Ⅲ. Discussion
MIM was first termed by Lee et al.[
1] in the case reports of 12 patients in 2014. Since 2014 when the malformation was first defined, cases of MIM had been reported along with the patients’ medical backgrounds. Majority of the patients had been hospitalized or treated due to premature birth, meningitis or brain-related diseases within 1 - 2 years after birth[
1,
4,
8]. The two girls presented in this study were diagnosed with neonatal jaundice. Jaundice features yellow discoloration of the sclera and skin, which is caused by an increase in serum bilirubin levels resulting in accumulation of bilirubin in the tissues[
9]. High levels of bilirubin could cause acute bilirubin toxicity and permanent brain damage[
9]. Elevated serum levels of bilirubin during the dental development period could cause green discoloration in teeth[
10]. Since jaundice is a condition that can affect the brain and dentition, neonatal jaundice seems in accordance with the medical issues which many MIM-affected patients have had. Neonatal jaundice the 2 patients had is not a rare systemic condition that could be present up to 80% among premature babies[
9,
11]. Jaundice in MIM affected patients was reported in previous case reports[
4,
8,
12]. It has yet to be determined how jaundice and tooth malformation are interrelated. According to Centers for Disease Control and Prevention (U.S. Department of Health & Human Sciences, October 30, 2020)[
13], preterm birth is when a baby is born before 37 weeks of pregnancy have been completed. Two patients in this study were born 2 weeks ahead of their estimated due dates. This was not severely premature condition considering that a full-term pregnancy is 40 weeks. There might be as yet unknown mechanism that led to MIM in spite of relatively mild medical histories.
Tooth root formation initiates after completion of tooth crown formation[
14]. Crown completion of mandibular first permanent molars was accomplished around 3.51 and 3.69 years old in boys and girls respectively[
15]. Approximate timing of initial root formation of mandibular first permanent molars was 4.17 and 3.65 years old in boys and girls respectively[
15]. Based on the facts above, the timing does not seem to explain that early-life medical events or interventions may be linked to the etiology of MIM. There should be complicated and delicate factors or mechanisms underlying molar root and incisor crown formation that have not been explored. Hormonal changes or medication was one of the possible causal factors associated with a systemic disease[
1,
3]. There is another well-known molar-incisor related dental anomaly, molar-incisor-hypomineralization (MIH). MIH is observations of hypomineralized enamel surface on one or more permanent first molars and some of permanent incisors[
16,
17]. While the aspects of the two anomalies are totally different from each other, both MIM and MIH show malformations on the permanent first molars and permanent incisors. It is assumed that the tooth formation periods of these teeth might be interrelated.
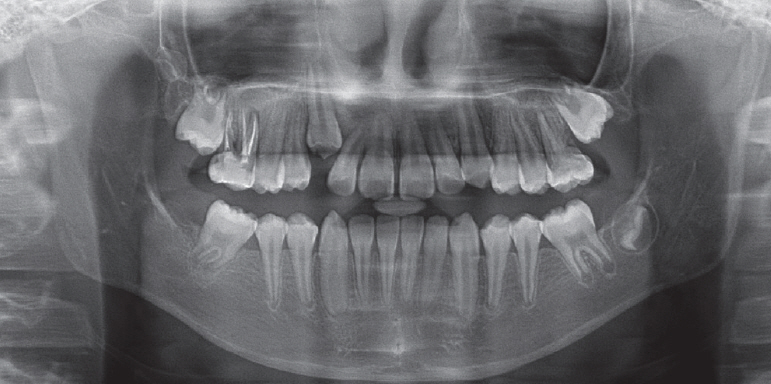
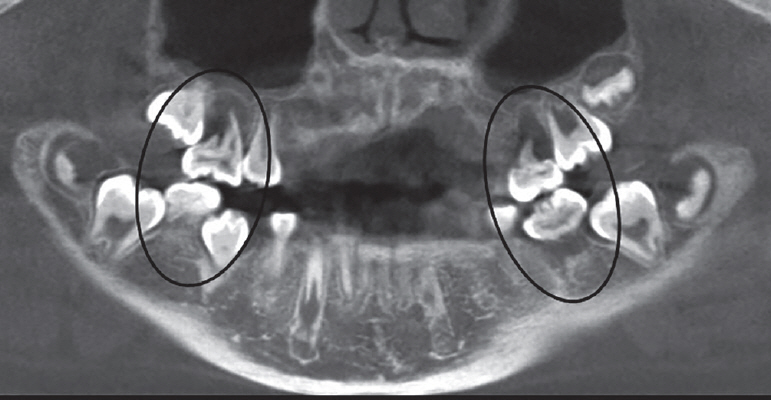
Abscess caused by periodontal inflammation, gingival swelling, periapical bone resorption and severe pain are typical clinical findings of MIM-affected patients. Witt et al.[
2] detected ectopic mineralized plates at the cemento-enamel junction (CEJ) level from the extracted molars, and named a cervical mineralized diaphragm (CMD). There were many soft tissue canals interspersed inside CMD and transmissions between CMD and the root furcation[
1,
2]. In Lee et al.[
3] microscopic analysis, 3 layers were marked in the pulpal floor; upper, middle, and lower. A higher radiopacity, amorphous hard tissues and hyperactive cells were detected in the middle pulpal floor (MPF). These structures could be potential paths of pulp exposure and bacterial infection. This results in periodontal infection, which could eventually infect the pulp. If the symptoms were untreated, it would cause severe alveolar bone resorption and unfavorable prognosis of the affected tooth. In this respect, making efforts to maintain good periodontal health seems crucial for MIM-affected patients. Prophylactic measures would be regular dental check-ups, scaling and mindful care of oral hygiene including flossing at home.
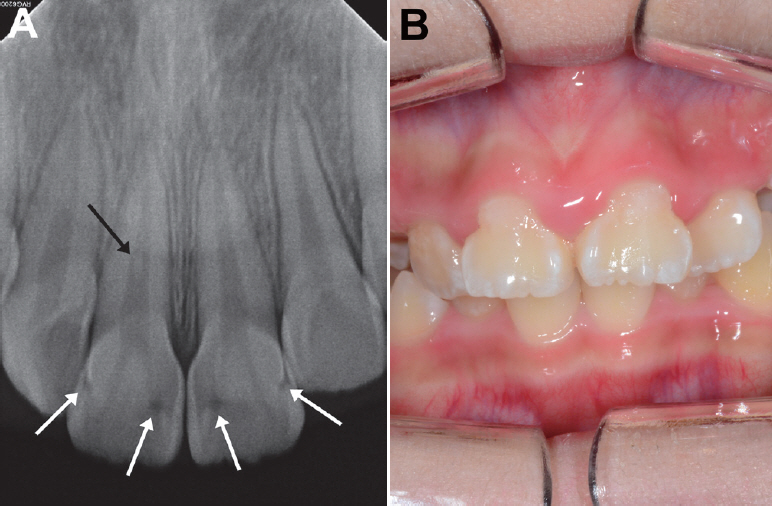
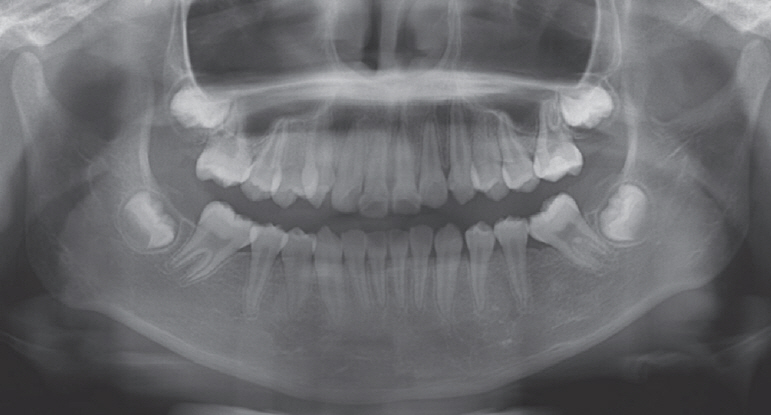
The first patient was misdiagnosed with DD type Ⅰ at first visit. DD type Ⅰ is an autosomal hereditary disturbance affecting both deciduous and permanent teeth in the entire dentition[
18-
20]. DD type Ⅰ-affected teeth clinically look normal in shape and color, but the roots are short with a constricted pulp chamber that is parallel with CEJ[
21]. MIM-affected teeth are mainly limited to permanent first molars, primary second molars and permanent maxillary central incisors. In a recent paper, affected permanent and deciduous canines were additionally reported[
4]. One of the important microscopic features of MIM that is distinguished from DD type Ⅰ is the existence of CMD or MPF[
2,
3].
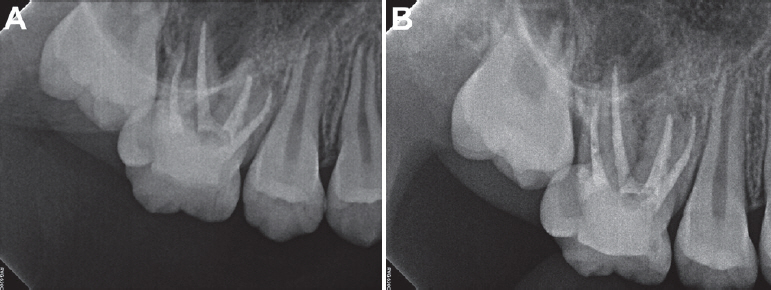
In case 1, the decision to wait and see for the right maxillary first permanent molar led to good results for the patient. Even though there was periapical radiolucency on the tooth, no clinical symptoms were present on the 2-year follow-up. Regular check-ups should be performed on the molar with a notification of the possibility of tooth extraction when the condition becomes worse. If the right permanent first molar would have to be removed, the second permanent molar could be guided to the first molar position. Some of the extraction space could be used to level the canine, since space did not seem enough for the right canine to be erupted. Both right maxillary and mandibular third molars were not observed on the radiograph at the time. Dental implants on both maxillary and mandibular second permanent molar positions may be needed for a better function of occlusion on the right posterior side. If the right maxillary permanent first molar is retained for a period of time with the maxillary second permanent molar being erupted, the second permanent molar may overerupt due to the absence of the opposing tooth. Splinting the second permanent molar with the adjacent teeth or an orthodontic appliance may be needed to prevent the molar from overerupting. Meanwhile, if the second permanent molar being erupted is locked under the distal contour of the MIM-affected first permanent molar, inserting a separator or using appliances such as Halterman would be considered. Comprehensive space management should be planed until a dental implant is implanted or another replacement is placed on the right mandibular second permanent molar position.
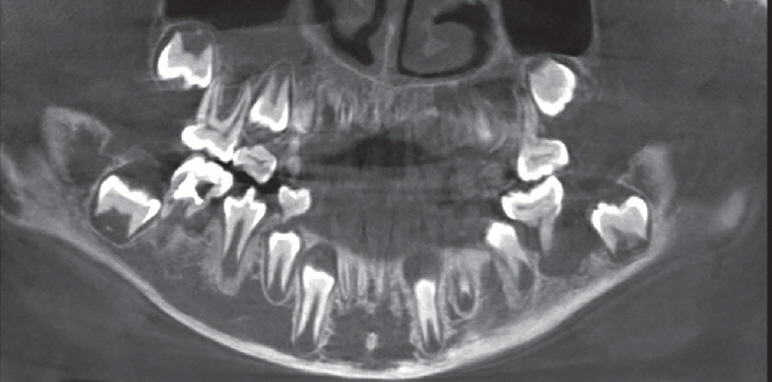
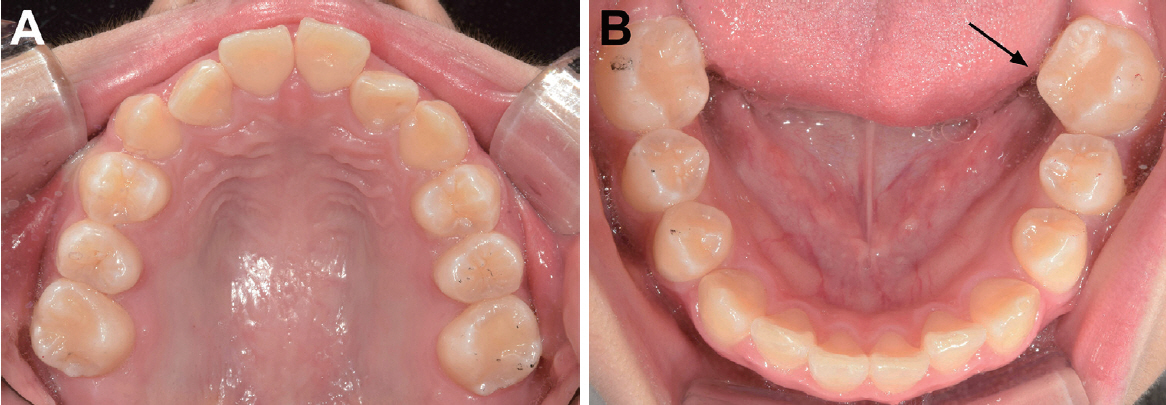
In case 2, the 4 permanent first molars were extracted without consideration of root canal treatment unlike case 1. The second permanent molars favorably erupted shifting to mesial and replaced the first molars. Kim et al.[
22] reported a similar case in which the mandibular permanent first molars were removed due to MIM and the extraction sites were closed through eruption of the second permanent molars. In our cases, the dental developmental stage of the permanent second molars corresponded to stage E in case 1 and stage F in case 2 (Demirjian’s method)[
6]. The ideal stage of development was stage E at the time of first permanent molars extraction[
6,
7]. Although 92% of maxillary extractions demonstrated complete space closure irrespective of second permanent molars development stage, only 66% of mandibular first permanent molars extracted at second permanent molars stage E showed complete space closure[
7]. The ideal extraction timing of first permanent molars has not been clearly decided. Late removal of the first permanent molar would increase the risk of mesial tipping of the second permanent molar and result in spaces adjacent to the extracted region[
23,
24]. Early removal would cause a distal drifting or rotation of the second premolar, which could occupy the space for the second permanent molar to erupt[
23,
24]. Eichenberger et al.[
25] researched the timing of extraction of permanent first molars to minimize clinical complications such as remaining gaps adjacent to the extracted region, tilting or rotation of the permanent second molars. The authors concluded that extraction should be performed between the ages of 8 and 11.5 for mandibular first permanent molars, whereas no solid conclusions were drawn concerning the maxillary first permanent molars[
23,
25]. When considering extraction of the first permanent molars, extraction in the maxilla is thought to be relatively free from clinical complications than in the mandible. The extraction of the first permanent molar should be performed at the right timing for successful eruption of the second permanent molar.
Mesial inclination of the second permanent molars seemed inevitable in our cases, especially in case 2. At the time of first permanent molar extraction, roots of the mandibular second permanent molars were more developed in case 2 than in case 1. The root length was less than the crown height in case 1, while the root length was equal to or longer than the crown height in case 2. The second molars of case 2 were almost supraosseous, whereas the ones of case 1 were intraosseous. These developmental conditions of the second permanent molars at the time of first molar extraction would be possible factors affecting their eruption in the future. Although space closure was fulfilled in both cases, the second permanent molar eruption was more favorable in case 1 than in case 2. Crown rotation was observed on the left mandibular second permanent molar in case 2. Mesially inclined and rotated second permanent molars might be corrected by the aid of orthodontic forces. Regular check-ups are needed to observe the progress of third molars eruption and their functional occlusion within the dentition.
MIM is now a dental anomaly with accumulated case descriptions. Brusevold et al.[
5] cautiously speculated that prevalence of MIM could increase because newborns with medical issues previously mentioned, who might have not made it to life in the past, have been well treated and survived thanks to the development of health care. Clinicians should be aware of characteristics of MIM and be able to detect, diagnose and provide appropriate treatments. Since treatment guidelines for MIM-affected children have not been clearly established, whether to preserve or extract the affected molar is a difficult decision. Enforced molar extractions are performed when tooth prognosis is poor due to extensive caries or severe MIH[
23,
24]. Depending on the dentition stage of the affected child and the level of MIH severity, treatment plans would vary from preventative cares, restoration, endodontic treatment to extraction[
24]. For MIM-affected children, if short, slender, rudimentary roots of permanent first molars are examined on radiographs, possible symptoms of MIM should be explained to the parents and the patients with emphasis of maintaining good periodontal health. Moreover, prophylactic oral hygiene care including flossing and scaling and regular check-ups should be stressed to prevent late detection of inflammation. Once pain is present and continuous, taking CBCT is recommended to scrutinize the anatomy of the affected tooth. If the symptomatic region seems endodontic-origin and the canal shapes are endodontically approachable, root canal treatment may be indicated[
26]. Successful root canal treatment may ensure a good prognosis of the affected tooth[
27,
28]. When all canals were negotiated and filled, and vertical bone loss from the furcation was less than one third, a favorable prognosis was observed until 2 years post-treatment[
28]. In Kim et al.[
4] study, MIM-affected mandibular first permanent molars with endodontic-periodontal lesion were retained for 5 years after root canal treatment. If inflammation is severe and periodontal bone loss is destructive, extraction of the malformed molar would be the last choice. Before extraction, clinicians should examine the developmental stage of the second permanent molars, the existence of third molar tooth germs and the patient’s age. Depending on the conditions, molar extraction could be awaited until the right timing. The recommended timing for the first molar extraction was when a calcified point on the root bifurcation of the second permanent molar would appear on radiographs[
23]. A beginning of calcification of third molars would be observed between 7 and 9 years old[
29]. Depending on the time of extraction, favorable closure of extraction sites could be accomplished or not. In some cases, space management should be considered.













 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



