Ⅳ. Discussion
In the treatment of the large carious lesions, the cavity bases can be used to reduce postoperative sensitivity and secondary caries[
1]. There are many characteristics required for the base materials. Sealing ability and compressive strength are one of them. In this study, the microleakages and compressive strength of 5 base materials were evaluated.
The marginal leakage is the precursor of secondary caries, staining of restoration, tooth discoloration, postoperative sensitivity, and pulpal pathology[
5]. So, it is important to have a good marginal seal for the longevity of restorative material, thereby reducing the marginal leakage[
5]. In this study, microleakages with 5 base materials was evaluated. In previous studies, BD exhibited less microleakage than conventional glass ionomer cement and MTA[
6,
7]. In this study, BD and WRPT showed the lowest microleakage and RLC showed the highest microleakage (
Table 3). And the BD and WRPT groups showed significantly less microleakage than the FLC and RLC groups (
p < 0.05). And the WMTA group showed significantly less microleakage than the RLC groups (
p < 0.05). The consistency and handling property of the mixed materials might be one of the factors that affect these results.
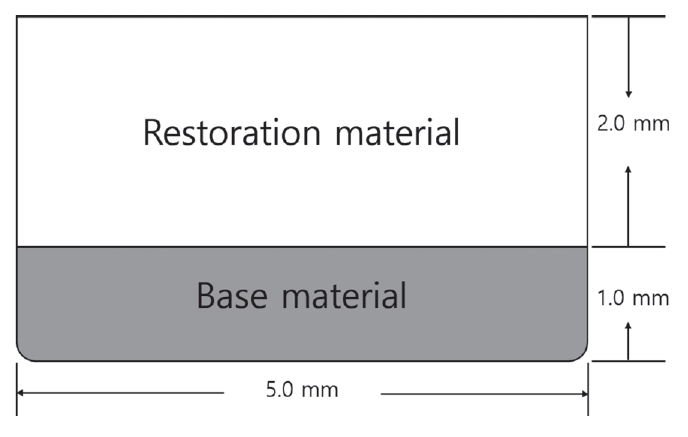
The handling property is important for the convenience of the procedure in pediatric dentistry. The materials used in this study had different handling properties. FLC showed a high viscosity and good handling property so that it was possible to condense the material with an instrument. RLC showed low viscosity and poor handling property; therefore dense restoration was difficult. WMTA showed a sandy consistency and initial looseness after mixing, revealing a poor handling property[
8]. BD can be well-aggregated and it easily adheres to the tooth surface; thus, it has a good handling property and sealing ability[
7,
9]. WRPT showed a good handling property so that it could be condensed using instruments during the filling process. In this study, BD and WRPT showed the lowest microleakage (
Table 3). BD can achieve constant properties through auto-mixing and it has excellent handling property and sealing ability[
7,
9]. Auto-mixing method is not under the control of the operator, and the mixing regime is standardized by the manufacturer so that the functional properties of the mixed materials are constant[
10,
11]. WRPT is a pre-mixed type material that shows constant physical properties, and it is provided in the form of a syringe. Therefore, it can be easily applied to the desired area[
6]. Moreover, WRPT has excellent handling property. Thus, it can be densely restored to the cavity. It is thought that these factors contributed in part to BD and WRPT showing the lowest microleakage. From the results of microleakage evaluation in the present study, it was confirmed that BD and WRPT were the base materials that have an excellent sealing ability. FLC showed significantly higher microleakage than BD and WRPT in this study (
p < 0.05). FLC might show a difference in physical properties each time because it is a power/liquid type material and is mixed by hand. The physical properties of materials that use a traditional hand-mixing method may vary depending on the skill of the operator and mixing environments[
11]. Also, because FLC is not available in syringe form, there is high possibility of the presence of voids inside the material during the filling process[
12]. RLC is an auto-mixing and syringe-type material. Therefore, it can achieve constant properties and is easy to apply to the cavity. But, it showed the hightest microleakage in this study (
Table 3). This result was attributed to the fact that RLC was difficult to condense in the cavity due to its low viscosity and poor handling property. The voids could have been present during the process of adjusting the base material to 1.0 mm height with a cotton pellet. This was supported by Nomoto
et al. [
10], who stated that a lowviscosity material encouraged more voids to be formed during mechanical mixing. From this result, it could be suggested that the material in the form of auto-mixing does not always show lower porosity and good properties. Therefore, when selecting a material, it is necessary to simultaneously consider other factors, such as the viscosity and handling property of the material and the environment in which the material is being used.
Products applied as a cavity bases require sufficient strength to withstand condensing stresses during filling of the restoration[
13]. Compressive strength is one of the main physical properties of base materials. When used as a base material, the cement should have the capacity to withstand masticatory stress[
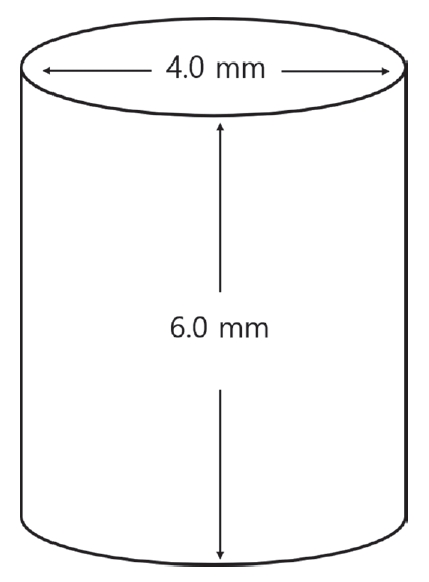
5]. In this study, FLC showed significantly higher compressive strength than the rest of the groups. No statistical significance was observed among the other groups (
Table 5,
6). According to the International Organization for Standardization (ISO) 3107, when zinc oxide eugenol is used as cavity bases, the compressive strength should be at least 25 MPa[
14]. In ISO 9917-1, the compressive strength of glass ionomer cement, used for a cavity base/lining material, is specified to be at least 50 MPa[
15]. In this compressive strength test, FLC had 189.04 ± 12.79 MPa and RLC had 64.14 ± 9.34 MPa, which satisfied the requirements. BD had a compressive strength of 57.04 ± 9.34 MPa, WMTA 53.58 ± 7.10 MPa, and WRPT 44.55 ± 6.55 MPa. Although there are no requirements presented in the international standard for calcium silicate-based materials, the experimental results satisfied the requirements as seen in the standards of ISO 3107 or ISO 9917-1[
14,
15]. Therefore, all materials in this study can be used as cavity bases. But, if the tooth receives large masticatory stress, such as a permanent molar, a base material with sufficiently high compressive strength would be more recommended[
5]. Thus, it can be suggested that if the treated tooth receives large masticatory stress, the material that showed higher compressive strength, such as FLC, is more recommended. In this study, FLC showed the highest compressive strength. The compressive strength of BD in this study was 57.04 ± 9.34 MPa, which was lower than the value reported in previous studies[
16]. It is presumed that there was a possibility for the existence of voids inside the specimen due to insufficient operator skills. It was reported that the compressive strength might differ due to the presence of the voids[
17]. Grech
et al. [
18] reported that BD had low fluid uptake, low setting time, and superior mechanical properties. Camilleri
et al. [
19] reported that BD is more dense and less porous than MTA. According to these results, BD could be also considered as a base material in areas requiring high strength.
Due to the characteristics of pediatric dentistry, it is important to shorten the operation time when treating patients. Therefore, when using the base materials, the materials that have a short setting time and make it possible to complete the whole procedure in a single appointment are recommended. Among the materials used in this study, RMGICs, which can be light-cured immediately, can be used for 1-visit treatment. WMTA has a long setting time, so it cannot be used for 1-visit treatment. BD and WRPT have been promoted as having relatively short setting times, each 12 minutes and 25 minutes, respectively, according to the manufacturers. Although BD and WRPT have relatively short setting times than WMTA, the setting times of these materials are not short enough to be used for a 1-visit treatment.
In the treatment of the teeth affected by extensive caries, cavity bases can be used to reduce postoperative sensitivity and secondary caries. When selecting the base material to be used, many factors, such as the sealing ability, biocompatibility, and physical properties, should be considered. At the same time, in pediatric patients, other factors, such as patient cooperation, the convenience of the procedure and visit times for treatment, should also be considered. In this study, when considering the ease of handling and microleakages of the materials, BD and WRPT showed good results. But, when considering the visit times for treatment and mechanical properties, FLC was more suitable than other materials.
From the findings of this study, it was found that BD and WRPT showed little microleakages and good handling properties as base materials. And it was found that FLC has a short setting time and large compressive strength. But there are many other things that should be considered when selecting a base material. The clinician should know the characteristics of the material and be able to select the appropriate material according to the situation.
This study has some limitations. First, this study would not completely reproduce the oral environment. In this study, WRPT was not cured within 25 minutes, the time indicated by the manufacturer. So, the final restoration was proceeded after 30 minutes. It is thought to be because the environment in which the material is cured is not the same as the clinical conditions. Second, the effect of the final restoration was not considered when evaluating the microleakages. The microleakage on the enamel may be the effect of the final restoration, not the base materials, but this was not considered in this study. Although the composite resin was restored in the form of a single bulk filling to minimize the effect of the final restoration, the effect of the final restoration on the microleakage evaluation was not completely controlled. Third, due to insufficient skills to prepare specimens for the compressive strength evaluation, the experimental results of BD were lower than those of previous studies. Fourth, only the microleakages and compressive strengths of the base materials were evaluated in this study. There are many other factors that should be considered for selecting materials, such as biocompatibility, solubility, and sealing ability. Further studies on other factors that should be considered for selecting materials are needed.












 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



