 |
 |
| J Korean Acad Pediatr Dent > Volume 48(2); 2021 > Article |
|
ņ┤łļĪØ
ņāüņĢäņ¦łĒśĢņä▒ļČĆņĀäņ”ØņØĆ ņāüņĢäņ¦ł ĒśĢņä▒ ņØ┤ņāüņØ┤ ņ┤łļלļÉśļŖö ņ£ĀņĀäņä▒ ņ¦łĒÖśņ£╝ļĪ£ ņāüņŚ╝ņāēņ▓┤ ņÜ░ņä▒ ĒśĢņ¦łņØä ļö░ļźĖļŗż. ņāüņĢäņ¦łĒśĢņä▒ļČĆņĀäņ”ØņØĆ ņ£Āņ╣śņÖĆ ņśüĻĄ¼ņ╣ś ļ¬©ļæÉ ņØ┤ĒÖśļÉśļ®░, ļŗżņ¢æĒĢ£ ņ╣śņĢä ļ│Ćņāē, ņāüņĢäņ¦ł ļ░Å ļ▓Ģļ×æņ¦ł ĒīīĻ┤┤, ņŗ¼ĒĢ£ ņ╣śņĢäļ¦łļ¬© ļō▒ņØś ņ×äņāüņåīĻ▓¼ņØä ļ│┤ņØĖļŗż. ļ░®ņé¼ņäĀĒĢÖņĀüņ£╝ļĪ£ ņ╣śņĢäļŖö Ļ░ĆļŖÉļŗżļ×Ć ņ╣śĻĘ╝Ļ│╝ ļæźĻĘĖļ¤░ ņ╣śĻ│╝ņØś ĒśĢĒā£ļź╝ ļ│┤ņØ┤Ļ│Ā ņ╣śņłśĻ░ĢņØĆ ņĀüĻ▒░ļéś ĒÅÉņćäļÉśņŚłļŗż. ņāüņĢäņ¦łĒśĢņä▒ļČĆņĀäņ”ØņØś ņ╣śļŻīļŖö ņČöĻ░ĆņĀüņØĖ ļ¦łļ¬©ļź╝ ļ░®ņ¦ĆĒĢśĻ│Ā ņłśņ¦ü Ļ│ĀĻ▓Į ĒÜīļ│ĄņØä ļ¬®Ēæ£ļĪ£ ĒĢ£ļŗż.
ļ│Ė ņ”ØļĪĆļŖö ņ╣śņĢäņØś ļ¦łļ¬©ņÖĆ ļ│ĆņāēņØä ņŻ╝ņåīļĪ£ ļé┤ņøÉĒĢ£ ņāüņĢäņ¦łĒśĢņä▒ļČĆņĀäņ”ØņØä ņ¦Ćļŗī ļé©ļ¦żņØś ņāüņØ┤ĒĢ£ 15ļģäĻ░äņØś ņןĻĖ░ ņśłĒøäļź╝ ļ│┤Ļ│ĀĒĢśĻ│Āņ×É ĒĢ£ļŗż. ļæÉ ĒÖśņ×ÉņŚÉņä£ ņ╣śļŻīĻ░£ņ×ģ ņŗ£ĻĖ░ņØś ņ░©ņØ┤ņŚÉ ļö░ļØ╝ ņāüņØ┤ĒĢ£ ņ╣śļŻīĻ│╝ņĀĢņØä ļ│╝ ņłś ņ׳ļŗż. ņ▓½ ļ▓łņ¦Ė ĒÖśņĢäļŖö ļīĆļČĆļČäņØś ļ│ĖņØĖ ņ╣śņĢäļź╝ ņé┤ļĀĖņ£╝ļéś, ļæÉ ļ▓łņ¦Ė ĒÖśņĢäļŖö ļ¬©ļōĀ ņ╣śņĢäļź╝ ļ░£ņ╣śĒĢśņśĆļŗż. ņØ┤ļŖö ņāüņĢäņ¦łĒśĢņä▒ļČĆņĀäņ”ØņØś ņĪ░ĻĖ░ ņ¦äļŗ© ļ░Å ņ╣śļŻīļ░®ļ▓Ģ Ļ▓░ņĀĢņŚÉ ļÅäņøĆņØ┤ ļÉĀ ņłś ņ׳ļŗż.
Abstract
Dentinogenesis imperfecta (DI) is a hereditary disorder of dentinal defect. It is generally inherited as a single autosomal dominant trait. DI usually affects both the primary and permanent dentition. Affected teeth have various types of discolorations, rapid destruction of the dentin, and severe attrition. In radiologic view, the affected teeth have bulbous crowns, short roots and narrow or closed pulp chambers. The treatment objective is to prevent additional attrition and recover the vertical dimension of occlusion.
The aim of this report was to present the long-term prognosis in 15 years in a pair of siblings. Both the patients had DI with tooth attrition and discoloration. Different treatment procedures were used, depending on the difference in the timing of intervention. The first patient saved most of his teeth. The second patient had all of her teeth extracted. This report could be helpful for early diagnosis and overall treatment of DI.
Dentinogenesis imperfecta (DI) is inherited as an autosomal dominant trait with high penetrance and a low mutation rate[1-3]. A mutation in the dentin sialophosphoprotein (DSPP) gene located on chromosome 4q21.3 has been reported as a cause of hereditary dentin defect[2,4]. Shields et al.[5] proposed three types of DI. DI type 1 is associated with osteogenesis imperfecta (OI)[5]. DI type 2 has essentially the same clinical, radiological and histological features as DI type 1 but without OI[5]. DI type 3 was first discovered in USA and is characterized by ŌĆ£shell teethŌĆØ of wide pulp cavity, severe attrition and discoloration[2,5].
In clinical examination, DI usually affects both the primary and permanent dentitions, characterized by the disturbed dentin formation[5]. The primary dentition appears more severely affected than the permanent dentition[6]. The color of the teeth varies from brown to blue and is sometimes described as gray, with an opalescent sheen[6]. The exposed dentin may undergo severe and rapid attrition[6]. Severe attrition may lead to a rapid decrease in the vertical dimension[7]. In radiologic view, the affected teeth are in the shape of slender roots and bulbous crowns; the pulp chambers are narrow or closed, and the root canal is obliterated and has a ribbon shape[5,8].
In previous studies, various approaches for treating patients with DI have been introduced. The choice of rehabilitation was based on the patientŌĆÖs age at the time of initial treatment and attrition severity[9]. In early primary dentition, severe attritions appeared immediately after the eruption[7]. Protection of the primary molars with stainless-steel crowns was generally necessary[7]. Some patients were left untreated until adolescence or adulthood and complete dentures were fitted when all the teeth were extracted[10]. Because root canal treatment of teeth with DI may cause problems because in most cases the root canals were narrow or absent[10]. The risk of root perforation is high, owing to the obliteration of the coronal parts of the root canals[11]. Pettiette et al.[12] proposed performing early root canal treatment before severe root canal obliteration occurs.
Intracoronal restorations may be acceptable in mild cases with low attrition[7]. In the restorative treatment of pediatric patients, the use of glass ionomers, that release fluoride and chemically bonds to tooth structure is recommended[13]. An acid etch technique followed by composite restoration is proposed as an alternative for the restoration of the anterior teeth[13,14]. In severe cases, an acrylic overlay denture, resting over the remnants of the crowns and roots of the primary dentition, has been used successfully[9].
Several studies have reported on cases of DI in patients with mixed dentition and early permanent dentition. Few reports have discussed long term prognosis and treatment outcomes after the completion of growth. This case report aimed to present the clinically different prognoses in siblings with DI who were followed up and treated at different times for 15 years.
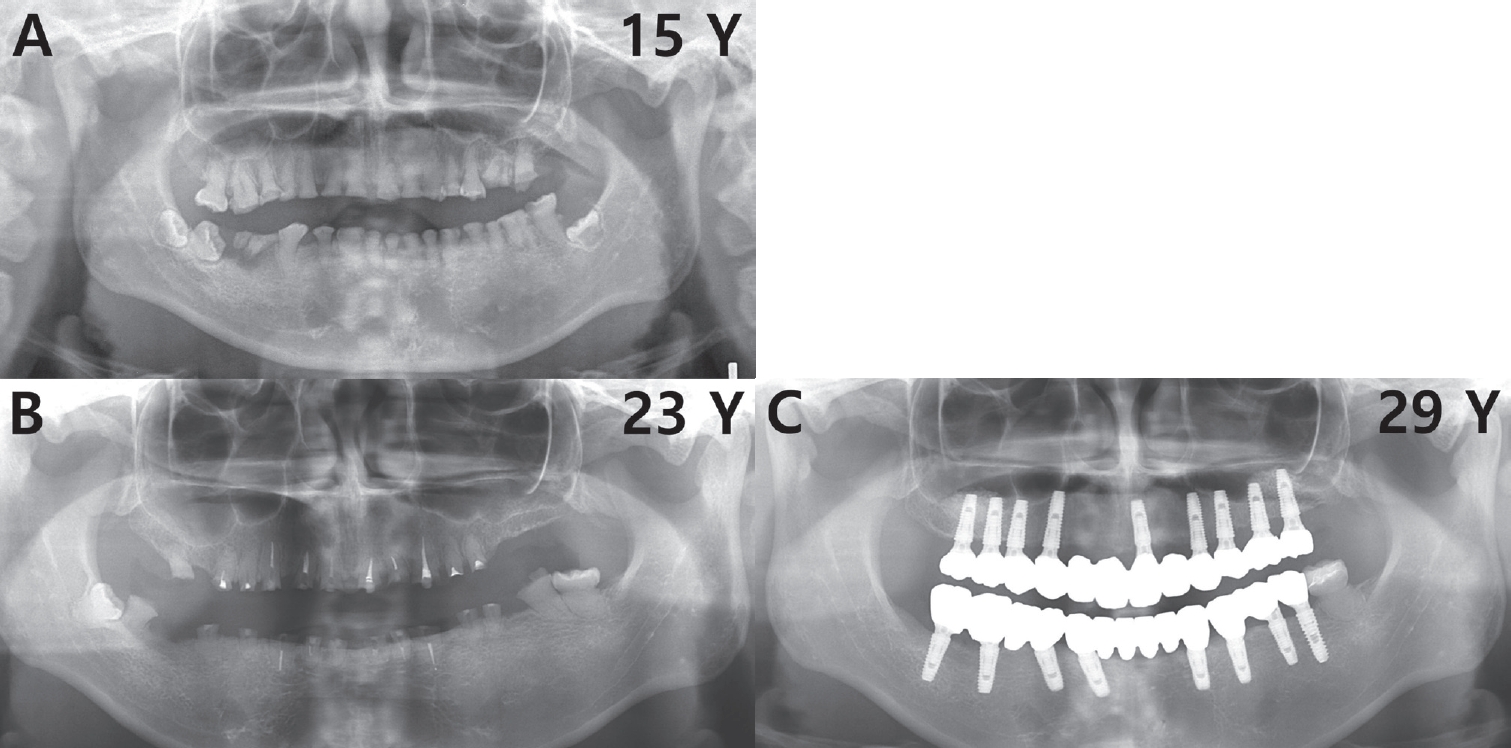
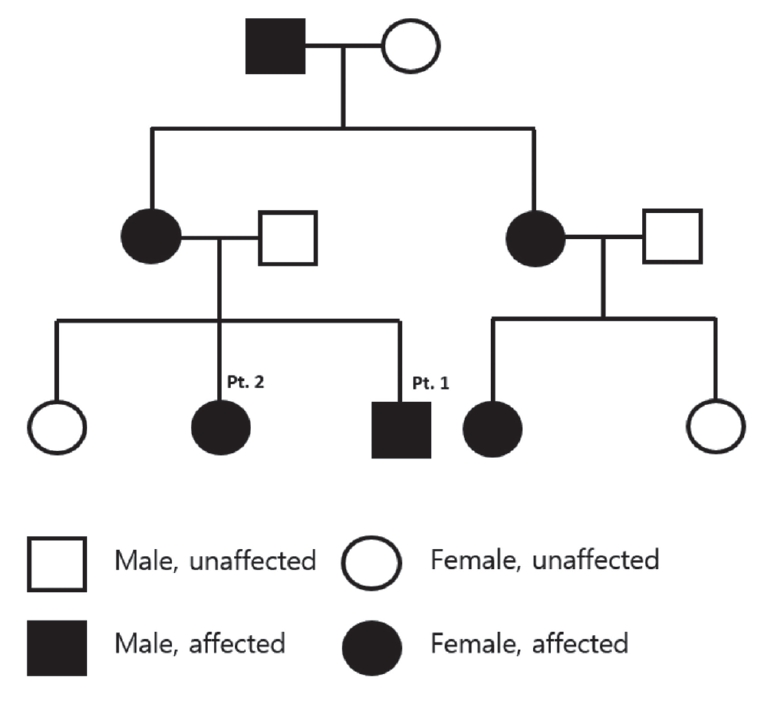
An 11 year-old boy and a 15 year-old girl, who were siblings, visited the Department of Pediatric Dentistry at Kyungpook Dental Hospital with worn and yellow-brown teeth. Both patients showed clinically severe tooth attrition and loss of vertical dimension. In panoramic view, obliteration of the pulp chamber and root canal, bulbous crowns with constricted cervical areas, and shortened thin roots were observed.
Based on these features, they were diagnosed with DI, and the results of a medical examination through an interview confirmed that this condition was inherited from their mother (Fig. 1). In the systemic disease examination, a tentative diagnosis of type II DI was established because osteogenesis imperfecta was not present.
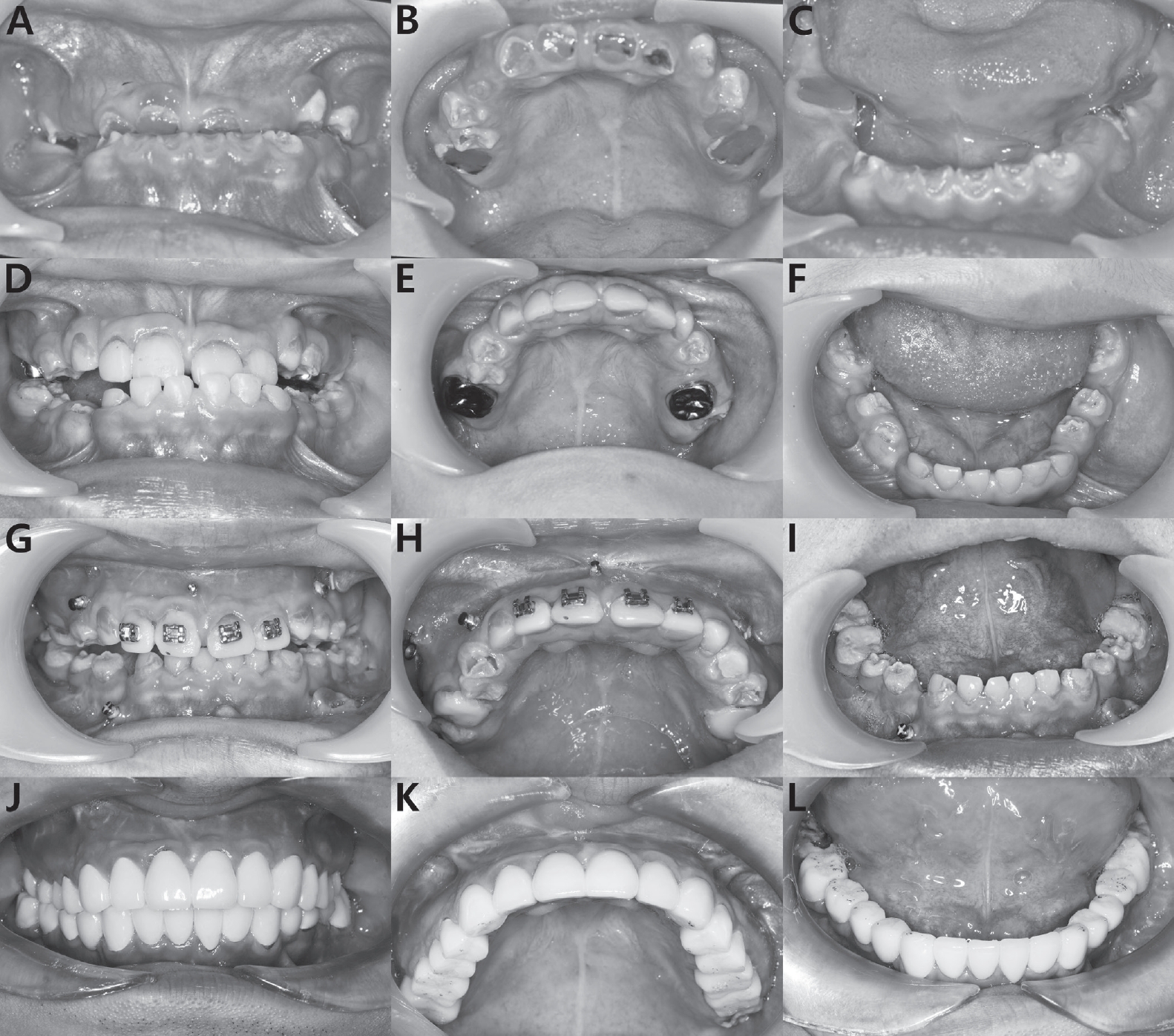
An 11 year-old male patient had a late mixed dentition at his first visit to the department of pediatric dentistry (Fig. 2A, 2B, 2C, 3A). Further, skeletal class III malocclusion was observed. For restorative and orthodontic treatment, the following treatment plan was established accordingly.
Until permanent dentition was completed, restorative treatment using composite resin and stainless-steel crowns could be performed, and orthognathic surgery could also be considered under the cooperation of the Orthodontics Department and Oral and Maxillofacial Surgery after growth completion. Then, through full-mouth rehabilitation in the prosthodontic department, the functional and esthetic aspect of the treatment plan could be completed.
In the actual treatment process, his maxillary and mandibular anterior teeth were first restored with composite resin to prevent further attrition. In the regular check-up, restoration of the maxillary anterior teeth fell out several times; therefore, composite resin restoration was performed repeatedly. Maxillary first molars were covered with stainless-steel crowns (Fig. 2D, 2E, 2F). The crowns were severely worn, and resin restoration could not be performed; therefore, both the mandibular first molars were extracted. Thereafter, to prevent further attrition, the second molars that erupted were restored with composite resin (Fig. 3B).
After completion of growth, the patient underwent orthodontic treatments and orthognathic surgery for the correction of class III malocclusion (Fig. 3C). At the end of the orthodontic treatment, anterior cross bite was corrected (Fig. 2G, 2H, 2I), and he was referred to the prosthodontic department for rehabilitation of entire dentition at the 11-year follow up.
Endodontic treatment is difficult owing to the obliterated root canal, and there is risk of root fracture. Prosthetic treatment could be performed without root canal treatment because the patient did not have any periapical lesion and pain (Fig. 3D). Using porcelain-fused-to-metal crowns and full zirconia crowns, all the teeth were rehabilitated with fixed prosthetics (Fig. 2J, 2K, 2L). Prosthetic rehabilitation fulfilled the esthetic and functional aspect of the treatment plan.
A 15 year-old female patient who was the older sister of Patient 1 had a permanent dentition when she first visited the department of pediatric dentistry (Fig. 4A, 4B, 4C). The enamel could not be observed easily owing to severe attrition, and periapical lesions were observed on the mandibular molars (Fig. 5A). Restorative treatment was not possible because the height of the crown owing to the exposed softened dentin was consistent with the gingival margin. Thus, prosthodontic treatment was planned via root canal treatment and crown lengthening while wearing overdenture until growth completion (Fig. 4D, 4E, 4F).
Even after a prolonged period of root canal treatment, closed root canals made further treatment impossible (Fig. 5B). Thus, when growth was completed, the remaining roots were extracted and the prosthetic restoration was performed via full-mouth implant treatment (Fig. 5C). The final prosthesis was finished with full zirconia crowns. The patient showed recovered vertical dimension and good esthetic outcome (Fig. 4G, 4H, and 4I).
DI is a hereditary abnormality that may show different clinical manifestations[15]. Severe cases show excessive and rapid attrition on both the primary and permanent teeth[15]. Mild cases show little or no attrition on the permanent teeth[15]. In both types, primary dentition is more severely affected by attrition than permanent dentition[8]. Abnormal dentinal structure might be the cause of enamel fracture, resulting from lower numbers, varied diameters, short, twisted, and irregularly distributed dentinal tubules[16,17]. Majorana et al.[18] declared that in DI-affected teeth, yellow-brown discoloration is more prevalent than gray discoloration. Both the patients showed yellow-brown discoloration, and the enamel of the tooth was destroyed from the incisal margin of the anterior tooth and from the occlusal surface of the posterior tooth. The loss of vertical dimension followed accordingly, and in the second case, which was more severely destroyed, the exposed soft dentin on the level of the gingival margin could be observed.
Restorative treatment for DI patients can be performed using composite resin or glass ionomer cement in the anterior tooth and stainless-steel crown in the posterior tooth[15]. Covering the permanent teeth as soon as they enter into occlusion is necessary to prevent attrition[19]. This treatment is long and complex. In the first case, the patient visited the hospital during mixed dentition; further, to prevent additional tooth attrition, stainless-steel crown and resin restorations were performed in the molars and incisors respectively. Patient collaboration and parent compliance are factors of success in restoration[19]. Many treatments and follow-ups were possible in this case over a long period because of good cooperation form the patients and their parents. The degree of cooperation during the treatment was high in Patient 1 who continued to visit the hospital regularly for check-ups even after the restorative treatment.
Despite complete pulpal obliteration, these periapical lesions seem to appear on the first molars[12,15]. Owing to complete obliteration, endodontic treatment has very poor prognosis, and most teeth with such radiolucencies need to be extracted[12,15]. Both cases showed shortened thin roots, and the pulp chamber and root canal were obliterated in the radiographic images. These features, make it difficult to complete the root canal treatment. In the second case, implant treatment was selected after the extraction because periapical lesions were also present.
The purpose of treatment in the permanent dentition stage, that begins when the maxillary growth is stable, is to establish esthetic appearance and efficient masticatory functions[8]. In cases of extreme attrition or in adolescence, overdentures are usually a treatment option[20]. Patient 2 initially visited the hospital during the permanent dentition; she wore an overdenture to recover masticatory function and for esthetic recovery. In fact, full coverage crowns are usually a preferred method of restoration for DI patients because such restorations protect the dental tissues from developing further dental defects[21]. In these cases, zirconia and porcelain crowns were used. These are favorable options because they are esthetical, have an accurate fit, and are biocompatible. A long-term prognostic observation is necessary for implant prostheses and dental prostheses for DI.
Generally, for DI the recommendation is to initiate treatment as early as possible[13,22]. Bouvier et al.[19] showed good results in the long-term prognosis with early treatment in DI patients. The initial objectives of treatment in primary dentition were to increase the vertical dimension of occlusion by crowning the primary molars, that would enable the permanent teeth to erupt without undergoing early attrition[19]. And Sapir et al.[8] also declared that it is essential that children with DI be admitted into an early treatment to halt attrition that causes functional disorders. Darendeliler-Kaba and Marechaux[10] reported that in growing children it was decided to maintain the teeth for as long as possible under an overdenture till the time a permanent prosthetic solution can be decided.
In this case report, in the first case, a mixed dentition was appeared and in the second case, a permanent dentition was appeared at the first visited. In the second case, the prosthetic treatment was completed in an edentulous state. In contrast, the patient in the first case was able to undergo restorative treatment, and prosthetic restoration was performed with mostly natural teeth. In both the cases, the treatment cost was high, the duration was long, and the final treatment was completed via prosthetic restoration. There is a significant difference between restoration via implants in the edentulous stage and restoration through maximum usage of oneŌĆÖs remaining teeth.
This is a case report of long-term observation of siblings with DI. It is possible to observe how the treatment is performed over a long period, and it can be good data for predicting the prognosis in DI patients and establishing a treatment plan for pediatric dentists who meet mainly during primary and early mixed dentition as the prediction of the prognosis.
One limitation of this case report is that there were no reports of early intervention and treatment observations in patients from the middle of the primary and mixed dentition. If patient were observed for a long time with early intervention with primary dentition, it would have enabled a better comparison. Various prognoses as per different starting points could benefit DI patients who need to be constantly exposed to long-term dental treatment. Further studies would be needed in the future aimed at determining the best timing to start treatment for DI patients.
According to the type, DI may cause a wide range of tooth attrition in a short time. In this case report, both the treatment periods were lengthy, and finally, prosthetic restoration was required. Different treatment results were obtained with the difference in the timing of intervention for the siblings. This supports the importance of early intervention in DI.
Fig┬Ā2.
(A, B, C) Initial intraoral photographs show loss of vertical dimension. (D, E, F) At the 4-year follow-up, Intraoral photograph shows resin restoration of the anterior teeth and stainless steel crown setting of the upper first molars. (G, H, I) At the 9-year follow-up, panoramic view shows orthognathic surgery history. (J, K, L) At the 15-year follow-up, final intraoral photographs show recovery of vertical dimension with a zirconia crown
Fig┬Ā3.
(A) Initi al panoramic view shows severe attrition
on mixed dentition. (B) At the 4-year follow-up, panoramic view shows resin restoration of the anterior teeth and stainless steel crowns setting of the upper first molars. (C) At the 9-year follow-up, panoramic view shows orthognathic surgery history and correction of class III malocclusion. (D) At the 15-year follow-up, panoramic view shows final prosthesis with porcelain fused metal crowns and full zirconia crowns.

Fig┬Ā4.
(A, B, C) Initial intraoral photographs show severe attrition on permanent dentition and loss of vertical dimension. (D, E, F) Intraoral photographs show wearing overdenture. (G, H, I) At the 14-year follow-up, final intraoral photographs show recovery of the vertical dimension with a zirconia crown.

Fig┬Ā5.
(A) Initial panoramic view shows severe attrition on permanent dentition and loss of vertical dimension. (B) At the 8-year follow-up, panoramic view shows complete obliteration of the pulp and shortened roots. (C) At the 14-year follow-up, final panoramic view shows 9 upper implants and 8 lower implants with zirconia crowns
References
1. Bhandari S, Pannu K : Dentinogenesis imperfecta: A review and case report of a family over four generations. Indian J Dent Res, 19:357-361, 2008.


3. Subramaniam P, Mathew S, Sugnani SN : Dentinogenesis imperfecta: a case report. J Indian Soc Pedod Prev Dent, 26:85-87, 2008.


5. Shields ED, Bixler D, el-Kafrawy AM : A proposal classification for heritable human dentin defects with a description of a new entity. Arch Oral Biol, 18:543-553, 1973.

6. Witkop CJ, Rao S : Inherited Defects in Tooth Structure. Birth Deffects Orig Aric Ser, 7:153-184, 1971.
7. Gibbard PD : The management of children and adolescents suffering from amelogenesis imperfecta and dentinogenesis imperfecta. Int J Orthod, 12:15-25, 1974.


8. Sapir S, Shapira J : Dentinogenesis imperfecta: An early strategy. Pediatr Dent, 23:232-237, 2001.

9. Moundouri-Andritsakis H, Kourtis SG, Andritsakis DP : Allceramic restorations for complete-mouth rehabilitation in dentinogenesis imperfecta: A case report. Quintessence Int, 33:656-660, 2002.

10. Darendeliler-Kaba A, Marechaux SC : Hereditary dentinogenesis imperfecta: A treatment program using an overdenture. J Dent Child, 59:273-276, 1992.
11. Soliman S, Meyer-Marcotty P, Krastl G, et al. : Treatment of an Adolescent Patient with Dentinogenesis Imperfecta Using Indirect Composite Restorations-A Case Report and Literature Review. J Adhes Dent, 20:345-354, 2018.

12. Pettiette MT, Wright JT, Trope M : Dentinogenesis imperfecta: Endodontic implications. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 86:733-737, 1998.


13. Ranta H, Lukinmaa PL, Waltimo J : Heritable dentin defects: Nosolgy, pathology and treatment. Am J Med Genet, 45:193-200, 1993.


14. Posnick WR : Treatment of hereditary opalescent dentin: report of case. J Dent Child, 43:46-48, 1976.
15. Bouvier D, Duprez JP, Morrier JJ, et al. : Strategies for rehabilitation in the treatment of dentinogenesis imperfecta in a child: A clinical report. J Prosthet Dent, 75:238-241, 1996.


16. Biria M, Abbas FM, Ahmadi R, et al. : Dentinogenesis imperfecta associated with osteogenesis imperfecta. J Dent Res, 9:489-494, 2012.
17. Seow WK : Developmental defects of enamel and dentine: challenges for basic science research and clinical management. Aust Dent J, 59:143-154, 2014.


18. Majorana A, Bardellini E, Favia G, et al. : Dentinogenesis imperfecta in children with osteogenesis imperfecta: a clinical and ultrastructural study. Int J Paediatr Dent, 20:112-118, 2010.


19. Bouvier D, Leheis B, Jean L, et al. : Dentinogenesis Imperfecta: Long-term Rehabilitation in a Child. J Dent Child, 75:192-196, 2008.
20. Joahi N, Parkash H : Oral rehabilitation in dentinogenesis imperfecta with overdentures: Case report. J Clin Pediatr Dent, 22:99-102, 1998.

21. Edelhoff D, Weber V, Jovanovic SA, et al. : IPS Empress 2 porcelain crowns and bridges. J Multidiscipl Collab Prosthodont, 2:64-66, 2002.
22. Wright JT : The diagnosis and treatment of dentinogenesis imperfecta and amelogenesis imperfecta. Hellenic Dent J, 2:17-24, 1992.
- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 779 View
- 123 Download
- ORCID iDs
-
Gimin Kim

https://orcid.org/0000-0002-2979-070XJaesik Lee

https://orcid.org/0000-0001-5514-4595 - Related articles



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



