Introduction
Distalization of maxillary molars is often required in the non-extraction treatment of Angle Class II malocclusion with minimal to moderate crowding. This can be achieved with both orthodontic and orthopedic actions by exerting extraoral forces from headgear. However, treatment using headgear largely depends on patient cooperation and can require a long period of time due to the use of intermittent forces [
1]. Accordingly, various intraoral appliances for maxillary molar distalization have been developed to avoid the need for patient cooperation. In 1978, Blechman and Smiley [
2] introduced repelling magnets; in 1991, Gianelly et al. [
3] used superelastic nitinol coil springs on continuous arch wires; and in 1992, Hilgers [
4] developed the pendulum appliance while Jones and White devised the Jones jig appliance [
5]. In 1995, Karla [
6] created the K-loop; and in 1996, Carano and Testa [
7] invented the distal jet appliance.
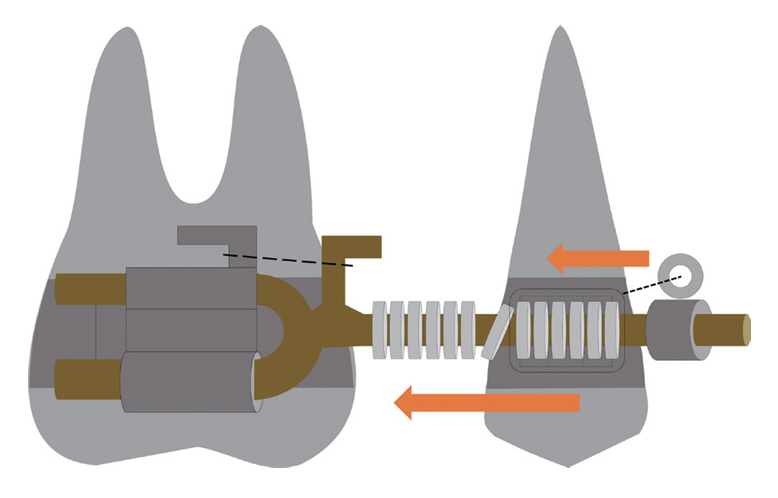
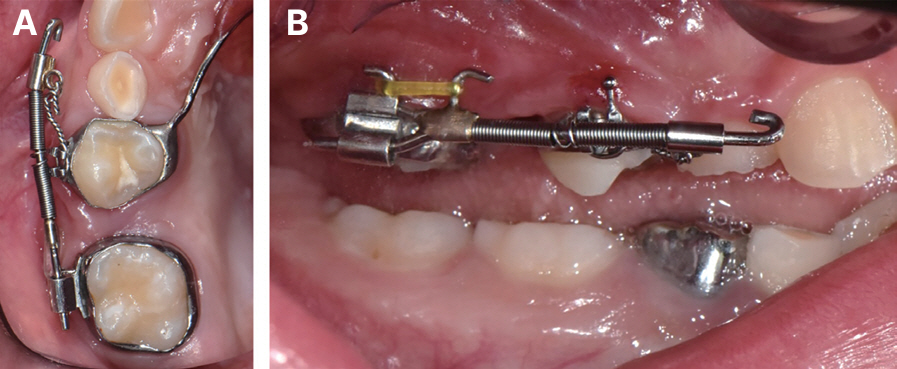
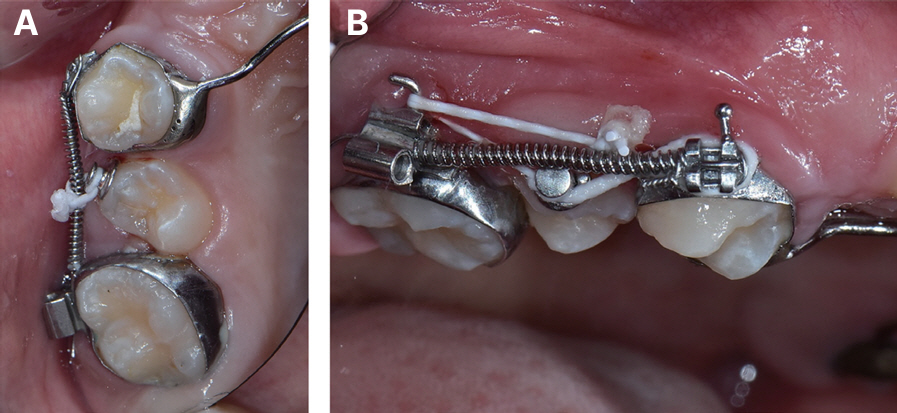
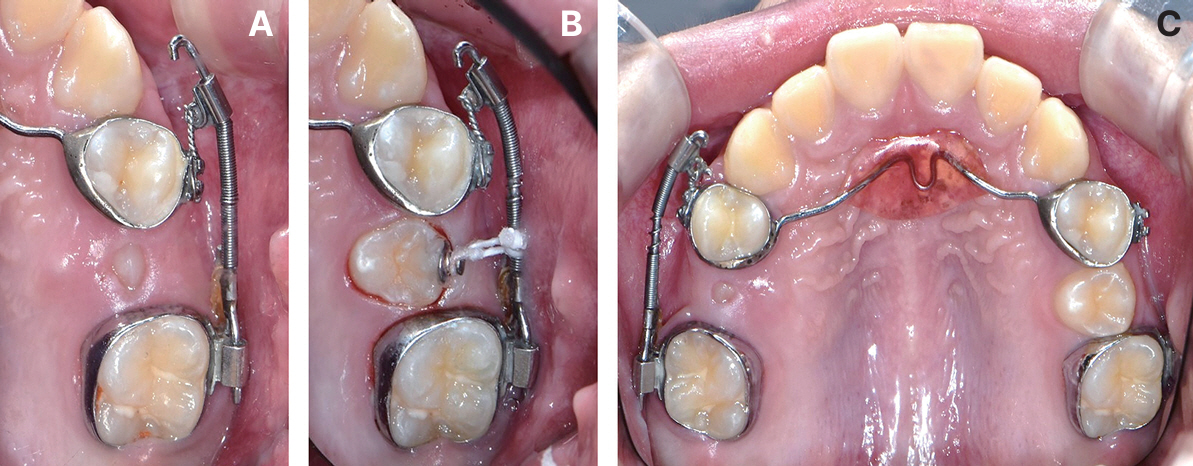
The Jones jig appliance is a combination of a sectional jig assembly and a modified Nance holding arch (NHA). The NHA serves as anchor that usually connects the premolar on the molar distalization side to the contralateral premolar or molar. The sectional jig assembly, which is the active part of the appliance, consists of a 0.030-inch stainless steel wire with a sliding nitinol coil spring and eyelet tube. The distal part of the sectional wire is inserted into a double-slotted tube on the molar to be distalized. The nitinol coil spring is guided over the wire mesial to the molar and compressed by the eyelet tube, which is guided over the wire mesial to the coil spring. The eyelet tube is tightly ligated with a stainless-steel wire to a bracket welded onto the buccal side of the premolar band (
Fig. 1). The jig assembly is activated every 4 weeks by compressing the coil spring from 1.0 - 5.0 mm on each activation [
5]. The maxillary molar is distalized at a rate of approximately 0.83 mm/month [
8], and the jig assembly is activated until Class I molar relationship is established.
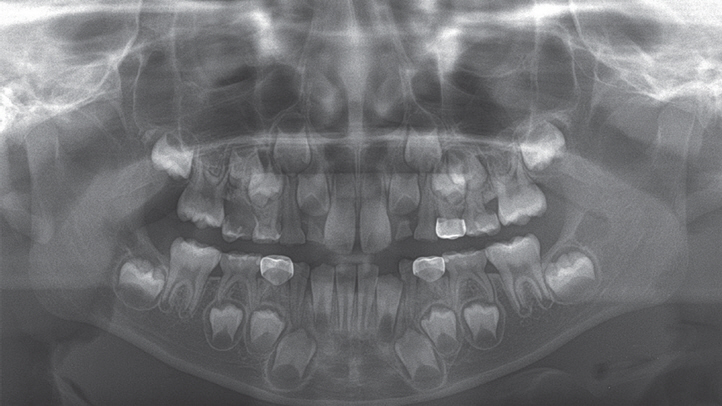
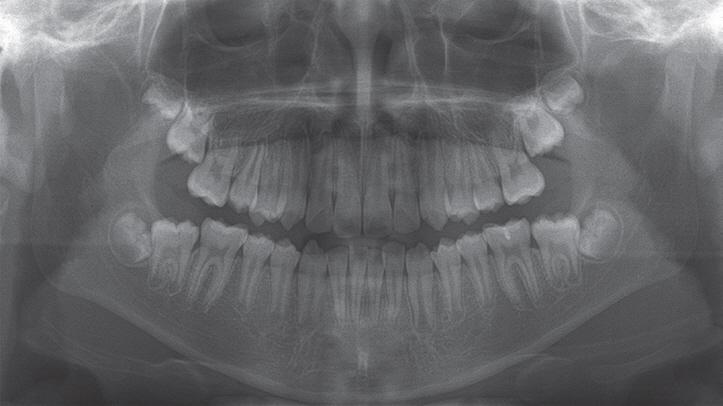
Premature loss of the primary maxillary second molar causes significant mesial movement and tilting of the adjacent first molar [
9]. Space loss occurs fastest and in the greatest amount when the primary second molar is extracted before the eruption of the first molar. If left untreated, eruption disturbances of the second premolar can occur, leading to further development of malocclusion. Thus, space problems due to early loss of the primary second molar must be resolved in a timely manner. The Jones jig appliance can be used to regain space lost by mesial encroachment of the maxillary first molar. This report describes two cases utilizing the Jones jig appliance to distalize the maxillary first molar into its original position.
Discussion
Eruption space loss for the maxillary second premolar (P2) due to early exfoliation of its predecessor is usually caused by mesial ectopic eruption of its adjacent first molar. This often occurs in the early mixed dentition period and can be related to various conditions such as cleft lip and palate, short maxilla, mesially inclined eruption pathway of the maxillary first molar (M1), overhanging crown margin of the adjacent primary second molar, and infraocclusion of the adjacent primary second molar [
10]. An M1 mesially encroaching into the roots of its adjacent primary second molar may self-correct in certain cases. However, spontaneous correction may not occur in children older than 8 years, in cases of severe root resorption of the primary second molar, or with severely inclined M1 [
11-
13]. In both of our cases, early exfoliation of the primary second molars was caused by mesial encroachment of their adjacent M1s. In the first case, however, only the right primary second molar exfoliated, while the left one was maintained until its normal exfoliation stage.
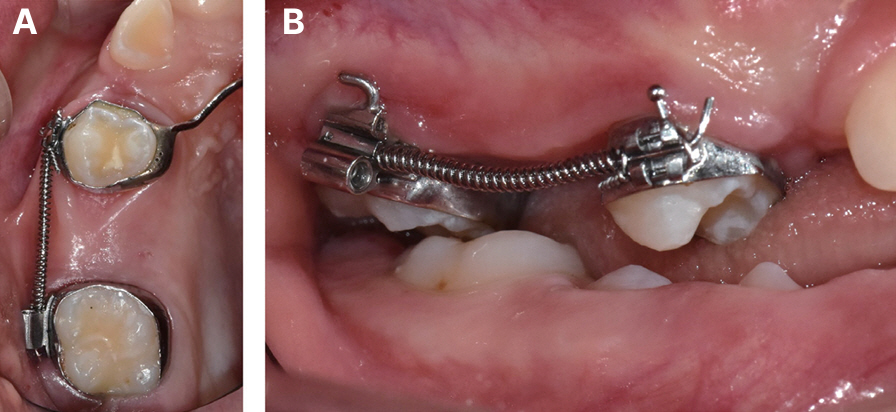
Appropriate intervention in a patient with space loss due to mesial migration of M1 should be performed to prevent eruption disturbances of P2. If the primary second molar remains stable for use as an anchor tooth, early distalization of its adjacent M1 can be simply conducted using the Halterman appliance. Unfortunately, if the primary molar becomes mobile or exfoliates prematurely due to severe root resorption, distalization of M1 should be considered after the eruption of P1. The Jones jig appliance can efficiently and effectively distalize M1 during the late mixed dentition period through continuous force applied by an activated coil spring.
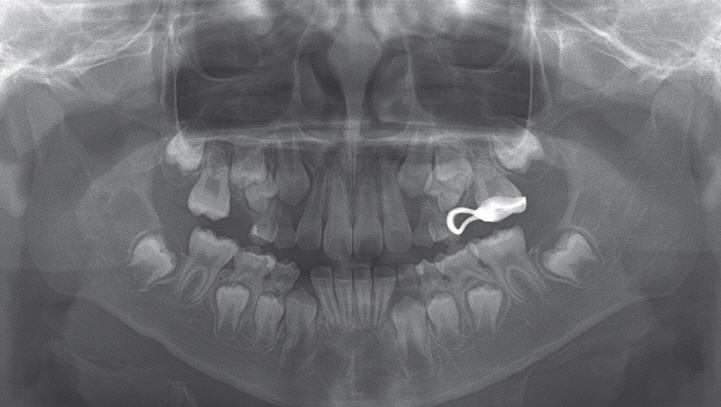
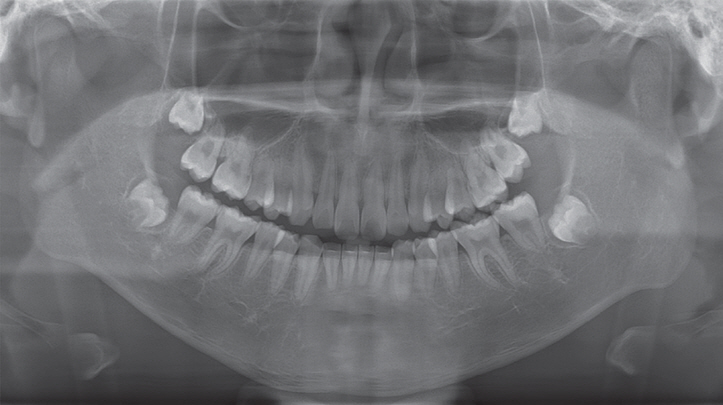
The movement rate of M1 is affected by the type and timing of movement. Movement is faster when the molars are distally tipped than when they are bodily moved. In our cases, distalization of M1 consisted of both distal tipping and bodily movement. The amount of distal tipping could be inferred by measuring the angular change of M1 in panoramic radiographs. Both cases showed distal tipping of M1 to a certain degree, but were not large enough to cause any eruption disturbances of the adjacent maxillary second molars (M2). This is shown in a panoramic radiograph taken after the eruption of M2 in our second case (
Fig. 16). It is recommended to apply light and continuous force when using the Jones jig appliance to minimize the amount of distal tipping.
Faster movement also occurs before the eruption of M2 [
14]. Distalization before the eruption of M2 results in more efficient movement of M1 and less anchorage loss than that after the eruption of M2 [
14,
15]. In another study comparing the distalization of M1 depending on the M2 eruption stage, distal movement of M1 mostly occurred in a bodily fashion when M2 was erupted, while distal tipping was more pronounced when distalization was performed before the eruption of M2. Distalization of M1 before the eruption of M2 was recommended since longer treatment times and heavier forces were needed after the eruption of M2 [
16]. Although Bussick and Mc-Namara Jr [
17] did not find any significant differences between the movement rate of M1 before and after the eruption of M2, they pointed out that a smaller increase in lower facial height and a smaller decrease in overbite were prevalent when distalization was performed before the eruption of M2. These studies, however, used nitinol coils or the pendulum appliance for molar distalization. Our literature search yielded few studies on the effect of the M2 eruption stage on the distal movement of M1 when using the Jones jig appliance.
The Jones jig appliance has several advantages over other intraoral distalizing appliances. One of them is that this appliance can aid in the alignment of the palatally erupted P2 [
18]. In both of our cases, P2 erupted palatally even though sufficient eruption space was established. With other molar distalizing appliances, such as the pendulum appliance, distal jet, or the Keles slider [
19], an additional appliance would be needed to align the palatally erupted P2. A severely palatally positioned P2 can cause crossbite, which leads to extrusion and deep overbite of P2. The development of a crossbite takes more effort to correct, so simple intervention during the eruption stage of P2 is a key benefit of this appliance. However, in some cases, P2 can erupt buccally, as reported in certain literature [
20]. In these cases, the Jones jig appliance might disturb the eruption of P2. A cone beam computed tomography image would therefore be necessary to determine the buccolingual position of P2 and the appropriate type of intraoral distalizing appliance.
Another virtue of the Jones jig appliance is that both distal tipping and buccolingual rotation are reduced, since the round and edgewise wires of the distal part of the assembly fit tightly into the tube of M1 (
Fig. 1). This aids in the bodily movement of M1, reducing relapse and the time needed for stabilizing the altered position of M1 [
8]. In our cases, although not much concern was put about retention after treatment, the corrected positions of P2 and M1 were well-maintained.
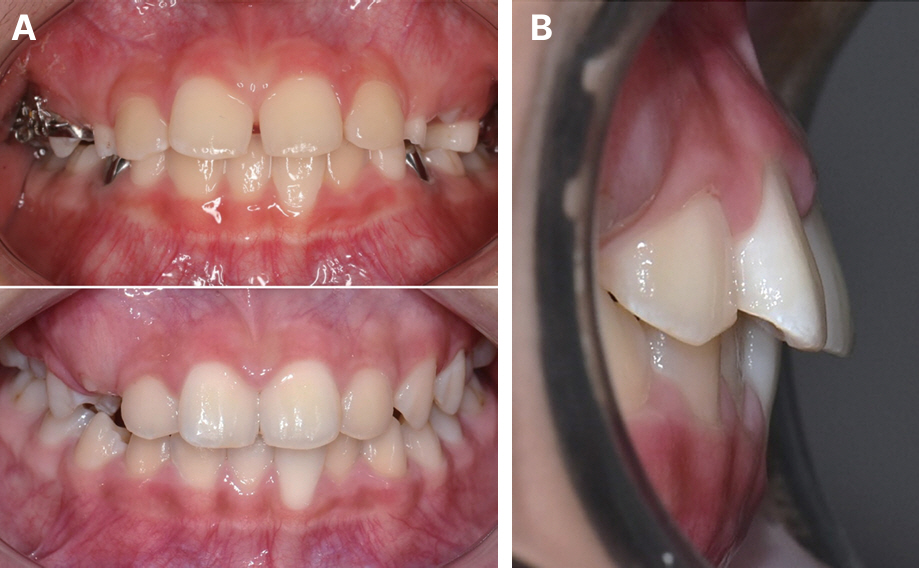
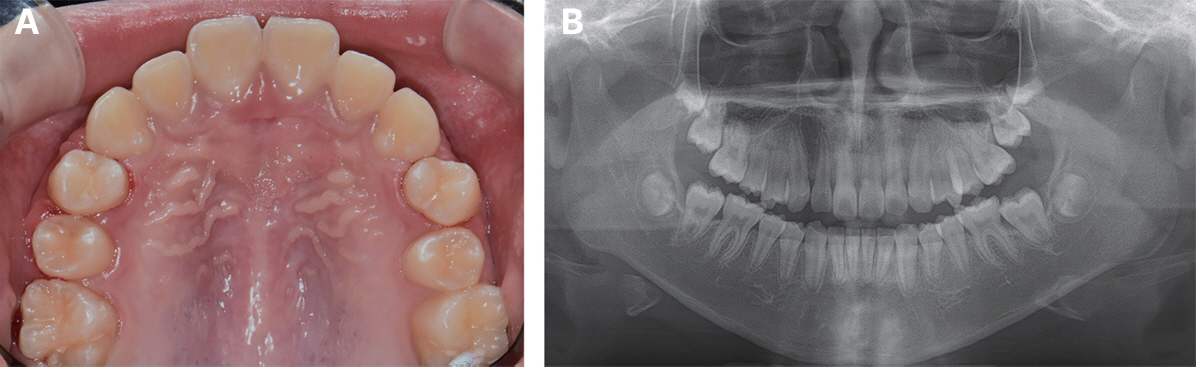
A characteristic feature of patients whose primary maxillary second molar has been exfoliated earlier than its normal exfoliation stage is that the adjacent M1 rotates mesio-palatally around its palatal root. This can be noticed in the first case before treatment (
Fig. 4). Since the line of action lies buccal to the center of resistance, M1 is rotated disto-buccally during distalization [
21]. This is one of the differentiated advantages of the Jones jig appliance over palatally acting distalizing appliances such as the pendulum.
Clear aligners have several advantages over conventional intraoral distalizing methods, including the Jones jig appliance. M1 can be distalized up to 2.0 - 3.0 mm without causing significant distal tipping [
22]. Also, clear aligners provide better control of the occlusal vertical dimension, while an increase in lower facial height is present when using the Jones jig appliance [
23]. Despite these advantages, we recommend using the Jones jig appliance over clear aligners for two reasons. 1) The treatment effect when using clear aligners highly depends on patient cooperation. 2) The amount of distalization required to create space for the eruption of P2 exceeds the normal range created by clear aligners.
Loss of anchorage is of main concern when using intraoral distalizing appliances. This manifests as mesial movement of P1 and protrusion and extrusion of the upper incisors, causing an increase in overjet. A superimposition image of the pre-treatment and post-treatment lateral cephalometric radiographs is essential to accurately compare the positional and angular changes of the premolars and incisors. Unfortunately, we did not take any lateral cephalometric radiographs of the patients. Instead, some post-treatment intraoral photographs showed that protrusion and extrusion of the incisors were minimal (
Fig. 9).
Jones and White [
5] reported no anchorage loss when using the Jones jig appliance, while Gulati et al. [
8] reported 1.05 ± 0.87 mm mesial movement of P1 and 1.10 ± 0.83 mm increase in overjet. Brickman et al. [
24] showed mesial movement of 2.0 mm and mesial tipping of 4.76o of P1. However, overjet increase and incisor labioversion were not as severe as those of other intraoral distalizing appliances, such as repelling magnets, nitinol coil springs, or the pendulum appliance. Conflicting results were shown in another study in which mesial tipping was greater when using the Jones jig appliance [
25], and a separate analysis of tooth movement when using the Jones jig appliance revealed that only 46% of the space created between M1 and P2 was due to distalization of M1 [
26]. In the latter study, however, M1 and M2 were simultaneously distalized, which could have contributed to greater anchorage loss.
The resistance to anchorage loss depends on several factors, such as distalization force [
8], the size and number of teeth incorporated in the anchorage unit [
25], the lack or inconsistency of contact points between spaced or severely crowded anterior teeth, and the shape of the palatal vault [
26]. In cases where there are insufficient teeth to incorporate into the anchorage unit, miniscrews implanted in the anterior paramedian region can be used to reinforce anchorage [
27]. The use of J-hook headgear or Class II elastics has been proposed [
24] but would require patient cooperation, negating the advantage of intraoral appliances.
Temporary anchorage devices (TADs) provide absolute anchorage and can thus minimize unwanted tooth movements. According to a systematic review, inter-radicular TADs result in less distal tipping but also less amount of distalization. Meanwhile, distalization using palatal TAD-supported appliances showed greater distal tipping [
28]. Depending on our clinical experience, children of school age lack bone quality for stability of TADs. Thus, using TADs over the Jones jig appliance has few advantages for molar distalization in the mixed dentition period.
When using the Jones jig appliance, it may be beneficial to position the double-slotted tube of M1 gingivally to minimize distal tipping. Since the center of resistance is located near the trifurcation of the root, a shorter distance to the line of action will cause lesser distal tipping of M1 [
8]. Shetty et al. [
29] pointed out that patients should be told to follow up for breakage of the ligature wire connecting the eyelet tube to the bracket on P1. A broken ligature wire is not easily detectable by patients, and repeated break-offs might cause relapse, extending treatment time. This was prevented using a 0.014-inch Kobayashi wire, which is usually used with up-and-down elastics during the finishing stage of fixed orthodontic treatment. In neither of our cases did the patient present with a broken ligature wire.



















 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



