and gold sputter-coated using a 15 mA current for 90 seconds (Hitachi E-1045, Tokyo, Japan). Specimens were analyzed with a SEM (Hitachi S-4700, Tokyo, Japan). Images of the selected materials were obtained at different magnifications.
All data were processed using the SPSS 18.0 (SPSS Inc., Chicago, IL, USA). The Kruskal-Wallis test was used for evaluating shear bond strength and the type of adhesive system and base material. Post-hoc analysis was performed using the Mann-Whitney test. The significance level was set at p < 0.05.
The data on shear bond strength of the adhesive agents to BD and RMTA are presented in Table 2. Among the adhesive systems, BD-ABU-SE (6.87 ± 2.55 MPa) presented the highest shear bond strength and RMTA-AQ (0.39 ± 0.26 MPa) showed the lowest shear bond strength. When all groups were compared, data were arranged as follows in descending orders : BD-ABU-SE, RMTA-ABU-SE, BD-ABU-TE, BD-CSE, RMTA-ABU-TE, BD-AQ, RMTA-CSE, and RMTA-AQ. In both groups, ABU-SE showed the highest shear bond strength to the composite resin. There was no significant difference between ABU-TE and ABU-SE and between ABU-TE and CSE, but a significant difference was observed among the other groups (Table 3).
When BD and RMTA are compared in the same adhesive agents, BD showed significantly higher bond strength than did RMTA. For ABU-SE and ABU-TE adhesive systems, shear bond strengths of BD and RMTA were not significantly different. However, for AQ and CSE, the shear bond strength of BD was significantly higher than that of RMTA (Fig. 3).
The results of the analysis of the fracture mode are shown in Table 4. When the bonding agent was CSE, BD showed mixed fracture and RMTA showed cohesive fracture. In AQ samples, the failure mode of BD was mainly adhesive fracture while RMTA showed cohesive fracture. In the ABU-SE and ABU-TE groups, predominantly cohesive failure occurred with both BD and RMTA. A representative SEM of a fractured BD and RMTA samples exhibiting cohesive fracture is shown in Fig. 4.
The essential goal of pulp therapy is to treat the pulp successfully and preserve the tooth in a good condition for constituting the primary and young permanent dentition[12]. Recently, MTA has been reported to be widely used in pediatric dentistry as a medicament in pulpotomy for primary teeth and as a pulp capping material in immature permanent teeth[2]. It has advantages such as high protection against microleakage, and biocompatibility. However, although MTA has desirable biological properties, some disadvantages have also been observed, such as a long setting time and poor handling characteristics. Further, an additional follow-up is required to apply resin-based restorative materials on the set MTA. In pediatric dentistry, it is especially important to reduce the number of clinical steps and shorten treatment time. To overcome the shortcomings of MTA, fast-setting MTA-like calcium silicate cements, such as BD and RMTA, have been developed.
Clinically, resin-based restorative materials were used for successful restoration of teeth with BD and RMTA. The bond strength between the resin and both the materials with an adhesive influences the quality of fillings. Shear bond strength indicates strength between two materials evaluated by measuring the local force that the bonding layer can withstand[1].
Most of the previous studies have evaluated the effect of various restorations and adhesives on the bond strength of MTA[13]. It has been shown that the shear bond strength of MTA was better with TE adhesive systems rather than with SE adhesive systems[14]. Further, composite resin with TE adhesive systems was suitable as the final restorative material over MTA[15]. However, TE systems are technique sensitive and require several steps in the bonding process. The SE system has been developed to simplify the bonding process. In particular, the long procedure time and complicated process are important factors compromising the quality of fillings in pediatric patients who have difficulty in controlling behavior. Recently, the 6th and 7th generation dentin adhesives have been shown to be useful in pediatric dentistry where behavior management is important, such as for reducing procedure time, simplifying the procedure, and reducing the possibility of contamination during treatment. However, only a few studies have investigated the bond strength of BD to composite resin, and there is limited research on the shear bond strength between RMTA and restorative materials.
The present study was designed to evaluate and compare shear bond strength of dentin adhesives of each generation when used with BD and RMTA. Mean shear bond strength varied between 0.39 and 6.87 MPa in our study. We found that ABU-SE (1-step SE adhesive) exhibited the highest bond strength to BD among all tested adhesives. The bond strength between two restorative materials is an important factor affecting the quality of the fillings. It has been estimated that a bond strength of 17 - 20 MPa may be required to sufficiently resist contraction forces and produce gap-free restoration margins[16]. The low shear bond strength of BD and RMTA groups appears to be due to the low initial cohesive strength. In order for BD, a porous material, to have bulk strength sufficient to resist polymerization shrinkage, at least 2 weeks are required for crystallization of hydrated calcium silicate gel to achieve complete setting of BD and optimal physical properties[17]. In the present study, dentin adhesive was applied to BD after 12 minutes and RMTA after 10 minutes to reenact the one time clinical procedure. It appears that relatively low bond strength and cohesive fracture patterns are caused by the shear force applied to BD and RMTA without sufficient maturation inside the BD and RMTA. However, Cantekin et al.[8] reported that methacrylate-based composites and BD had optimal SBS values (17.7 ± 6.2 MPa). The reason for the difference from the results of this study is the difference in the experimental method such as the speed of load and the magnitude of maximum load when measuring SBS.
RMTA is composed of calcium zirconium aluminate cement containing 60 - 80% calcium carbonate (CaCO3), 5 - 15% silicon dioxide (SiO2), 5 - 10% aluminum oxide, and 20 - 30% calcium zirconia complex. RMTA has smaller particles than does MTA and does not involve the use of any chemical accelerators. Compared to BD, RMTA showed lower shear bond strength when using the same adhesive agents. Ha et al.[18] reported that the particle size of MTA showed a close linear correlation with the initial setting time and final setting time. Further, the particle size of BD is smaller than that of RMTA. It is believed that during setting, the small particle size leads to a significant decrease in the material’s porosity and increase in its compressive strength[6]. According to the manufacturer’s instructions, the final setting time of RMTA is 360 minutes and that of BD is 12 minutes.
Since there was no resin structure in BD and RMTA, the bond with composite resin is completely micromechanical[19]. Since micromechanical bonding directly depends on the physical aspects of the surface, it can be inferred that the surface treatment method would have a major influence on the bonding[20].
The various functional monomers in different adhesives are important in improving the bonding strength with the teeth. In some studies, the functional monomer 10-methacryloyloxydecyl dihydrogen phosphate (10-MDP) has been shown to react with calcium ions in BD and RMTA, thereby increasing microchemical interlocking and chemical adhesion[21]. In the present study, we used the ABU and CSE, which contain the 10-MDP functional monomer; we believe that this could have increased the bonding strength with BD and RMTA. Both BD and RMTA showed significantly higher values of bond strength in the ABU-SE, ABU-TE, and CSE groups than in the AQ group. In addition, hydroxyethyl methacrylate (HEMA) is a hydrophilic composition present only in ABU and CSE. It forms a polymerization network that stabilizes the surface of the material after photopolymerization and then absorbs moisture to aid hydration and setting of calcium silicate[22]. According to the findings of the present study, among all the tested adhesive agents, the AQ showed the lowest bonding strength to composite resin, which might be attributed to its composition.
In the SE mode, the 2-step SE adhesive consists of a primer and bonding agent. To eliminate the inconvenience associated with performing multiple steps, ABU was released as a single solution in a single bottle that was applied using either TE or SE mode. Although CSE and ABU contain similar functional monomers, shear bond strengths of BD and RMTA were significantly different between ABU-SE and CSE. The major difference between CSE and ABU-SE adhesives is the thickness of the adhesive layer. Jang et al.[23] reported that the thickness of the adhesive layer of the CSE was approximately 40 ㎛, but that of ABU-SE was approximately 10 ㎛. Although the thickness of the adhesive layer does not adversely influence the bond strength, it may cause imperfect restorations in some clinical situations.
Several studies have shown that optimal shear bond strength was acquired with TE adhesive systems[24]. Application of phosphoric acid produces a markedly roughened surface on the substrate and creates more retentive microporosities[25]. This may contribute to the reliable micromechanical bonding of the TE adhesive system to MTA[20]. However, we found that ABU-SE exhibited higher shear bond strength than ABU-TE to BD and RMTA. In addition, applying adhesive systems in either SE or TE was seen not to have statistically significant influence bond strength in the present study. Hashem et al.[26] reported that similar shear bond strengths between SE and TE were caused by the porous surface structure of BD, which may imply that there is no difference between the SE and TE techniques. Furthermore, BD and RMTA, which are alkaline, may be buffered due to the acidity of the bonding agents, and this may reduce their bonding effect[26]. This result is similar to that of the studies by Hanabusa et al.[27] and Marchesi et al.[28], who showed that SE or TE adhesive systems do not show significant differences in bonding strength. SEM analysis showed that on the BD-ABU-TE treated surface, some regions showed unique surface structures producing a uniform cracked surface with internal pores. In contrast, BD-ABU-SE did not show an aggressive surface on the substrate (Fig. 5). Therefore, it is suggested that a low pH, such as that achieved with the application of phosphoric acid, could affect the chemical setting of BD and RMTA by interrupting the hydration of calcium silicates, leading to weakening of the setting material’s microstructure.
Fracture analysis indicated that the fracture modes for BD and RMTA specimens were mostly cohesive failures within the calcium silicate-based materials. It is suggested that the curing contraction of the composite resin may induce stresses, resulting in cohesive failure in weak BD and RMTA. In a study of the fracture modes between MTA and restorative materials, cohesive fractures were similarly observed in the MTA. It has been reported that compressive strength of the MTA improves over time, further reducing the likelihood of cohesive failure[29].
On the basis of the results of this study, it may be suggested that ABU adhesive applied on BD and RMTA offers sufficient bond strength without the acid etching procedure, because ABU-TE and ABU-SE showed similar bond strengths. Thus, ABU (7th generation adhesive) can be applied for increasing convenience while treating uncooperative children through the use of a simplified treatment procedure and achieving a reduced risk of contamination with saliva.
The purpose of this study was to compare shear bond strength of various adhesive agents to two calcium silicatebased materials. However, fracture mode and shear bond strength can vary for each calcium silicate-based material depending on the setting time needed for and type of restorative material. This is the limitation of this study and further research is needed to compare the effects of these variables.
Moreover, the results of this study cannot be compared with the results obtained from in vivo studies. Since the current study was conducted in a laboratory setting, studies on the bond strength of these materials in the oral environment may reveal different results. The influence of various variables suggests the necessity for additional research under thoroughly controlled experimental conditions.
Comparison of the shear bond strength between calcium silicate-based materials (BD and RMTA) and adhesive agents of different generations revealed that the BD-ABU-SE group showed the highest shear bond strength and RMTA-AQ had the lowest shear bond strength. There was no difference between the SE and TE modes. In pediatric patients, reducing the number of steps in the treatment procedure may be important for improving the quality of restoration. Further, SE systems are more useful than TE systems for children who show uncooperative behavior. We therefore suggest that the bond strength difference between calcium silicate-based materials and dentin adhesives is one of important factors to consider when selecting restorative materials.
Fig 3.
Comparison of shear bond strength of the samples according to calcium silicate- based materials.
* : statistically difference by Mann-Whitney Test (p < 0.05)
CSE : Clearfil™ SE bond, AQ : AQ bond plus, ABU-SE : All bond universal Self-etch mode, ABU-TE : All bond universal Total-etch mode

Fig 4.
Scanning electron microscope images of cohesive failure. (A) BD-ABU-SE, (B) BD-ABU-TE, (C) RMTA-ABU-SE, (D) RMTA-ABU-TE Magnified images were also obtained of (E) BD-ABU-SE, (F) BD-ABU-TE, (G) RMTA-ABU-SE, (H) RMTA-ABU-TE.
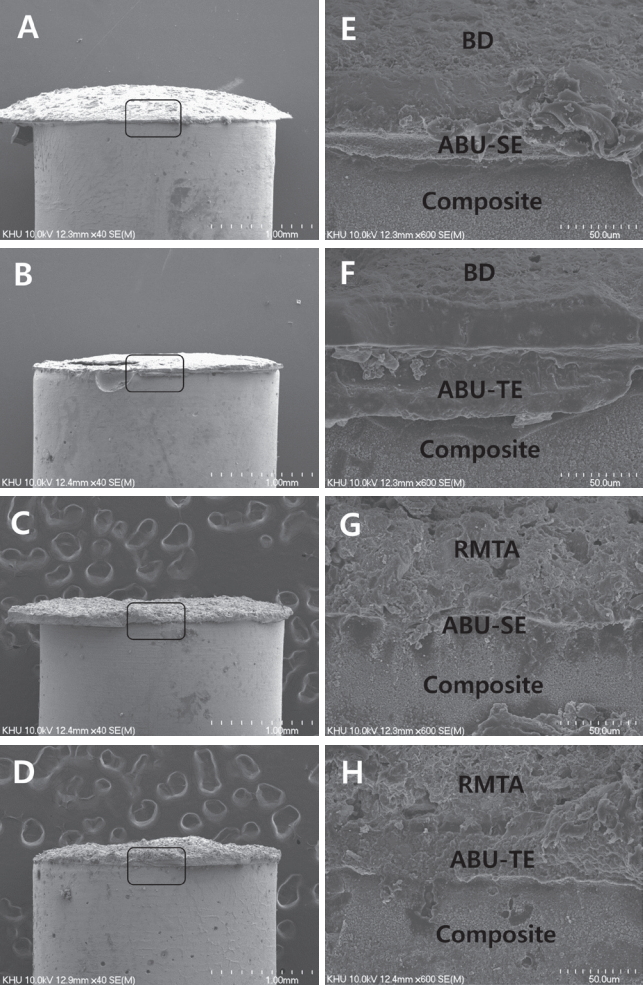
Fig 5.
Scanning electron microscope images of fractured cross section of Biodentine. (A) BD-ABU-SE, (B) BD-ABU-TE.

Table 1.
Adhesive agents used according to the manufacturer’s instructions
Table 2.
Shear bond strength of the adhesive systems bonded to Biodentine and RetroMTA
Table 3.
Comparison of shear bond strength of the studied samples according to materials
| Materials | Adhesive Agents (MPa) | ||||
|---|---|---|---|---|---|
| CSE | AQ | ABU-SE | ABU-TE | p value | |
| BD | 3.68±1.01a | 2.06±0.57 | 6.87±2.55b | 4.33±1.24ab | 0.000* |
| RMTA | 1.86±0.75c | 0.39±0.26 | 4.71±2.35d | 2.86±1.56cd | 0.000* |
Kruskall-Wallis Test (* : p < 0.05), Mann-Whitney post hoc
a,b,c,d : same letters indicate no statistical differences between values in each group
BD : Biodentine, RMTA : RetroMTA, CSE : ClearfilTM SE bond, AQ : AQ bond plus, ABU-SE : All bond universal Self-etch mode, ABU-TE : All bond universal Total-etch mode
References
1. Gulati S, Shenoy VU, Margasahayam SV : Comparison of shear bond strength of resin-modified glass ionomer to conditioned and unconditioned mineral trioxide aggregate surface: An in vitro study. J Conserv Dent, 17:440-443, 2014.



2. Cantekin K : Bond strength of different restorative materials to light-curable mineral trioxide aggregate. J Clin Pediatr Dent, 39:143-148, 2015.


3. Torabinejad M, Chivian N : Clinical applications of mineral trioxide aggregate. J Endod, 25:197-205, 1999.


4. Antunes Bortoluzzi E, Juárez Broon N, Monteiro Bramante C, et al. : The use of a setting accelerator and its effect on pH and calcium ion release of mineral trioxide aggregate and white Portland cement. J Endod, 32:1194-1197, 2006.


5. Boutsioukis C, Noula G, Lambrianidis T : Ex vivo study of the efficiency of two techniques for the removal of mineral trioxide aggregate used as a root canal filling material. J Endod, 34:1239-1242, 2008.


6. About I : Biodentine: from biochemical and bioactive properties to clinical applications. G Ital Endod, 30:81-88, 2016.

7. Nowicka A, Lipski M, Buczkowska-Radlińska J, et al. : Response of human dental pulp capped with biodentine and mineral trioxide aggregate. J Endod, 39:743-747, 2013.


8. Cantekin K, Avci S : Evaluation of shear bond strength of two resin-based composites and glass ionomer cement to pure tricalcium silicate-based cement (Biodentine®). J Appl Oral Sci, 22:302-306, 2014.




9. Kang CM, Sun Y, Shin Y, et al. : A randomized controlled trial of various MTA materials for partial pulpotomy in permanent teeth. J Dent, 60:8-13, 2017.


10. Van Meerbeek B, De Munck J, Vanherle G, et al. : Buonocore memorial lecture. Oper Dent, 28:215-235, 2003.

11. Kim YI, Yoon JH, Lim BS, et al. : Microleakage and Microtensile Bond Strength Evaluation of the Various Generations of Dentin Bonding Agents. Korean J Dent Mater, 39:119-128, 2012.
12. Subramaniam P, Konde S, Mathew S, Sugnani S : Mineral trioxide aggregate as pulp capping agent for primary teeth pulpotomy : 2 year follow up study. J Clin Pediatr Dent, 33:311-314, 2009.


13. Altunsoy M, Tanrıver M, Ok E, Kucukyilmaz E : Shear bond strength of a self-adhering flowable composite and a flowable base composite to mineral trioxide aggregate, calcium-enriched mixture cement, and Biodentine. J Endod, 41:1691-1695, 2015.


14. Atabek D, Sillelioğlu H, Olmez A : Bond strength of adhesive systems to mineral trioxide aggregate with different time intervals. J Endod, 38:1288-1292, 2012.


15. Tunç ES, Sönmez IS, Bayrak S, Eğilmez T : The evaluation of bond strength of a composite and a compomer to white mineral trioxide aggregate with two different bonding systems. J Endod, 34:603-605, 2008.


16. Davidson CL, de Gee AJ, Feilzer A : The competition between the composite-dentin bond strength and the polymerization contraction stress. J Dent Res, 63:1396-1399, 1984.


17. Deepa VL, Dhamaraju B, Bollu IP, Balaji TS : Shear bond strength evaluation of resin composite bonded to three different liners : TheraCal LC, Biodentine, and resin-modified glass ionomer cement using universal adhesive: An in vitro study. J Conserv Dent, 19:166-170, 2016.



18. Ha WN, Bentz DP, Kahler B, Walsh LJ : D90: the strongest contributor to setting time in mineral trioxide aggregate and Portland cement. J Endod, 41:1146-1150, 2015.


19. Karadas M, Cantekin K, Duymuş ZY, et al. : Evaluation of the bond strength of different adhesive agents to a resinmodified calcium silicate material (TheraCal LC). Scanning, 38:403-411, 2016.


20. Shin JH, Jang JH, Park SH, Kim E : Effect of mineral trioxide aggregate surface treatments on morphology and bond strength to composite resin. J Endod, 40:1210-1216, 2014.


21. Yoshida Y, Nagakane K, Van Meerbeek B, et al. : Comparative study on adhesive performance of functional monomers. J Dent Res, 83:454-458, 2004.


22. Gandolfi MG, Taddei P, Prati C, et al. : Development of the foremost light-curable calcium-silicate MTA cement as root-end in oral surgery. Dent Mater, 27:134-157, 2011.


23. Jang JH, Lee MG, Kim DS, et al. : Comparative study of the dentin bond strength of a new universal adhesive. Dent Mater J, 35:606-612, 2016.


24. Bayrak S, Tunç ES, Saroğlu I, Eğilmez T : Shear bond strengths of different adhesive systems to white mineral trioxide aggregate. Dent Mater J, 28:62-67, 2009.


25. Kayahan MB, Nekoofar MH, Dummer PM, et al. : Effect of acid-etching procedure on selected physical properties of mineral trioxide aggregate. Int Endod J, 42:1004-1014, 2009.


26. Hashem DF, Foxton R, Banerjee A, et al. : The physical characteristics of resin composite-calcium silicate interface as part of a layered/laminate adhesive restoration. Dent Mater, 30:343-349, 2014.


27. Hanabusa M, Mine A, De Munck J, et al. : Bonding effectiveness of a new ‘multi-mode’ adhesive to enamel and dentine. J Dent, 40:475-484, 2012.


- TOOLS
-
METRICS

-
- 5 Crossref
- 0 Scopus
- 3,149 View
- 146 Download
- Related articles




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



